Abstract
Background
The surgical approach to pilonidal sinus disease is open to debate with no ideal treatment. The aim of this work is to present the efficacy of the modified gluteal sliding plication closure technique in treatment of pilonidal sinus disease as regards the complication and recurrence rates, while maintaining a more cosmetically acceptable midline scar.
Patients and methods
All patients between the year 2000 and 2008 with symptomatic pilonidal disease were treated by the modified gluteal sliding plication closure method, except for recurrent cases after previous flap surgery. Outcome measures included wound complications, recurrence rate, follow-up period, and functional recovery. Patient esthetic satisfaction rates as regards the scar and shape of the buttocks were included on a scale of good, fair, or bad.
Results
Fifty-six patients, 41 male and 15 females, with 23 years median age (range, 17–45 years) were treated. After a median follow-up period of 12 months (range, 6–84 months), the incidence of recurrence was 1.8%, infection rate of 10.7%, paresthesia and seroma accumulation in 3.6% of cases. The median functional recovery achieved was 12 days (range, 10–45 days), while the esthetic satisfaction rates were good in 78.57%, fair in 17.86% and bad in 3.5% of cases.
Conclusion
This study presents a successful modified technique of primary closure which allows an extensive en bloc removal of diseased tissues and permits a safe and complete primary closure without undue tension and with respect of cosmetic principles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pilonidal disease is a chronic intermittent disorder of the sacrococcygeal region that most commonly arises in the hair follicles of the natal cleft, affecting predominantly young adults of working age [1]. Many factors were implicated in the etiology as large buttocks with deep natal cleft, family history, prolonged sitting, traveling or driving, excessive body hair, folliculitis at another site, obesity, and poor local hygiene [2]. Evidence suggests that one or more of the following are required for pilonidal sinus formation: tough semi-curved hairs, the deep natal cleft [3], the rolling effect of one buttock surface over the other [4], and the vulnerability of the skin to the insertion of hair at the depth of the natal cleft aided by the stretching forces that occurs during sitting [3].
Pilonidal sinus usually presents as an acute abscess or a chronically discharging painful sinus tract, but irrespective of the mode of presentation, the painful nature of the condition causes significant morbidity with a protracted loss of normal daily activities [1].
Conservative management of pilonidal disease is rarely advocated for other than mild cases, and most of the patients referred to surgeons are offered surgical treatment. However, wound infection, protracted wound healing, wound failure, cosmetic sequelae, and recurrence are problems all too familiar to surgeons engaged in treatment of pilonidal disease [5].
Surgical methods can be broadly categorized as wounds left to heal by open healing or by primary closure, which is further subdivided into midline closure techniques and off-midline closure techniques where the wound is placed outside the midline [1].
The flap repair techniques are crucial and have a major effect on the recurrence rate of the disease by allowing complete and wide excision of the lesion, while filling the resultant soft tissue defect by some means [6]. The aim of most flaps is to use asymmetrical, oblique, elliptical, or lateral incisions in an attempt to keep scars out of the natal cleft [7], leaving deformed buttocks and visible ugly scars. This denotes the cosmetic superiority of the midline scars and the importance of the buttocks as a major component of the concept of beauty in most cultures [5].
The gluteus maximus musculocutaneous flap have been used by many surgeons for reconstruction of sacrococcygeal wounds including after pilonidal sinus excision [8–12].
In this study, the use of a modified gluteal sliding plication closure technique is presented for closure of the defect after complete excision of the pilonidal disease. The aim is to treat the cause of the disease by reshaping the intergluteal anatomy achieving three goals. The first is to achieve complete excision and proper healing with a low rate of recurrence and wound complications. The second is achieving a high patient esthetic satisfaction rate by respecting the cosmetic value and the importance of the buttocks as a major component of the concept of beauty. And, the third is to allow the patient to resume normal daily activities as early as possible.
Anatomy
By definition, the natal cleft is the groove between the buttocks that runs from below the sacrum to the perineum. Laterally, it is bounded by the well-developed panniculous adiposus of the gluteal region, which is characterized by the superficial fascial apron (analogous to the superficial fascial system described by Lockwood) [13].
The gluteus maximus is a type III muscle with transversely oriented fibers. It originates from the fascia of the gluteus medius, the external ilium, the fascia of the erector spinae, the dorsum of the lower sacrum, the coccyx, and the sacrotuberous ligament. Invested by the deep gluteal fascia, it inserts into the iliotibial tract and, to a lesser extent, into the greater trochanter. The nerve supply is by the inferior gluteal nerve alone which enters the deep surface of the muscle near its origin [14]. The blood supply is from the superior and inferior gluteal arteries, which are direct branches of the internal iliac artery. The superior gluteal artery courses above the piriformis muscle to enter the deep surface of the gluteus maximus muscle. The inferior gluteal artery enters the gluteal region through the sciatic foramen and terminates in the lower half of the gluteus maximus muscle. Both arteries enter the muscle approximately 5 cm lateral to the sacral edge [9].
In the sacrum, there are four pairs of posterior sacral foramina on both sides within 2- to 4-cm area of the midline of the sacrum containing branches of the lateral sacral arteries. These may cause some bleeding during elevation of the origin of the gluteus muscle and should be cauterized if encountered [6].
Patients and methods
A total of 56 patients with chronic pilonidal sinus disease were treated using the modified gluteal sliding plication closure technique after excision of the disease. Between the year 2000 and 2008, all patients were operated upon by one surgeon in Kasr Al-Aini hospital (Cairo University), Bani-Suef University Hospital, and in the author's private practice. All patients gave informed consent for the operation and photography. Patients with primary disease and recurrent disease were included in the study, except those who were recurrent after previous flap surgery; these cases were excluded from the study because they have deformed buttocks already. Patients who presented with acute abscess formation were treated first by stab drainage and allowed to fully resolve before definitive surgery if a sinus persists. All excised specimen were tested after excision for completeness of excision and were examined pathologically to ensure the diagnosis and exclude possible rare complications. The outcome measures included complications in the form of wound failure (failure of the skin edges to heal), infection (wound infection was defined as redness and/or edema of the skin and/or discharge), recurrence, seroma formation, and paresthesia or numbness. Functional recovery was estimated by the time the patient was able to resume essential daily activities. In this study, the esthetic satisfaction rate of the patients were assessed after a period of 6 months by questioning the patient to give a grade for his operation as regard the scar and the shape of buttocks on a scale of good, fair, or bad. Follow-up was scheduled monthly for 6 months and every 3 months for 2 years, and then, according to the patient needs.
Surgical technique
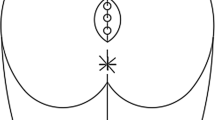
The patient was admitted on the day of surgery. No bowel preparation was necessary. Broad-spectrum antibiotic administration started with induction of anesthesia and continued postoperatively. The operation was carried out under general or spinal anesthesia with the patient in the prone position and the buttocks strapped apart with adhesive tape. All openings injected with methylene blue and hydrogen peroxide to ensure staining of all tracts. The lesion and all its ramifications were excised en bloc by means of an elliptical incision, its long axis in the natal cleft and the lateral borders were over 1 cm away from all sinuses. The incision was carried straight down to the sacral periosteum including the sacrococcygeal fascia and avoiding the deep gluteal fascia which is preserved to withhold suture taken later to approximate the gluteal muscle mass in the midline. Care was taken not to expose any stained tissues and to ensure proper hemostasis after excision. On a side table, the lesion was reinjected with methylene blue to ensure proper excision with no opened tracks (Fig. 1).
The origin of the gluteus maximus over the sacrum was elevated by electrocautery and aided by periosteal elevator to get the proper plane (Fig. 2). Allis clamps were placed on the freed muscle edge, and traction was exerted to test the amount of mobilization achieved (Fig. 3). Dissection continued equally on both sides until the gluteal muscle can be advanced to the midline with little overlap without tension. This is usually achieved by only 2 to 3 cm lateral sharp dissection and then by blunt finger mobilization in order not to injure the pedicle and cause troublesome bleeding. If injury to the vessels became an issue, they can be cauterized or ligated, since the gluteus maximus is a type III muscle with excellent blood supply. However, this has never occurred during our practice. Minimal dissection of the subcutaneous apron from the deep gluteal fascia was done to achieve proper approximation of tissues in the midline. The gluteal muscle mass is then plicated to each other with minimal tension and to the underlying periosteum in the midline with interrupted 0-vicryl suture (Fig. 4a, b). Hemovac suction drain was exited through separate lateral stab wound. The wound was irrigated with saline and garamycine. The subcutaneous fascial apron was reapproximated with interrupted inverted 3-0 vicryl sutures and the skin closed with running subcuticular 3-0 prolene sutures with four to five interrupted sutures (the interrupted sutures were removed by day 5 postoperatively; Fig 5).
A compressive dressing was applied. Postoperatively, the patient ambulated after 24 h and hemovac drain removed after 48 h while pressure dressing was maintained until complete healing of the wound and removal of subcuticular sutures.
Results
The modified gluteal sliding plication closure technique has been used in 56 patients. Forty-one male (73.2%) and 15 females (26.8%), with 23 years median age (range, 17–45 years). Ten cases (18%) were recurrent after previous excision and primary closure done elsewhere, and 46 patients (82%) had de novo disease. Seven cases presented by acute abscess and were treated by stab drainage and allowed to resolve, while the remaining 49 cases presented with chronically discharging sinuses (Table 1). General anesthesia has been used in 33 cases (58.9%) and spinal anesthesia in 23 cases (41.1%) with no cases done under local anesthesia. Defects up to 9 cm in transverse diameter (median, 7 cm; range, 5–9 cm) were closed; the defect was measured after complete excision of all sinuses and diseased tissues and removal of the adhesive tape.
The median follow-up period was 12 months (range, 6–84 months). Forty-seven cases (83.9%) had their functional recovery obtained within 2 weeks, while in nine cases (16.1%) it took more than 2 weeks to be able to resume their necessary daily activities. The median functional recovery was 12 days (range, 10–45 days). In Table 2, the results data are summarized as regards the incidence of each event in male and female patients in relation to their numbers as well as to the total number (Table 2).
Wound infection occurred in six cases (10.7%); four cases suffered mild to moderate infection and were treated conservatively with frequent dressing and antibiotics, while one case did not resolve completely and ended up with a sinus opening in the lower part of the scar and was considered a recurrent disease (1.8%). This case was allowed to heal by conservative measures, and the sinus tract was treated after 3 months with phenol injection.
In one case (1.8%), the infection was severe and associated with seroma due to dislodgement of the drain in the immediate postoperative period. This case necessitated removal of some skin and subcutaneous sutures and treated with frequent dressing of the wound until complete healing achieved in 45 days by secondary intention.
Paresthesia was observed in two cases (3.6%); the patients were reassured, and the symptoms disappeared after nearly 1 year. Seroma accumulation occurred in two cases (3.6%); one of them was treated by aspiration and compression until completely resolved, while the other case was the one who developed severe infection and was treated by open technique. Satisfaction rate as regards the scar site and shape was good in 44 cases (78.57%), fair in ten cases (17.86%), and bad in two cases (3.57%); one of these two cases was the patient who developed severe infection and was treated by open technique which ended up by a hypertrophic scar in the midline. The second case was the patient who developed recurrent disease.
Discussion
Pilonidal sinus is a common acquired disabling disease with variable incidence across countries and races [15]. Although many surgical methods have been proposed from simple laying out to advanced flap mobilization, no clear consensus as to optimal treatment has been reported so far in the literature [16]. In 2007, McCallum et al. [1] published a systemic review and meta-analysis of randomized controlled trials in healing by primary closure versus open healing. They concluded that wounds healed more quickly when primary closure was used but the risk of recurrence was higher than the open healing. A clear benefit was found with off-midline closure compared with midline closure. They advised that the treatment type should be based on surgeon and patient preference, with consideration of the patients' goals for therapy [1]. The cosmetic aspect and esthetic outcome of pilonidal sinus surgery which are major goals for most of patients were rarely studied in the literature. One study by Holmebakk and Nesbakken [5] showed poor results after rhomboidoplasty technique due to the conspicuous scar the patient left with. In this study, not only women were concerned about the cosmetic outcome, but young men were also aware of their look [5]. In another study, 20% of patients were not pleased with the cosmetic appearance of the scar after rhomboid flap for recurrent pilonidal disease [17]. It is obvious that maintaining a midline scar that is thin, strong, non-tender, and pliable is the most esthetically pleasing scar (Fig 6a, b). In this study, we achieved a high satisfaction rate among our patients with 78.57% good cosmetic results, and only 3.57% bad cosmetic results. As the normal relationship of one gluteal mass to the other was preserved, the shape of buttocks was maintained and sometimes improved by tightening of the deep gluteal fascia and the subcutaneous fascial apron. We had no cases left with deformity, asymmetry, and visible crossing or lateral scars.
The method of mobilization of equal bilateral flaps of gluteus maximus muscle was described by Holman in 1946 [18] and adopted by Turner in 1954 for pilonidal sinus primary closure with good results [8]. In 1983, Buchanan and Agris described the technique of gluteal plication closure of sacral pressure ulcer with safe mobilization of the gluteus maximus muscle origin and plication of the muscle in midline [9]. Another modification described by Ramirez, where he limited the dissection to the submuscular plane of the lower portion of muscle origin. This has permitted reconstruction of sacrococcygeal defects up to 12 cm in transverse diameter [10]. Other different techniques have been published about the use of gluteus maximus muscle in the literature as rotational gluteus maximus musculocutaneous flap for recalcitrant pilonidal disease [11, 12], extended split superior gluteus maximus musculocutaneous flap [19], hatchet-shaped gluteus maximus musculocutaneous flap [20], split gluteus maximus island flap [21], and the superior gluteal artery perforator flap [22]. All these techniques did not gain popularity due to the high magnitude of the operations, long operative time, and postoperative severe restrictions. Many authors did not justify the use of such important muscle especially in these healthy young individuals to treat a relatively simple disease.
In our study, the technique used is a more simple direct approach, with minimal blood loss, less operative time, less postoperative restrictions, and no functional abnormality. Even the gluteus muscle is well preserved and can be utilized for major reconstructions if needed. We have used the technique described by Buchanan and Agris [9] with some modifications as limiting the submuscular dissection for 3 cm only and supramuscular dissection for 2 cm to have a good approximation of tissues without endangering the vascular pedicles. Closure of the fascial apron as a separate layer added more strength to the closure line and decreased tension on the skin sutures. We routinely injected methylene blue, which proved to affect both the recurrence and infection rate [23].
In this study, defect size up to 9 cm was closed primarily without tension. Although the sliding gluteus maximus flap can close defects up to 20 cm, but this requires extensive dissection and mobilization of the musculocutaneous unit [10].
Flap techniques have been associated with lower infection and recurrence rates because they flatten the internal cleft with tension-less approximation of tissues after wide and radical removal of all diseased tissues. The results of our study supported these findings with better or comparable results with other techniques. Many authors emphasize the importance of avoiding the midline for closure, and several studies have shown that asymmetrical off-midline closure are superior to midline closure techniques as regarding the infection and recurrence rates [1]. The results achieved in our study do not substantiate these findings. The infection rate is 10.7%, but more important is that all cases were treated conservatively except one case complicated by severe infection due to associated seroma collection. Actually, the presence of muscle flap and proper fascial closure gave the wound more support, tension-free closure, and good blood supply, with no cases of wound disruption or failure in this study. Despite the long-term follow-up, reaching up to 7 years in some cases, the recurrence rate is only 1.8% (one case), which seems to be a promising result for a midline closure technique. In this particular case, it was considered early recurrence [24], despite the fact that the patient did not have a disease-free interval and mostly this was an inadequate excision. But, as it was treated by phenol injection because the patient refused to do another excisional operation, we did not have a pathological confirmation for the nature of recurrence.
In a recent study, the infection rate and recurrence rate in primary closure group were 25%, while wound breakdown was 20%. In flap surgery group in the same study including Limberg, modified Limberg, and adipo-fasciocutaneous flap for coverage, the results were 5% recurrence rate, 5% infection rate, and 5% wound breakdown rate. This study shows better infection rate results than we have achieved but with higher rates of recurrence and wound breakdown [25]. In another study by Lasheen et al., where closure was done by a crossed triangular flap technique, the results were comparable to our results but with a more complicated technique [26]. Osama et al. presented infection rate of 15% and recurrence rate of 10% after rhomboid flap surgery [17].
Other flaps with asymmetric closure line includes Z-plasty [27] and W-plasty [28] aim to reduce the depth of the natal cleft, and avoiding midline scars are associated with a high incidence of flap tip necrosis, unsatisfactory scars, and recurrence rates up to 8%. Fasciocutaneous and cutaneous flaps, such as V-Y flap [29], rhomboid flap [30], bilobed flap [31], S-GAP flap [22], and elliptical rotational flap [32], all have been proposed for recurrent diseases with large defects. These flaps entail massive dissection, sophisticated markings, and ends up by unsightly scars. The recorded recurrence rates for these techniques were 0% to 8%, while morbidity was from 0% to 20%.
Para-median approaches have gained popularity especially in the West. Karydakis described an advancement flap operation with recurrence rate between 1% and 4%, complication rate 9%, and the mean hospital stay is 3 to 4 days [33]. The simple Bascom technique done as an outpatient procedure under local anesthesia and sedation with recorded recurrence rates up to 8% and wound failure reaching 18% [16]. Another technique described by Bascom for advanced and refractory pilonidal disease is the cleft lift procedure, which showed superior results; but again, 9% of cases in his study required a second lift, and 1.5% of cases received a third lift procedure [7].
Paresthesia and seroma collection, which are a common cause of patient discomfort after flap surgery, were minimized in this study to only two cases each by limiting the subcutaneous dissection just above the deep gluteal fascia only for 2 cm and routine closed drainage of the wound.
The term functional recovery has been used in this study instead of time to return to work, as there are many variables affecting the return of patient to his work. What is actually estimated in this study is the time by which the patient is able to resume his daily activities even return to work if does not entail strenuous activities. The median functional recovery was 12 days, where 83.9% of patients were able to resume their activities within 2 weeks. Early return to normal activities is an important outcome, and a clear benefit in these young patients.
The efficacy of any treatment can be judged only after adequate follow-up to establish complete eradication of the disease and to exclude late complications. In this study, there is a long-term follow-up reaching up to 7 years in some cases.
Obvious important factors in the technique adopted in this study were that the excised specimen was double-checked for completeness; the depth of excision included the presacral fascia, while lateral dissection is limited to the minimum needed. The area of the cleft was replaced by an exposed healthy skin with good blood supply provided by the muscle. The bulk of the muscle fills the deep defect created by excision and also obliterated the cleft serving as a cushion under the closure site.
All our patients were instructed to shave the area once weekly and to clean the intergluteal area daily keeping it dry and clean. The separate closure of the fascial apron provided a good secured tension-less closure of the skin with no suture materials placed directly under the skin closure. This flap safety is greater than any other flap technique with simple straightforward technique and full complete preservation of the muscle function, with no need for design, markings, or measurements of the flap.
Conclusion
This procedure lets fat and muscle fall together to create a cushion in the midline, with healthy skin, exposed aerated wound, low morbidity, and high patient esthetic satisfaction rates, respecting the shape of the buttocks, symmetry of the gluteal mass, and minimizing early and late recurrence. These encouraging results need to be confirmed by further prospective randomized trials to compare this technique with para-median incision techniques and asymmetric incision techniques with proper standardization of outcome measures and definitions for postoperative events to allow proper evaluation and assessment of outcome.
References
McCallum IJD, Peter MK, Julie B (2008) Healing by primary closure versus open healing after surgery for pilonidal sinus: systemic review and meta-analysis. BMJ 336:868–871
Raghubir S, Nevil MP (2005) Adipo-fascio-cutaneous flaps in the treatment of pilonidal sinus: experience with 50 cases. Asian J Surg 28(3):198–201
Anyanwa AC, Williams A, Hossain S et al (1998) Karydakis operation for sacrococcygeal pilonidal sinus disease: experience in a District General Hospital. Ann R Coll Surg Engl 80:197–199
Garrido A, Ali R, Ramakrishnan et al (2002) Reconstruction of the natal cleft with a perforator-based flap. Br J Plast Surg 55(8):671–674
Holmebakk T, Nesbakken A (2005) Surgery for pilonidal disease. Scand J Surg 94:43–46
Onishi K, Maruyama Y (2001) Sacral adipofascial turn-over flap for the excisional defect of pilonidal sinus. Plast Reconstr Surg 108(7):2006–2010
Bascom J, Bascom T (2007) Utility of the cleft lift procedure in refractory pilonidal disease. Am J Surg 193:606–609
Turner FP (1954) Pilonidal sinus: primary closure with equal musculofascial flaps and removable far-and-near sutures. Ann Surg 140(5):687–694
Buchanan DL, Agris J (1983) Gluteal plication closure of sacral pressure ulcers. Plast Reconstr Surg 72(1):49–54
Ramirez OM (1990) The sliding plication gluteus maximus musculocutaneous flap for reconstruction of sacrococcygeal wounds. Ann Plast Surg 24(3):223–230
Perez-Gurri JA, Temple WJ, Ketcham AS (1984) Gluteus maximus myocutaneous flap for the treatment of recalcitrant pilonidal disease. Dis Colon Rectum 27(4):262–266
Rosen W, Davidson JS (1996) Gluteus maximus musculocutaneous flap for the treatment of recalcitrant pilonidal disease. Ann Plast Surg 37(3):293–300
Centeno RF, Young VL (2006) Clinical anatomy in aesthetic gluteal body contouring surgery. Clin Plast Surg 33:347–358
Constantino GM (2003) Gluteoplasty. Aesthet Surg J 23(6):441–455
Ertan T, Koc M, Erdal G et al (2005) Does technique alter quality of life after pilonidal sinus surgery? Am J Surg 190:388–392
Nordon IM, Senapati A, Cripps NPJ (2009) A prospective randomized controlled trial of simple Bascom's technique versus Bascom's cleft closure for the treatment of chronic pilonidal disease. Am J Surg 197:189–192
Osama E, Hashish M, Ismail K et al (2009) Outcome of the rhomboid flap for recurrent pilonidal disease. World J Surg 33(5):1064–1068
Holman E (1946) Pilonidal sinus—treatment by primary closure. Surg Gynecol Obstet 83:94
Kishi K, Nakajima H, Imanishi N et al (2008) Extended split superior gluteus maximus musculocutaneous flap and reconstruction after resection of perianal and lower gluteal hidradenitis suppurativa. J Plast Reconstr Aesthet Surg 62:1081–1086
Jósvay J, Sashegyi M, Kelemen P et al (2005) Clinical experience with the hatchet-shaped gluteus maximus musculocutaneous flap. Ann Plast Surg 55(2):179–182
Sharma RK (2001) Split gluteus maximus island flaps for concomitant closure of ischial and sacral pressure sores. Ann Plast Surg 46(1):52–54
Yavuz B, Hakan C, Alper A et al (2008) Reconstruction of extensive pilonidal sinus defects with the use of S-GAP Flaps. Ann Plast Surg 61(2):197–200
Dietrich D, Alexander N, Ronny R et al (2008) Methylene blue halves the long-term recurrence rate in acute pilonidal sinus disease. Int J Colorectal Dis 32:181–187
Dietrich D, Collin MK, Stefan S et al (2007) Time line of recurrence after primary and secondary pilonidal sinus surgery. Dis Colon Rectum 50:1928–1934
Mahdy T (2008) Surgical treatment of the pilonidal disease: primary closure or flap reconstruction after excision. Dis Colon Rectum 51:1816–1822
Lasheen AE, Saad K, Raslan M (2008) Crossed triangular flaps technique for surgical treatment of chronic pilonidal sinus disease. Arch Surg 143(5):503–505
Bose B, Candy J (1970) Radical cure of pilonidal sinus by Z-plasty. Am J Surg 120:783–786
Roth RF, Moorman WL (1977) Treatment of pilonidal sinus and cyst by conservative excision and W-plasty closure. Plast Reconstr Surg 60:412–415
Khatri VP, Espinosa MH, Amin AK (1994) Management of recurrent pilonidal sinus by simple V-Y fasciocutaneous flap. Dis Colon Rectum 37:1532–1535
Azab AS, Kamal MS, Saad RA et al (1984) Radical cure of pilonidal sinus by a transposition rhomboid flap. Br J Surg 71:154–155
El-Khatib HA, Habib BA (2009) A perforator-based bilobed fasciocutaneous flap: an additional tool for primary reconstruction following wide excision of sacrococcygeal pilonidal disease. J Plast Reconstr Aesthet Surg 62:494–498
Gürel N, Cüneyt K, Canbek S (2004) Elliptical rotation flap for pilonidal sinus. Am J Surg 187:300–303
Kitchen PRB (1996) Pilonidal sinus: experience with the Karydakis flap. Br J Surg 83:1452–1455
Acknowledgments
The author thanks Dr. Ahmad Farag, Professor of General Surgery (Cairo University) for reviewing the manuscript and for his assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Shaer, W.M. The modified gluteal sliding plication closure in the treatment of chronic pilonidal sinus. Int J Colorectal Dis 25, 887–894 (2010). https://doi.org/10.1007/s00384-010-0911-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-010-0911-z