Abstract
Purpose
In previous studies, a lack of antibiotic prophylaxis, smoking and obesity were described as factors that contribute to the development of a surgical site infection (SSI) after pilonidal disease (PD) surgery. In this study, we evaluated whether the volume of the excised specimen (VS) was a risk factor for SSI.
Methods
The patients who underwent surgical treatment for PD from January 2010 through December 2011 were retrospectively evaluated in terms of SSI, time off work and healing time. The single and multiple explanatory variable(s) logistic regression analyses were performed.
Results
One-hundred and sixty patients were included in the study. SSI occurred in 19 (11.9 %) patients. In the multiple explanatory variable logistic regression analysis, VS was emerged as a risk factor for SSI (OR 18.78, 95 % CI 2.38–148.10; P < 0.005). The healing time and time off work were longer when a SSI occurred (P < 0.001).
Conclusions
This study suggests that the rate of SSI after the surgical treatment of PD is higher in patients with a high VS. A SSI significantly prolongs the healing time. Surgeons can use this data for assessing the SSI risk. As a preventive measure, prolonged use of an empiric broad-spectrum antibiotic may be beneficial in patients with a high VS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pilonidal disease (PD) predominantly affects younger patients and it usually occurs in the sacrococcygeal region. Acquired and environmental factors have been considered to contribute more to the etiology than congenital factors. The incidence of the disease is reported to be 26 per 100,000 population [1]. It occurs more frequently in young males, and rarely occurs before puberty or after the age of 40 years [1, 2]. Several treatment modalities have been advocated for PD, ranging from conservative non-surgical treatments to extensive resections and flap procedures. The ideal surgery should be simple, should not need a prolonged hospital stay, should have a low recurrence rate, should be associated with minimal wound care and should also reduce the patients’ time off work as far as possible [3].
In surgical practice, the most commonly used techniques are primary closure and various kinds of excision plus flap procedures. The primary aim of excision and primary closure is rapid healing. However, the SSI rates have been reported to be 6 to 14 % after primary closure [4]. The Limberg flap repair is currently preferred for PD treatment due to the low recurrence rate [5, 6]. Nevertheless, the risk of SSI and PD recurrence has not been completely eliminated after Limberg flap repair [7–10].
SSI leads to wound dehiscence and prolonged healing times. It is clear that improved outcomes of PD management could be achieved by SSI prevention. The identification of risk factors for SSI may increase the prevention. In the current literature, two studies have been performed and reported a multiple explanatory variable risk factor analysis for SSI after primary closure for PD. Al-Khayat et al. [11] showed that smoking and obesity were significant predictors of an SSI. In another study with a multiple explanatory variable risk factor analysis for SSI, Popeskou et al. [12] showed that smoking and a lack of antibiotic prophylaxis were significant predictors for a SSI.
The eradication of the sinus tract and complete healing of the overlying skin are essential principles of surgical treatment. The first step in the surgical treatment is wide radical excision of the affected tissue. In patients with extensive disease, the volume of tissue to be excised will be greater, because it is necessary to remove all branches of the sinus tract. The relationship between SSI and the size of PD has not been studied so far. We think that the VS may be used to reflect the size of PD.
In the present study, we investigated the relationship between SSI and VS, in addition to the previously described risk factors after PD surgery, by performing a risk factor analysis.
Patients and methods
This study was approved by the local ethics committee. We retrospectively reviewed our prospectively maintained database of all consecutive patients surgically treated for PD from January 2010 through December 2011. The primary patient list was generated electronically based on diagnostic and surgical intervention codes. Patients at our institution with PD are generally managed with excision and primary closure or Limberg flap repair. The surgeons decided on the type of surgery on the basis of personal experience and subjective estimation. Patients with an acute pilonidal abscess were treated with a simple incision and with antibiotics before the surgical procedure. We included only the patients with a documented follow-up who underwent excision and primary closure or Limberg flap repair for PD. The patients whose wounds were left open for secondary healing were excluded.
All procedures were performed under spinal anesthesia in the prone position. Dissection was performed using electrocautery. All patients received cefazolin sodium (1 g intravenously) for prophylaxis immediately before the operation. The extent of the sinus tract was delineated by infusing each sinus opening with diluted methylene blue dye.
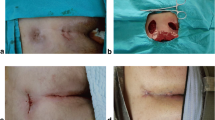
For primary closure, the sinus was resected en bloc through a longitudinal incision. The incision was elliptical, with its lateral margins equidistant from the midline at a level that would allow for apposition of the wound edges. The incision was carried vertically down to presacral fascia. The fat was closed with interrupted 3-0 absorbable sutures in three layers to minimize tissue traction. At the first layer, the fat mass sections were sutured to each other and to the underlying presacral fascia. The skin edges were closed with interrupted polypropylene sutures.
For Limberg flap repair, the sinus was resected en bloc with a rhomboid excision. The rhomboid incision, including the sinus and its extensions, was made down to the presacral fascia. The constructed flap, incorporating the gluteal fascia, was mobilized on its inferior edge and transposed medially to fill the Limberg defect. The subcutaneous layer was approximated with 3-0 absorbable interrupted sutures. The skin was closed with polypropylene sutures.
PD was classified according to Tezel et al. [13] during the preoperative examination. The extent of the sinus tract involvement was delineated by infusing each sinus opening with diluted methylene blue dye. Prophylactic cavity drainage was performed in all patients. The drains were removed after the drainage decreased to less than 10 ml/day. The patient was followed up in our outpatient clinic, and the sutures were typically removed within 2 weeks.
The patient age, gender, body mass index (BMI), VS, duration of surgery, smoking, preoperative hemoglobin (Hb) concentration, American Society of Anesthesiologists (ASA) score, history of diabetes mellitus (DM), hospital stay, postoperative complications, time off work and healing time were recorded for each patient. In the case of wound infection, the wound was drained by the removal of a few sutures, covered with new dressings daily, and oral cefuroxime was given for 7 days, otherwise, oral antibiotics were not used after discharge. The healing time was defined as the number of days from the start of treatment to the last day of dressing or treatment. Time off from work was subjectively defined by each patient. To define the postoperative time off work, the patients were asked when they felt that it was convenient to start their daily activities.
A graduated cylinder was used to measure the VS. First, we poured a known amount of water into the cylinder and then placed the specimen into the water and ensured that it was completely submerged. We noted the increase in the height of the water. The increase in volume from the original volume of water was accepted as the volume of the VS.
Dependent variables
During the investigation of risk factors, SSI was considered the primary end point of this study. SSI was defined according to the Center for Disease Control (CDC) guidelines [14]. The definition of SSI requires that signs and symptoms of wound infection occur within 30 days after the operation. The secondary end point was to investigate the effects of SSI on the time to return to work and the time for complete healing.
Independent variables
Age, a continuous variable, was converted to a categorical variable with two categories (≤25 years, >25 years) based on the median value. The BMI was derived as a ratio of the height and weight (kg/m2), and patients were categorized as non-obese (BMI < 30) and obese (BMI ≥ 30). The VS, a continuous variable, was converted to a categorical variable with two categories (<28 cm3, ≥28 cm3) based on the median value. The length of the operation was evaluated as a continuous variable. Smoking, gender, and the type of operation were already dichotomized.
Statistical analysis
Bivariate comparisons were conducted using Chi-square tests, odds ratio tests and Mann–Whitney U tests. The single and multiple explanatory variable(s) logistic regression analysis methods were employed. In the single explanatory variable logistic regression analysis, we estimated the odds ratios with 95 % confidence intervals of SSI for each study variable, and the significance level of each factor/covariate was determined. The Pearson correlation analyses were used to determine the correlation coefficient. In the multiple explanatory variable logistic regression analysis, the initial model was fit including all significant independent variables. Then, a backward-elimination approach in a multiple explanatory variable logistic regression model was conducted to evaluate the model for potential confounding effects. In this model, the factors/covariates were removed one at a time, starting with the factor/covariate that had the largest P value, until all remaining factors had a two-sided P value <0.05. The goodness of fit was tested using the Hosmer–Lemeshow test.
Results
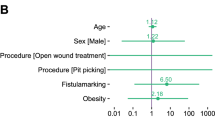
During the study period, 178 patients were surgically treated for PD. Eighteen patients whose wounds were left open for secondary healing were excluded from the study. The remaining 160 patients who underwent primary closure or classic Limberg flap repair were enrolled in the study. The patient characteristics are given in Table 1. Ninety-eight patients were treated with excision and primary closure and 62 patients were treated with excision and classic Limberg flap repair. During the 30-day postoperative follow-up period, an SSI was identified in 19 (11.9 %) patients. These infections required drainage of the wound and regular dressing changes. In the single explanatory variable analysis, smoking, obesity, a longer operation and a high VS were significantly associated with a higher risk of SSI (Table 2). A positive correlation was found between the VS and the duration of surgery (r = 0.552, P < 0.001). In the multiple explanatory variable logistic regression analysis, apart from VS, all factors/covariates were dropped from the model. Finally, only a high VS emerged as a risk factor for SSI (P = 0.005) (Table 3). The model-fitting procedure for the final logistic regression analysis was validated using the Hosmer–Lemeshow goodness of fit test (P = 0.556).
The median (Q1–Q3) for the healing time was 15 days (14–15) in patients without SSI and 33 days (28–43) in patients with SSI (P < 0.001). The median (Q1–Q3) time off work was 7 days (7–10) in patients without SSI and 10 days (7–12) in patients with SSI (P < 0.001). The overall medians (Q1–Q3) for the healing time and time off work were 15 days (14–19) and 7 days (7–10), respectively.
Discussion
In this study, a risk factor analysis was performed for SSI on 160 patients with PD who were treated with primary closure or Limberg flap repair. We found a SSI rate of 11.9 %, which compares well with published series [15]. The principal finding of this study is that a high VS is the main independent predictor of SSI. To the best of our knowledge, the relationship between SSI and the volume of the excised tissue has never been studied so far.
Especially after major breast surgery, the amount of the excised tissue was investigated as risk factor for SSI, however, a relationship between the amount of tissue removed with the risk of SSI was not demonstrated [16, 17]. The most commonly performed procedures for pilonidal disease involve a wide excision of the affected area of skin and underlying fatty tissue. The skin incision must involve all sinus openings. After passing the skin and subcutaneous tissue, the surgeons adjust the width of the excision to include all branches of the sinus tract. In another words, a high VS reflects extensive disease in the underlying fatty tissue. The volume of the sinus cavity and the weight and length of the excised specimen have been evaluated as risk factors for recurrence, but not for SSI [18–20]. This is the first study to investigate the relationship between SSI and the VS by a multiple explanatory variable logistic regression analysis. The logistic regression analysis revealed that, apart from the VS, all factors/covariates can be dropped from the model. The odds of developing a SSI were 19-folds higher in patients with a high VS (OR 18.78, 95 % CI 2.38–148.10; P < 0.005).
There have been only two studies that performed a multiple explanatory variable risk factor analysis for SSI, which found that obesity, smoking and a lack of preoperative antibiotic prophylaxis were risk factors for wound infection after PD surgery [11, 12]. All wounds lose their local vascular supply as a result of surgery. Therefore, postoperatively, there is often relative hypoperfusion or hypoxia. This provides an environment that supports the proliferation of bacteria in the wound. The risk of infection is related to the tissue oxygen partial pressure [21]. Smoking is a known factor that causes peripheral tissue hypoxia, reduced collagen synthesis and deteriorated oxidative killing mechanisms of neutrophils [22, 23]. Several mechanisms have been proposed to explain how obesity increases the risk of SSI. For example, it was suggested that the interactions of adipocytes with the immune system may result in impairment of the immune response [24, 25]. The technical difficulty during surgery, relative hypoperfusion and tissue trauma and tension on the healing of wound have also been reported to underlie this relationship [21, 26]. Like other studies [11, 12], obesity and smoking were risk factors for a SSI in the single explanatory variable analysis, but in our study, this was not confirmed after fitting the multiple explanatory variable logistic regression analysis.
A prolonged operation has been identified as an independent risk factor for SSI in a variety of surgical procedures, including gynecological surgery, orthopedic surgery, and general oncological surgery. In a multivariate analysis, Haley et al. [27] showed that an operation lasting more than 2 h is an independent predictor of SSI. In this study, the duration of surgery also seemed to be a risk factor for SSI in the single explanatory variable analysis, but it was not confirmed after fitting the multiple explanatory variable logistic regression analysis. Nevertheless, we found a positive correlation between the duration of surgery and the VS. This should be kept in mind when interpreting this result.
There is no definitive consensus on prophylactic antibiotic use prior to PD surgery. However, PD is accepted to produce ‘‘contaminated’’ surgical wounds, and prophylactic antibiotic use is recommended [28]. Sondenaa et al. [29] found no difference in the wound complication rates with respect to antibiotic prophylaxis. However, Popeskou et al. [12] demonstrated that a lack of preoperative antibiotic prophylaxis was significantly associated with a higher risk of SSI. Chaudhuri et al. [30] showed that an empiric broad-spectrum 5-day antibiotic regimen was superior to a single-dose antibiotic prophylaxis in preventing infection-related wound complications following PD surgery. We routinely use single-dose antibiotic prophylaxis prior to PD surgery in our institute; therefore, this factor could not be analyzed.
Most of the published studies about the issue have shown that primary closure is associated with higher SSI rates [8–10]. A recently published meta-analysis showed that wound infection was less-frequently encountered after rhomboid flap excision than the primary closure [31]. In our study, the patients treated with primary closure seemed to suffer SSI more often, but the difference was not significant, which might have been due to the relatively small sample size of our study.
Infection was associated with a prolonged healing time. Based on the results of our study, we concluded that the healing time was approximately two times longer when a SSI occurred. Similarly, the time off work was found to be longer in patients with a SSI. A randomized controlled trial previously showed that the development of a SSI after PD surgery predicts a higher risk of recurrence [32], and that the total costs may have been increased due to prolonged healing time. However, the assessment of the total costs and recurrence rates were not within the scope of this study.
There are several limitations to this study that should be kept in mind when interpreting the results. First, we evaluated some of the potential risk factors for SSI. Due to the retrospective nature of the study, it was difficult to evaluate all possible risk factors for SSI, such as skin color, occupation, hair characteristics or the location of sinus orifices.
In conclusion, our results suggest that a high VS is a significant risk factor for SSI after pilonidal sinus surgery. The risk of SSI increased with increasing VS. The results obtained from this study may be useful for surgeons in assessing SSI risk. In addition, our results suggest that there might be a benefit of using an empiric broad-spectrum antibiotic (extended post-discharge) for patients with a high VS, when clinically appropriate, as a preventive measure.
References
Sondenaa K, Andersen E, Nesvik I, Soreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10:39–42.
Dwight RW, Maloy JK. Pilonidal sinus: experience with 449 cases. N Engl J Med. 1953;249(23):926–30.
Solla JA, Rothenberger DA. Chronic pilonidal disease: an assessment of 150 cases. Dis Colon Rectum. 1990;33:758–61.
Zimmerman CE. Outpatient excision and primary closure of pilonidal cysts and sinuses. Long-term follow-up. Am J Surg. 1984;148:658–9.
Cihan A, Mentes BB, Tatlicioglu E, Ozmen S, Leventoglu S, Ucan BH. Modified Limberg flap reconstruction compares favourably with primary repair for pilonidal sinus surgery. ANZ J Surg. 2004;74(4):238–42.
Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg. 2005;92:1081–4.
Arumugam PJ, Chandrasekaran TV, Morgan AR, Beynon J, Carr ND. The rhomboid flap for pilonidal disease. Colorectal Dis. 2003;5:218–21.
Yilmaz S, Kirimlioglu V, Katz D. Role of simple V-Y advancement flap in the treatment of complicated pilonidal sinus. Eur J Surg. 2000;166:269–72.
Cubukcu A, Gonullu NN, Paksoy M, Alponat A, Kurt M, Ozbay O. The role of obesity on the recurrence of pilonidal sinus disease in patients, who were treated by excision and Limberg flap transposition. Int J Colorectal Dis. 2000;15:173–5.
Quinodoz PD, Chilcott M, Grolleau JL, Chavoin JP, Costagliola M. Surgical treatment of sacrococcygeal pilonidal sinus disease by excision and skin flaps: the Toulouse experience. Eur J Surg. 1999;165:1061–5.
Al-Khayat H, Al-Khayat H, Sadeq A, et al. Risk factors for wound complication in pilonidal sinus procedures. J Am Coll Surg. 2007;205(3):439–44.
Popeskou S, Christoforidis D, Ruffieux C, Demartines N. Wound infection after excision and primary midline closure for pilonidal disease: risk factor analysis to improve patient selection. World J Surg. 2011;35(1):206–11.
Tezel E. A new classification according to navicular area concept for sacrococcygeal pilonidal disease. Colorectal Dis. 2007;9(6):575–6.
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infection in the acute care setting. Am J Infect Control. 2008;36(5):309–32.
Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Dis Colon Rectum. 2002;45(11):1458–67.
Angarita FA, Acuna SA, Torregrosa L, Tawil M, Escallon J, Ruíz Á. Perioperative variables associated with surgical site infection in breast cancer surgery. J Hosp Infect. 2011;79(4):328–32.
Olsen MA, Lefta M, Dietz JR, et al. Risk factors for surgical site infection after major breast operation. J Am Coll Surg. 2008;207(3):326–35.
Anderson JH, Yip CO, Nagabhushan JS, Connelly SJ. Day-case Karydakis flap for pilonidal sinus. Dis Colon Rectum. 2008;51(1):134–8.
El-Shaer WM. The modified gluteal sliding plication closure in the treatment of chronic pilonidal sinus. Int J Colorectal Dis. 2010;25(7):887–94.
Kaymakcioglu N, Yagci G, Simsek A, et al. Treatment of pilonidal sinus by phenol application and factors affecting the recurrence. Tech Coloproctol. 2005;9(1):21–4.
Hopf HW, Hunt TK, West JM, et al. Wound tissue oxygen tension predicts the risk of wound infection in surgical patients. Arch Surg. 1997;132:997–1004 (discussion 1005).
Fawcett A, Schembekar M, Church JS, Vashisht R, Springall RG, Nott DM. Smoking, hypertension, and colonic anastomotic healing: a combined clinical and histopathological study. Gut. 1996;38:714–8.
Jorgensen LN, Kallehave F, Christensen E, Siana JE, Gottrup F. Less collagen production in smokers. Surgery. 1998;123:450–5.
Pond CM. Adipose tissue and the immune system. Prostaglandins Leukot Essent Fatty Acids. 2005;73:17–30.
Nieman DC, Henson DA, Nehlsen-Cannarella SL, et al. Influence of obesity on immune function. J Am Diet Assoc. 1999;99:294–9.
Kabon B, Nagele A, Reddy D, et al. Obesity decreases perioperative tissue oxygenation. Anesthesiology. 2004;100:274–80.
Haley RW, Culver DH, Morgan WM, White JW, Emori TG, Hooton TM. Identifying patients at high risk of surgical wound infection. A simple multivariate index of patient susceptibility and wound contamination. Am J Epidemiol. 1985;121:206–15.
Cruse PJ, Foord R. The epidemiology of wound infection: a 10-year prospective study of 62, 939 wounds. Surg Clin North Am. 1980;60(1):27–40.
Sondenaa K, Nesvik I, Gullaksen FP, et al. The role of cefoxitin prophylaxis in chronic pilonidal sinus treated with excision and primary suture. J Am Coll Surg. 1995;180(2):157–60.
Chaudhuri A, Bekdash BA, Taylor AL. Single-dose metronidazole vs 5-day multi-drug antibiotic regimen in excision of pilonidal sinuses with primary closure: a prospective, randomized, double-blinded pilot study. Int J Colorectal Dis. 2006;21(7):688–92.
Horwood J, Hanratty D, Chandran P, Billings P. Primary closure or rhomboid excision and Limberg flap for the management of primary sacrococcygeal pilonidal disease? A meta-analysis of randomized controlled trials. Colorectal Dis. 2012;14(2):143–51.
Sondenaa K, Diab R, Nesvik I, et al. Influence of failure of primary wound healing on subsequent recurrence of pilonidal sinus: combined prospective study and randomised controlled trial. Eur J Surg. 2002;168(11):614–8.
Conflict of interest
Hunsu Alptekin and co-authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alptekin, H., Yilmaz, H., Kayis, S.A. et al. Volume of the excised specimen and prediction of surgical site infection in pilonidal sinus procedures (surgical site infection after pilonidal sinus surgery). Surg Today 43, 1365–1370 (2013). https://doi.org/10.1007/s00595-012-0444-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-012-0444-x