Abstract
Purpose
We recently revealed the preoperative lymphocyte C-reactive protein ratio (LCR) to be a new marker for predicting various outcomes in malignancies. The aim of our present study was to clarify the potential utility of the preoperative LCR for predicting the perioperative risk and oncological outcome in esophageal cancer patients.
Methods
We analyzed the preoperative LCR from 153 esophageal cancer patients to clarify its clinical relevance.
Results
The preoperative LCR was significantly decreased in a stage-dependent manner, and a decreased preoperative LCR was significantly associated with the occurrence of postoperative surgical site infection. Esophageal cancer patients with a low LCR showed a poor outcome in both the overall survival and disease-free survival compared with those who had a high LCR. Multivariate analyses showed that a decreased LCR was an independent prognostic factor for both a poor overall survival and disease-free survival. A decreased preoperative LCR was an independent predictive factor for postoperative surgical site infection and significantly correlated with nutritional and inflammatory indicators. In addition, the LCR was useful for identifying esophageal cancer patients likely to have a poor outcome among patients with and without neoadjuvant chemotherapy.
Conclusions
Assessing the preoperative LCR might help physicians identify populations at high risk for perioperative complication and oncological outcomes, and determine individualized perioperative therapeutic strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer (EC) is the sixth-most common cause of cancer-related death worldwide [1]. With advances in our understanding of tumor biology, new evidence has been uncovered that provides further insight into this disease. Recent advances in multimodality therapy have provided survival benefits to EC patients. However, the long-term prognosis of patients undergoing potentially curative esophageal resection remains poor [2]. The ability to predict tumor behavior would be informative for patients and clinician during the decision-making process. Therefore, there is a clear need for prognostic biomarkers that identify high-risk EC patients to provide each patient with favorable intensive therapy.
The inflammatory response is intimately related to tumorigenesis, and an elevated inflammatory response is correlated with a poor survival in numerous cancers [3,4,5]. In esophageal squamous cell carcinoma in particular, the pathogenesis is robustly related to chronic inflammation caused by alcohol drinking and cigarette smoking. Chronic inflammation from these sources can lead to mucosal injury and subsequent DNA damage [6, 7]. In addition, inflammatory processes are thought to affect various steps of carcinogenesis and play a pivotal role in the underlying biological mechanisms of resistance to chemotherapeutic treatment for EC patients [8]. Furthermore, previous studies have shown that perioperative complications are associated with an unfavorable short-term quality of life and long-term oncology outcome of early recurrence and a poor survival after esophagectomy [9, 10]. Therefore, a biomarker that also evaluates the risk of perioperative complications would be useful.
Our previous study showed that several scoring systems for inflammatory status have potential utility for predicting the perioperative risk and oncological outcome in gastrointestinal cancer patients [11,12,13,14,15,16,17,18,19]. Recently, our newly developed biomarker of the lymphocyte C-reactive protein ratio (LCR) was shown to be a predictive biomarker for recurrence, the prognosis, and postoperative morbidity in CRC patients, and it proved useful for perioperative management and as a postoperative oncological follow-up strategy [20].
In this study, we explored the clinical significance of the LCR as a prognostic biomarker for EC patients receiving surgery and identified patients whose prognosis was likely to improve according to the choice of postoperative therapeutic strategy.
Methods
Patients
In this study, we enrolled 153 patients who underwent surgery for EC at our institution between 2002 and 2017. All patients were classified according to the International Union against Cancer TNM Classification (seventh edition). Before treatment, 18 patients (11.8%) had clinical stage 0 disease, 41 (26.8%) had stage I, 47 (30.7%) had stage II, 30 (19.6%) had stage III, and 17 (11.1%) had stage IV disease. The surgical approaches included thoracoscopic esophagectomy and both left and right transthoracic esophagectomy. Sixty-five patients (42.4%) received neoadjuvant chemotherapy (NAC) before surgery (with or without radiation therapy). Preoperative treatment options were determined based on the tumor stage and operability, including the patient’s age and history. Neoadjuvant chemotherapy was performed as 5-fluorouracil and cisplatin for two cycles. Chemoradiotherapy schedules consisted of three cycles of 5-fluorouracil and cisplatin weekly and 2.0 Gy per fraction for a total dose of 30 Gy.
Patients were followed up using our standard protocol every 12–16 weeks for at least 1 year. This protocol included tumor-marker studies, computed tomography, endoscopic examinations, ultrasonography, and chest radiography. Bone scans were performed when bone metastasis was indicated. Data collected from inpatient and outpatient records included demographic data (age and sex), tumor-specific data, pathologic data [including T classification, lymph-node metastasis, distant metastasis, histology, and tumor markers, including carcinoembryonic antigen (CEA) and squamous cell carcinoma antigen (SCC), at the diagnosis], and survival data [disease-free survival (DFS) and overall survival (OS)].
Postoperative surgical site infection (SSI) as a primary short-term post-operative outcome was defined as that occurring within 30 days of surgery. Details of SSI were obtained from a prospectively collected database and, where necessary, from patient medical records. Postoperative SSI included wound infection (superficial or deep infection requiring treatment with antibiotic agents or wound drainage) and intra-abdominal abscess (intra-abdominal fluid collection associated with a fever or leucocytosis that discharged spontaneously or required surgical or radiologically guided drainage, with positive blood or fluid culture).
Written informed consent was obtained from all patients, and the study was approved by the Institutional Review Board of Mie University Hospital.
Laboratory measurements
Each patient’s blood specimen was obtained within 1 day prior to surgery. A full blood count (FBC) and blood molecules, including albumin (ALB), choline esterase (Ch-E), CRP levels, and tumor markers, were evaluated during a routine blood examination. The LCR was calculated as follows: lymphocyte count/C-reactive protein. The cut-off value for the LCR was defined according to the receiver-operating characteristic (ROC) curve analysis with Youden’s index for the survival. The cut-off value for ALB was 3.5 g/dl and for Ch-E was 240 U/l depending on the upper limit of the normal range in our institute. In addition, the cut-off values for CEA (5 ng/ml) and SCC (1.5 ng/ml) were the upper limit of the normal range in our institute.
Statistical analyses
The association between the LCR and clinicopathological findings was analyzed using the Kruskal–Wallis test to clarify the clinical significance as both a prognostic and predictive biomarker of treatment. Results are expressed as the median ± interquartile range (IQR). F tests were conducted to assess the equality of variance for comparable groups. For time-to-event analyses, survival estimates were calculated using a Kaplan–Meier analysis, and groups were compared using the log-rank test. The OS was measured from the date the patient underwent surgery until the date of death resulting from any cause or until the last known follow-up in patients who were still alive. The DFS was measured from the date the patient underwent curative surgery to the date of disease recurrence, death from any cause (i.e., cancer-unrelated deaths were not censored), or until the last contact with the patient. ROC curves were established to discriminate the patients who died from those who survived for the OS and those who did have recurrence from those who did not have it for the DFS. Youden’s index was used to determine the optimal cut-off threshold of the LCR from our EC cohort for predicting the OS and DFS. Cox’s proportional hazards model was used to estimate hazard ratios (HRs) for the OS and DFS. The assumption of proportionality was confirmed for the Cox proportional hazard analyses by generating Kaplan–Meier survival curves (e.g., LCR low group and LCR high group) and by ensuring that the two curves did not intersect.
Multivariate logistic regression models were used to predict factors influencing postoperative infectious complication. Multivariate analyses were performed using the factors that were significant in univariate analyses. Clinical variables that were considered for univariate and multivariate analyses, in addition to the target LCR, were previously identified confounding factors with an impact on the prognosis and perioperative complications in patients with EC: sex, age at the diagnosis, histology, pathological T stage (T1/2 or T3/4), lymph-node metastasis (present or absent), distant metastasis (present or absent), neutrophil–lymphocyte ratio (NLR; < 2.5 or ≥ 2.5), modified Glasgow prognostic score (mGPS; 2 or 0,1), CEA levels (≥ 5.0 ng/mL or < 5.9 ng/mL), SCC levels (≥ 1.5 ng/mL or < 1.5 ng/mL), body mass index (BMI; < median or ≥ median), ALB (< 3.5 g/dl or ≥ 3.5 g/dl), Ch-E (< 240 U/l or ≥ 240 U/l), operation time (< median or ≥ median), and blood loss (< median or ≥ median). All p values were two-sided, and P < 0.05 was considered statistically significant. All statistical analyses were carried out using the JMP 13.1 software program (SAS Institute Inc., Cary, North Carolina, USA).
Results
Association between the LCR and disease progression in patients with EC
The median value of the preoperative LCR was 11,750 [95% confidence interval (CI): 17,469–28,018]. Table 1 shows the association between the clinicopathological findings and the preoperative LCR in EC patients. A lower LCR was significantly associated disease progression factors, such as advanced T classification (T3/4, P = 0.02) and TNM stage (stage III/IV, P = 0.02). Furthermore, the preoperative LCR was significantly decreased in EC patients with a history of neoadjuvant treatment compared with those with no such history in this cohort (P < 0.0001). This finding suggested that patients who underwent neoadjuvant treatment had more advanced disease and thus a lower LCR (Supplementary Table 1). Regarding postoperative complications, a lower LCR was associated with SSI (P = 0.02).
EC patients with a low LCR showed a poor outcome for both the OS and DFS
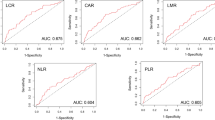
Next, we investigated the prognostic impact of the preoperative LCR on the OS and DFS of EC patients. To generate Kaplan–Meier curves subdivided by the preoperative LCR, we first performed ROC analyses to define the optimal cut-off value of the preoperative LCR. ROC analyses for the OS showed that 7842 was the cut-off value of the LCR that could discriminate EC patients with a poor prognosis from those without a poor prognosis, with an area under the curve (AUC) of 0.65 (sensitivity: 0.60, specificity: 0.69, Fig. 1a). Interestingly, ROC analyses for the DFS showed that the same cut-off value of the LCR (7842) could discriminate EC patients with recurrence from those without is, with an AUC of 0.65 (sensitivity: 0.58, specificity: 0.70, Fig. 1b). Subsequent time-to-event analyses showed that EC patients with a low LCR (< 7842; N = 61) were significantly more likely to have a poor outcome than those with a high LCR (≥ 7842; N = 92) in terms of the OS (log-rank test, P = 0.003, Fig. 1c). In addition, EC patients with a low LCR (< 7842; N = 55) were significantly more likely to have a poor DFS than those with a high LCR (≥ 7842; N = 75; log-rank test, P = 0.001, Fig. 1d).
A receiver-operating characteristic (ROC) analysis for the overall survival (OS) showed that 7842 as the cut-off value of the lymphocyte C-reactive protein ratio (LCR) discriminated esophageal cancer (EC) patients with a poor prognosis from those with a good prognosis, with an area under the curve (AUC) of 0.65 (a). An ROC analysis for the disease-free survival (DFS) showed that 7842 as the cut-off value of the LCR discriminated EC patients with early recurrence from those without early recurrence, with an AUC of 0.65 (b). A time-to-event analysis showed that patients with a low LCR were significantly correlated with poor outcomes compared to those with a high LCR in terms of the OS (c). EC patients with a low LCR were correlated with early recurrence compared with those with a high LCR in terms of the DFS (d)
A decreased preoperative LCR was an independent prognostic factor for both the OS and DFS
To clarify the potential utility of the preoperative LCR as a prognostic predictor for the survival and recurrence, we conducted a Cox proportional hazard regression analysis for the OS and DFS in EC patients. A multivariate analysis showed that an advanced pathological T stage (HR: 3.02, 95% CI: 1.35–6.74, P = 0.007), presence of lymph-node metastasis (HR: 2.24 95% CI: 1.12–4.67, P = 0.02), presence of distant metastasis (HR: 4.79, 95% CI: 1.54–13.6, P = 0.009), high serum CEA level (HR: 4.17, 95% CI: 2.17–8.08, P < 0.0001), and decreased preoperative LCR (HR: 2.76, 95% CI: 1.33–5.86, P = 0.006) were independent prognostic factors for a poor OS in EC patients (Table 2a). Furthermore, a multivariate analysis revealed that a low preoperative LCR was also an independent prognostic factor for a poor DFS in EC patients (HR: 1.98, 95% CI: 1.06–3.72, P = 0.03, Table 2b).
The preoperative LCR was an independent predictive factor for postoperative SSI
We observed a significant association between the preoperative LCR and postoperative SSI in EC patients (Table 1). One clinically necessary biomarker for the perioperative period is a predictive biomarker for identifying patients at risk of infectious complications, especially SSI. We, therefore, analyzed the predictive factors of SSI in EC patients by a logistic regression analysis. A multivariate analysis showed that a low LCR (≤ 7842) was the only independent factor for predicting SSI in EC patients [odds ratio (OR): 2.62, 95% CI: 1.12–6.12, P = 0.03, Table 3].
The preoperative LCR reflects the nutritional or inflammatory status of the host
Several lines of evidence demonstrated that preoperative nutritional or inflammatory status predicted postoperative SSI in various malignancies [21]. Furthermore, recent evidence from our group first showed that the preoperative LCR reflected the nutritional status of patients with gastric cancer [22]. Based on this evidence, we further assessed the direct correlation between the preoperative LCR and nutritional or inflammatory indicators in EC patients. As nutritional factors, although the BMI did not correlate with the LCR (Fig. 2a), serum ALB and Ch-E showed positive correlations with the LCR (ALB: R = 0.30, P = 0.0002; Ch-E: R = 0.23, P = 0.005, Fig. 2b, c). In addition, as inflammatory indicators, the NLR and mGPS demonstrated negative correlations with the LCR (NLR: R = − 0.27, P = 0.001; mGPS: R = − 0.35, P < 0.0001, Fig. 2d, e).
The evaluation of the correlation between nutritional or inflammatory markers and the lymphocyte C-reactive protein ratio (LCR). As a nutritional marker, the BMI did not have a significant correlation with the LCR (a), while the serum albumin (ALB) and choline esterase (Ch-E) showed positive correlations with the LCR (b, c). As inflammatory indicators, the neutrophil-to-lymphocyte ratio (NLR) and modified Glasgow prognostic score (mGPS) showed negative correlations with the LCR (d, e)
The preoperative LCR identified EC patients with a poor OS and DFS among those who did and did not receive NAC
Although the prognostic impact of the LCR was revealed in the total cohort, some of the EC patients received NAC before surgery in our cohort. This adjuvant therapy may have affected their laboratory data. Indeed, EC patients who received NAC might have had a reduced preoperative LCR compared with those who did not (6385 ± 14,205 vs. 19,125 ± 28,789, P < 0.0001, Fig. 3a). Therefore, we next investigated whether or not the LCR was a predictor of a poor OS and DFS in EC patients divided by whether or not they were receiving NAC (NAC[ −] group: N = 89; NAC[ +] group: N = 64). Although adjusting the cut-off threshold in each cohort was necessary due to the effect of NAC, a survival curve analysis based on the NAC( −) group showed a clear stratification for assessing the prognosis using the LCR for both the OS and DFS (Fig. 3b, c). Furthermore, the preoperative LCR status identified EC patients with a poor OS and DFS in the NAC( +) group (Fig. 3d, e). In addition, a multivariate Cox regression analysis revealed very consistent findings for the total cohort and showed that a low LCR was an independent prognostic factor, especially for the DFS, in both groups (NAC[ −] EC patients: DFS, HR = 9.53, 95% CI: 1.76–44.4, P = 0.01, Table 4a, b; NAC[ +] EC patients: DFS, HR = 2.27, 95% CI: 1.11–4.98, P = 0.02, Table 5a, b).
The lymphocyte C-reactive protein ratio (LCR) was decreased among esophageal cancer (EC) patients who did and did not receive neoadjuvant chemotherapy (NAC) (a). Survival curve analyses based on the NAC( −) group showed clear stratification for assessing the prognosis for both the overall survival (OS) and disease-free survival (DFS), with an LCR cut-off value of 1865 (b, c). The LCR also identified EC patients with a poor OS and DFS in the NAC( +) group with an LCR cut-off value of 7842 (d, e)
Discussion
The systemic inflammatory response may contribute to tumor development, and emerging evidence has suggested the potential utility of several parameters for assessing the systemic inflammation status, including neutrophils, lymphocytes, albumin, and CRP, to predict the prognosis of the oncological outcome in EC patients [4, 23,24,25,26]. In addition, several combination markers, such as the NLR and mGPS, have been described as feasible prognostic biomarkers for malignancies [27, 28].
Our recently developed parameter of the LCR is calculated using the lymphocyte count and serum CRP level and mainly assesses the systemic inflammation and nutritional status [20, 22]. The LCR can be a more reliable indicator of a poor oncological outcome than other combinations of inflammatory markers as well as a reliable indicator of perioperative complications, as previously described [20]. Furthermore, a recent study from another group also validated these findings in other types of cancer [29]. However, the predictive potential of the preoperative LCR for the short-term (perioperative risk) and long-term outcomes (prognosis) in EC patients have never been elucidated. Thus, this study explored whether or not the preoperative LCR can be used as a predictive biomarker for the perioperative risk and prognosis in EC patients.
Several novel findings were demonstrated regarding the clinical relevance of the preoperative LCR during the course of this study. First, we showed that a low preoperative LCR was significantly associated with clinicopathological factors for disease development and that EC patients with a low preoperative LCR showed a poorer prognosis for both the OS and DFS than those with a high preoperative LCR. Second, a low preoperative LCR was an independent prognostic factor for both OS and DFS. Third, we showed that a low preoperative LCR was a potential predictor for postoperative SSI, because it reflects the host’s systemic nutrition and inflammation status. Finally, we showed that the preoperative LCR identified EC patients with a poor prognosis, especially with regard to the DFS, among populations who did or did not receive NAC.
Inflammation and the immune response play critical roles in cancer development. Lymphocytes are assigned a major role in immune surveillance, and tumor-infiltrating lymphocytes are widely recognized as key indicators of antitumor effects via the host’s cytotoxic immune response [24]. Lymphocytes infiltrating the tumor microenvironment are a trigger for a cell-mediated immunological antitumor reaction, and this cell-mediated immune response is largely dependent on lymphocytes [24]. Therefore, lymphopenia is recognized as a marker of host immunological incompetence for malignant disease and a prognostic marker for the oncological outcome [30,31,32]. CRP is a well-established serum marker reflecting systemic inflammatory responses in clinical settings. In addition, it has a role as both a marker of cancer development and a prognostic marker [4]. Some studies have shown that an elevated CRP level was associated with an unfavorable prognosis and/or perioperative complications in EC patients [23, 33, 34]. Furthermore, CRP has been combined with other markers of the systemic inflammatory response in prognostic scores, such as mGPS, and has been shown to be a useful prognostic biomarker in several types of tumor [4]. Given the above evidence, the preoperative LCR is expected to be able to assess the combined status of the host immunological response and systemic inflammation, and a decreased LCR might reflect an impaired immunological response and an enhanced systemic inflammatory response in EC patients. Thus, LCR can be a more reliable prognostic marker and predictor of recurrence than the peripheral lymphocyte count or serum CRP alone.
In the present study, we also revealed that the preoperative LCR status is a potential predictor for postoperative SSI. Several lines of evidence have demonstrated a preoperative systemic inflammatory reaction via host–tumor interactions, including immune disorders and malnutrition, as a potential predictive marker for postoperative complications in cancer patients. The LCR had a positive correlation with other serum biomarkers that reflect immune and nutritional conditions, such as ALB and Ch-E. ALB reflects inflammation and nutrition, and a low ALB status is associated with postoperative complications [25]. A low Ch-E concentration is also thought to be indicative of immune disorders and malnutrition, and therefore, it is closely associated with postoperative complications [35, 36]. However, the LCR has a negative correlation with the NLR and mGPS as relevant combination biomarkers reflecting the immune and nutritional status. Although the preoperative status of the inflammatory markers in this study was not found to be an independent factor for predicting postoperative SSI, the preoperative LCR, which was correlated with all of these inflammatory markers, was extracted as an independent predictor for postoperative SSI in RC patients. Considering our findings alongside previous evidence concerning lymphocytes and the CRP level, the LCR might represent not only an immunological response and systemic inflammatory response but also the nutritional condition of the host. Collectively, the preoperative LCR may be used as a predictive biomarker for postoperative SSI in EC patients.
Another main result of our study was that the preoperative LCR status identified EC patients with a poor oncological outcome among those who were or were not receiving NAC, even though the LCR differed by the treatment course. The theoretical advantages of adding chemotherapy before surgery for EC are the potential for tumor downstaging and for targeting micro-metastasis, which can decrease the risk of distant metastasis [37]. Preoperative chemotherapy with fluorouracil and cisplatin (FP) is currently regarded as standard treatment for EC patients with stage II/III disease in Japan [37]. However, whether preoperative treatment alone is sufficient or if postoperative chemotherapy should additionally be given after surgery remains controversial. A recent phase III study suggested that perioperative chemotherapy may improve the oncological outcome compared with preoperative chemotherapy alone [38]. Considering this background with significant costs and renal toxicity for NAC, a predictive biomarker would be clinically relevant for identifying populations who could benefit from NAC and who would have a high risk of an oncological outcome despite receiving NAC. Interestingly, our LCR approach identified EC patients with a poor DFS in the NAC( −) and NAC( +) groups. Identifying NAC( −) patients with a high risk for an oncological outcome could allow physicians to change the treatment strategy for EC patients who truly need preoperative chemotherapy. Furthermore, the identification of a high-risk population for oncological outcome among NAC( +) EC patients would also help physicians decide on additional chemotherapy treatment options after surgery. Despite the differing cut-off thresholds of the preoperative LCR in patients who do or do not receive NAC, stratifying the outcome using the preoperative LCR is directly linked to decision-making concerning perioperative treatment strategies in EC patients.
Several limitations associated with the present study warrant mention. First, this study was a retrospective and relatively small cohort study. Second, all of the enrolled patients were from a single institution in Japan. Third, whether or not the cut-off threshold of the LCR was optimal is unclear. Although we determined the cut-off threshold of the LCR using ROC curves with Youden’s index and clearly demonstrated the predictive value of the preoperative LCR for the OS and DFS, a further validation study will be needed to confirm the prognostic value of the preoperative LCR with a cut-off value of 7842. To overcome these limitations, larger multicenter prospective controlled trials are needed to confirm the prognostic value of the preoperative LCR and its cut-off value and investigate the prognostic and predictive potential of the LCR for identifying EC patients at a high risk of poor outcomes.
In conclusion, our study highlights the clinical utility of the preoperative LCR as a predictive biomarker for the perioperative risk and oncological outcome in EC patients. Assessing the preoperative LCR might help physicians determine individualized perioperative therapeutic strategies.
References
Global Burden of Disease Cancer C, Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, et al. Global, regional, and National cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global burden of disease study. JAMA Oncol. 2017;3(4):524–48.
Anderson LA, Tavilla A, Brenner H, Luttmann S, Navarro C, Gavin AT, et al. Survival for oesophageal, stomach and small intestine cancers in Europe 1999–2007: results from EUROCARE-5. Eur J Can. 2015;51(15):2144–57.
Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nature reviews. Clin Oncol. 2015;12(10):584–96.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Radojicic J, Zaravinos A, Spandidos DA. HPV, KRAS mutations, alcohol consumption and tobacco smoking effects on esophageal squamous-cell carcinoma carcinogenesis. Int J Biol Markers. 2012;27(1):1–12.
Toh Y, Oki E, Ohgaki K, Sakamoto Y, Ito S, Egashira A, et al. Alcohol drinking, cigarette smoking, and the development of squamous cell carcinoma of the esophagus: molecular mechanisms of carcinogenesis. Int J Clin Oncol. 2010;15(2):135–44.
Lin R, Zhang C, Zheng J, Tian D, Lei Z, Chen D, et al. Chronic inflammation-associated genomic instability paves the way for human esophageal carcinogenesis. Oncotarget. 2016;7(17):24564–71.
Baba Y, Yoshida N, Shigaki H, Iwatsuki M, Miyamoto Y, Sakamoto Y, et al. Prognostic impact of postoperative complications in 502 patients with surgically resected esophageal squamous cell carcinoma: a retrospective single-institution study. Ann Surg. 2016;264(2):305–11.
Lerut T, Moons J, Coosemans W, Van Raemdonck D, De Leyn P, Decaluwe H, et al. Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg. 2009;250(5):798–807.
Fujikawa H, Toiyama Y, Inoue Y, Imaoka H, Shimura T, Okigami M, et al. Prognostic impact of preoperative albumin-to-globulin ratio in patients with colon cancer undergoing surgery with curative intent. Anticancer Res. 2017;37(3):1335–42.
Mohri Y, Tanaka K, Ohi M, Saigusa S, Yasuda H, Toiyama Y, et al. Identification of prognostic factors and surgical indications for metastatic gastric cancer. BMC cancer. 2014;14:409.
Mohri Y, Tanaka K, Toiyama Y, Ohi M, Yasuda H, Inoue Y, et al. Impact of preoperative neutrophil to lymphocyte ratio and postoperative infectious complications on survival after curative gastrectomy for gastric cancer: a single institutional cohort study. Medicine. 2016;95(11):e3125.
Oki S, Toiyama Y, Okugawa Y, Shimura T, Okigami M, Yasuda H, et al. Clinical burden of preoperative albumin-globulin ratio in esophageal cancer patients. Am J Surg. 2017;214(5):891–8.
Shimura T, Toiyama Y, Saigusa S, Imaoka H, Okigami M, Fujikawa H, et al. Inflammation-based prognostic scores as indicators to select candidates for primary site resection followed by multimodal therapy among colorectal cancer patients with multiple metastases. Int J Clin Oncol. 2017;22(4):758–66.
Toiyama Y, Inoue Y, Kawamura M, Kawamoto A, Okugawa Y, Hiro J, et al. Elevated platelet count as predictor of recurrence in rectal cancer patients undergoing preoperative chemoradiotherapy followed by surgery. Int Surg. 2015;100(2):199–207.
Toiyama Y, Inoue Y, Saigusa S, Kawamura M, Kawamoto A, Okugawa Y, et al. C-reactive protein as predictor of recurrence in patients with rectal cancer undergoing chemoradiotherapy followed by surgery. Anticancer Res. 2013;33(11):5065–74.
Toiyama Y, Shimura T, Yasuda H, Fujikawa H, Okita Y, Kobayashi M, et al. Clinical burden of C-reactive protein/albumin ratio before curative surgery for patients with gastric cancer. Anticancer Res. 2016;36(12):6491–8.
Toiyama Y, Yasuda H, Ohi M, Yoshiyama S, Araki T, Tanaka K, et al. Clinical impact of preoperative albumin to globulin ratio in gastric cancer patients with curative intent. Am J Surg. 2017;213(1):120–6.
Okugawa Y, Toiyama Y, Yamamoto A, Shigemori T, Ide S, Kitajima T, et al. Lymphocyte-C-reactive protein ratio as promising new marker for predicting surgical and oncological outcomes in colorectal cancer. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003239.
McMillan DC. Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care. 2009;12(3):223–6.
Okugawa Y, Toiyama Y, Yamamoto A, Shigemori T, Ichikawa T, Yin C, et al. Lymphocyte-to-C-reactive protein ratio and score are clinically feasible nutrition-inflammation markers of outcome in patients with gastric cancer. Clin Nutr. 2019;39(4):1209–17.
Asti E, Bonitta G, Melloni M, Tornese S, Milito P, Sironi A, et al. Utility of C-reactive protein as predictive biomarker of anastomotic leak after minimally invasive esophagectomy. Langenbeck’s archives of surgery. 2018;403(2):235–44.
Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21(2):137–48.
Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J. 2010;9:69.
Uribe-Querol E, Rosales C. Neutrophils in cancer: two sides of the same coin. J Immunol Res. 2015;2015:983698.
Otowa Y, Nakamura T, Takiguchi G, Tomono A, Yamamoto M, Kanaji S, et al. Changes in modified Glasgow prognostic score after neoadjuvant chemotherapy is a prognostic factor in clinical stage II/III esophageal cancer. Dis Esophagus. 2016;29(2):146–51.
Yodying H, Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Yamada M, et al. Prognostic significance of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in oncologic outcomes of esophageal cancer: a systematic review and meta-analysis. Ann Surg Oncol. 2016;23(2):646–54.
Fan Z, Luo G, Gong Y, Liu C, Yu X. ASO author reflections: C-reactive protein/lymphocyte ratio as a promising marker for predicting survival in pancreatic cancer. Ann Surg Oncol. 2020;27(10):4026–7.
Hoffmann TK, Dworacki G, Tsukihiro T, Meidenbauer N, Gooding W, Johnson JT, et al. Spontaneous apoptosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clin Cancer Res. 2002;8(8):2553–62.
Kim US, Papatestas AE, Aufses AH Jr. Prognostic significance of peripheral lymphocyte counts and carcinoembryonic antigens in colorectal carcinoma. J Surg Oncol. 1976;8(3):257–62.
Vayrynen JP, Tuomisto A, Klintrup K, Makela J, Karttunen TJ, Makinen MJ. Detailed analysis of inflammatory cell infiltration in colorectal cancer. Br J Cancer. 2013;109(7):1839–47.
Badakhshi H, Kaul D, Zhao KL. Association between the inflammatory biomarker, C-reactive protein, and the response to radiochemotherapy in patients with esophageal cancer. Mol Clin Oncol. 2016;4(4):643–7.
Zheng TL, Cao K, Liang C, Zhang K, Guo HZ, Li DP, et al. Prognostic value of C-reactive protein in esophageal cancer: a meta-analysis. Asian Pac J Cancer Prev. 2014;15(19):8075–81.
Kanda M, Koike M, Tanaka C, Kobayashi D, Hayashi M, Yamada S, et al. Risk prediction of postoperative pneumonia after subtotal esophagectomy based on preoperative serum cholinesterase concentrations. Ann Surg Oncol. 2019;26(11):3718–26.
Kobayashi T, Oshima K, Yokobori T, Idetsu A, Hayashi Y, Hinohara RN, et al. Perioperative nutriture in esophageal cancer patients undergoing esophagectomy. Hepatogastroenterology. 2013;60(126):1311–6.
Ando N, Kato H, Igaki H, Shinoda M, Ozawa S, Shimizu H, et al. A randomized trial comparing postoperative adjuvant chemotherapy with cisplatin and 5-fluorouracil versus preoperative chemotherapy for localized advanced squamous cell carcinoma of the thoracic esophagus (JCOG9907). Ann Surg Oncol. 2012;19(1):68–74.
Zhao Y, Dai Z, Min W, Sui X, Kang H, Zhang Y, et al. Perioperative versus preoperative chemotherapy with surgery in patients with resectable squamous cell carcinoma of esophagus: a phase iii randomized trial. J Thoracic Oncol. 2015;10(9):1349–56.
Acknowledgements
Yuji Toiyama had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. We thank RJ Frampton from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design (AY, YT, and YO); acquisition of data and the analysis and interpretation of data (AY, YT, YO, TI, HI, HY, HF, YO, TY, and MO); drafting the work critically for important intellectual content (AY, YT, and YO); final approval of the version to be published (AY, YT, YO, and MO); agreement to be accountable for all aspects of the work (AY, YT, YO, TI, HI, HY, HF, YO, TY, and MO).
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflicts of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamamoto, A., Toiyama, Y., Okugawa, Y. et al. Clinical implications of the preoperative lymphocyte C-reactive protein ratio in esophageal cancer patients. Surg Today 51, 745–755 (2021). https://doi.org/10.1007/s00595-020-02166-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-02166-5