Abstract
Background and aims
Bariatric surgery (BS) reduces long-term mortality in comparison with medical treatment of obesity. Some studies indicate that this effect is significant for patients above mean age in different cohorts, but not for younger patients. These findings raise the question whether morbid obese patients should undergo BS as soon as possible, or whether patients might undergo surgery later in their life.
Methods
We performed a post hoc analysis of two studies; we evaluated surgery-related long-term mortality in: (1) the whole cohort [857 surgery patients (163 diabetes) vs. 2086 controls (512 diabetes)]; (2) patients above mean age [> 43 years, 427 surgery patients (133 diabetes) vs. 1054 controls (392 diabetes)]; (3) patients below mean age [≤ 43 years, 432 surgery patients (30 diabetes) vs. 1032 controls (120 diabetes]. Then, we analyzed age-related long-term mortality in the whole cohort, as well as in surgery patients and in controls. Finally, we analyzed incident diseases (diabetes, cardiovascular disease, and cancer) as a function of surgery versus no-surgery and of mean age.
Results
Surgery patients, compared with controls receiving standard medical/dietary treatment, had reduced mortality in the whole cohort (HR = 0.45, 95% CI 0.33–0.62, p = 0.001) and in the study group aged > 43 years (HR = 0.39, 95% CI 0.28–0.56, p = 0.001), but not in the study group aged ≤ 43 years (HR = 0.87, 95% CI 0.42–1.80, p = 0.711). Reduced mortality was observed in non-diabetic and diabetic patients aged > 43 years (HR = 0.37, 95% CI 0.23–0.62, p = 0.001 and HR = 0.45, 95% CI 0.27–0.74, p = 0.002, respectively) who underwent bariatric surgery. In contrast, in patients aged ≤ 43 years, no significant protective effect of bariatric surgery appeared in non-diabetic patients (HR = 0.64, 95% CI 0.24–1.71, p = 0.371), and mortality increased, almost significantly, in diabetic patients aged < 43 years (HR = 2.87, 95% CI 0.96–8.56, p = 0.058), and even more in diabetic patients aged 33–43 years; HR = 4.99, 95% CI 1.18–21.09, p = 0.029). As expected, age-related mortality was increased in the whole cohort (HR = 7.23, 95% CI 5.14–10.17, p = 0.001), in non-diabetic and diabetic controls (HR = 8.55, 95% CI 5.77–12.68, p = 0.001, and HR = 3.76, 95% CI 1.97–7.18, p = 0.001, respectively). The effect of aging was slightly reduced in surgery patients (HR = 3.76, 95% CI 1.87–7.58, p = 0.001), while it was not significant in diabetic surgery patients (HR = 0.70, 95% CI 0.26–1.90, p = 0.88), further emphasizing that diabetes per se has a strong negative effect on survival, also with concomitant bariatric surgery. In a supplementary analysis, HRs did not change when surgery and control parents were matched for the presence of diabetes. Incident diseases (cardiovascular, diabetes, and cancer) were less frequent in surgery than in control patients, irrespective of age.
Conclusion
Bariatric surgery reduces long-term mortality in comparison with medical treatment when performed in patients aged > 43 years, but not in younger patients, where it is neutral or could even increase mortality; reduction in morbidity occurs at any age.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Bariatric surgery is commonly performed in severely obese middle-aged patients, with a mean age of 39 years (16–64 years) [1]. Recently, positive data on bariatric surgery have been published in obese adolescents, so that it has been proposed that “bariatric surgery in severely obese adolescents should be considered standard of care” [2], even though the numbers of interventions performed in the USA appear overall small [3]. On the other hand, obese patients with advanced age (> 50 years or > 60 years) seem to have benefits not different from middle-aged obese patients in terms of resolution of comorbidities [4,5,6].
Bariatric surgery, when compared to medical treatment, reduces long-term mortality in obesity [7, 8]. Data from a few studies indicate that the effect is significant for patients above mean age of cohorts (i.e., aged > 42, or > 43, or > 44 years in different published cohorts), but not for younger patients. This phenomenon seems to be consistent because it has been shown consistently for different procedures such as laparoscopic adjustable gastric banding (LAGB [9] (restrictive), for gastric bypass (RYGB [10] (restrictive/malabsorptive), as well as malabsorptive surgeries (biliopancreatic diversion/Scopinaro procedure [BPD] and biliointestinal bypass [BIBP] together [11]).
These data open the question whether obese patients should undergo bariatric surgery as soon as possible, or whether patients might undergo surgery later in their life, i.e., which should be the best age to perform bariatric surgery. In order to attempt to address this question, we performed a post hoc analysis. In a preliminary set of data, we confirmed that bariatric surgery reduces long-term mortality in comparison with medical treatment of obesity in the whole cohort, and in patients above mean age (> 43 years), but not in patients below mean age (≤ 43 years). Then, we analyzed age-related mortality in obese patients receiving medical treatment of obesity. We found that age-related mortality is elevated in obese diabetic and non-diabetic patients receiving medical treatment of obesity and is reduced by bariatric surgery in non-diabetic patients, but not in diabetic patients, suggesting that bariatric surgery reduces mortality in older patients, likely at higher risk, but can increase mortality in younger patients, likely at lower risk. If confirmed in larger, multicenter, and randomized studies, these data would imply that surgery should be restricted to older patients.
Patients and methods
Two studies performed by the LAGB10 working group were analyzed. One study evaluated long-term mortality in obese patients undergoing LAGB in comparison with obese patients receiving medical treatment of obesity [9]. The other study evaluated long-term mortality in obese patients undergoing malabsorptive surgery (BPD or BIBP) in comparison with obese patients receiving medical treatment of obesity [11].
The two studies were retrospective, had a similar dimension, and were of a similar duration [13.9 ± 1.87 (mean ± SD)] versus [12.1 ± 3.41 years (mean ± SD)]. In both studies series, several patients refused bariatric surgery, mainly because of lack of understanding of potential benefits, fear of surgery and of surgical complications, or inability/unwillingness to comply with the anticipated change of lifestyle habits or with the program of scheduled visits. Patients who declined surgery for any reason, but agreed to be followed up during medical/dietary treatment, were considered controls. In both studies, medical records of obese patients undergoing surgery [(LAGB, n = 385; 52 with diabetes) or no-surgery medical treatment (controls, n = 681; 127 with diabetes)] during the period 1995–2001; [(BPD + BIBP, (n = 472; 111 with diabetes) or no-surgery medical treatment (n = 1405; 385 with diabetes)] during the period 1999–2008] were collected from baseline (visit 1). The mean age of the combined cohorts was 43 years. In both studies, patients were matched for age, sex, BMI, and blood pressure. In the first cohort [9], but not in the second cohort [11], patients with diabetes in the control group were in slight excess as compared with the surgery group; after combining the two cohorts, the number of patients with diabetes was greater in the control group than in the surgery group (p = 0.01). In both studies, identification codes of patients were entered in the Italian National Health System, Lombardy Region database, which contains life status, causes of death, as well as exemptions (proxy of incident diseases) [9, 11,12,13], and hospital admissions from visit 1 to September 2012, and from visit 1 to December 2016, respectively. In both studies, survival was compared across surgery patients and no-surgery patients using Kaplan–Meier plots and Cox regression analyses.
In the Italian National Health System, development of chronic diseases (diabetes mellitus, liver and cardiovascular diseases, cancer, selected thyroid, renal, and lung diseases) yields the right to exemption from medical charges (exemptions), which means life-long free prescriptions and examinations for these diseases [12, 13]. Therefore, the awarding of exemptions can be appropriately considered “bona fide” new cases (incident cases) of chronic diseases.
Outcomes
Death rate among patients (surgery vs. no-surgery), as a function of mean age and of diabetes. Death rate among patients (above and below mean age), as a function of surgery and of diabetes. Exemptions, a proxy of incident diseases, among patients (surgery vs. no-surgery), as a function of mean age. Exemptions among patients (above and below mean age), as a function of surgery. Analysis of survival and that of other outcomes were carried out on an intention-to-treat basis, irrespective of the time of LAGB removal, which occurred generally 5–6 years after its positioning, according to the current guidelines.
Statistical analysis
Data are shown as average values (± SD) for continuous variables or absolute numbers and frequencies for discrete variables. Continuous variables were compared with the Student’s t test. Frequencies were compared with the Fisher exact test. Surgery and no-surgery patients were matched (non-diabetic and diabetic patients separately). Matching was made for sex, age, systolic and diastolic blood pressure, and body mass index. The proportion of dead patients was plotted through Kaplan–Meier curves, and differences in survival among subgroups were tested by the log-rank test. Since control patients had diagnosis of coronary heart disease (CHD) and of diabetes mellitus more frequently than surgery patients, all Kaplan–Meier curves were re-calculated also after a further group matching of surgery and control patients for presence of diabetes.
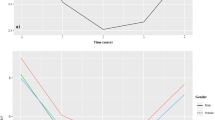
The first set of analysis was aimed at comparing death rates of surgery and no-surgery in the whole cohort of patients, and as a function of mean age and of diabetes mellitus. (The results are given in the text and in Figs. 1 and 2.) The second set of analysis was aimed at comparing death rates linked to mean age in the whole cohort of patients, and as a function of surgery and of diabetes mellitus. (The results are given in the text and in Figs. 3 and 4.)
Effect of surgery on mortality in the whole cohort. Years since visit 1. Patients at risk are indicated at each time interval. a Mortality in surgery and in no-surgery patients. b Mortality in surgery and in no-surgery patients below mean age (≤ 43 years). c Mortality in surgery and in no-surgery patients above mean age (> 43 years)
Effect of surgery on mortality according to mean age (43 years) and to diabetes. a Mortality in non-diabetic surgery and no-surgery patients. b Mortality in non-diabetic surgery and no-surgery patients below mean age (≤ 43 years). c Mortality in non-diabetic surgery and no-surgery patients above mean age (> 43 years). d Mortality in diabetic surgery and no-surgery patients. e Mortality in diabetic surgery and no-surgery patients below mean age (≤ 43 years). f Mortality in diabetic surgery and no-surgery patients above mean age (> 43 years)
Effect of aging on mortality in the whole cohort. a Mortality in patients divided according to mean age (43 years). b Mortality in patients divided according to mean age in the absence of surgery (≤ 43 years). c Mortality in patients divided according to mean age in the presence of surgery (> 43 years)
Effect of aging on mortality according to surgery and to diabetes mellitus. a Mortality in non-diabetic patients divided according to mean age (43 years) in the absence of surgery. b Mortality in non-diabetic patients divided according to mean age (43 years) in the presence of surgery. c Mortality in diabetic patients divided according to mean age (43 years) in the absence of surgery. d Mortality in diabetic patients divided according to mean age (43 years) in the presence of surgery
A multivariable analysis of risk factors for mortality was performed (Cox proportional hazards model) and used to plot Kaplan–Meier curves for surgery versus no-surgery patients; age, mean age, presence of diabetes, female sex, systolic and diastolic blood pressure, estimated glomerular filtration rate (e-GFR), and presence of coronary heart disease (CHD) were entered a priori. Proportionality among the survival rates and attributable factors in the Cox model was assessed by plotting the log [− log (survival function)] versus time. Statistical analyses were performed with STATA 12.0 for MacIntosh.
Power calculation and sample size
Being a retrospective study, power calculation and sample size were only calculated to understand whether the study was meaningful. Due to previous publications on long-term prevention of mortality, demonstrating effectiveness in reducing mortality by approximately 50% in comparison with no-surgery subjects [4, 5], given a power = 80% and an alpha error 0.05, it was calculated that 500 surgery subjects with 30 fatal events and 1000 no-surgery subjects with 90 fatal events would be required to detect significant differences in the outcomes [14, 15]. Similarly, given the high efficacy of bariatric surgeries in the long-term prevention of diabetes and of cancer [16,17,18], we estimated that the occurrence of 100 exemptions in 500 bariatric surgery subjects and 300 exemptions in 1500 subjects undergoing dietary and medical treatment would be necessary to detect significant differences in the outcomes between the two groups [14, 15]. This manuscript was prepared following the guidelines of the STROBE statement [19].
Results
The clinical and metabolic data of patients of the two cohorts pooled together are summarized in Table 1. Minor differences were found, in particular a higher heart rate among surgery patients and a higher frequency of diabetes and of CHD among no-surgery patients. Table 1 also shows clinical and metabolic data after further matching for diabetes. Table 2 summarizes clinical and metabolic data of patients of the two cohorts pooled together, divided according to mean age (> 43 years and < 43 years).
In agreement with previous studies [6,7,8,9,10,11], mortality was higher in no-surgery than in surgery patients (HR = 0.45, 95% CI 0.33–0.62, p = 0.001). Interestingly, the effect of surgery to reduce mortality was significant in patients above mean age (> 43 years, HR = 0.39, 95% CI 0.28–0.56, p = 0.001), while it was not significant in patients below mean age (≤ 43 years, HR = 0.87, 95% CI 0.42–1.80, p = 0.711) (Fig. 1a–c). Also among non-diabetic patients, the protective effect of surgery against mortality was significant in patients above mean age (HR = 0.37, 95% CI 0.23–0.62, p = 0.001), but not significant in patients below mean age (HR = 0.64, 95% CI 0.24–1.71, p = 0.371) (Fig. 2a–c). Among diabetic patients, the protective effect was significant, as for non-diabetic patients, above mean age (HR = 0.45, 95% CI 0.27–0.74, p = 0.002); in contrast, in patients below mean age, there was a nearly significant higher risk (HR = 2.87, 95% CI 0.96–8.56, p = 0.058), with a mortality higher in surgery than in no-surgery patients (Fig. 2d–f). In particular, in diabetic patients aged 33–43 years, mortality was higher in surgery patients [(5/25) than in control patients (3/72), p = 0.029, HR = 4.99, 95% CI 1.18–21.09, p = 0.029). This effect was not different for the two cohorts, i.e., for the different surgeries (data not shown), also because of the small number of deaths. The number of deaths below mean age was very small, for both surgical (n = 9) and no-surgery patients (n = 21, NS); for instance, deaths among diabetic patients were 4 versus 6, respectively (NS), and deaths among non-diabetic patients were 5 and 15, respectively (NS). Analysis of clinical and biochemical variables did not reveal any significant variable possibly related to the differences observed.
Mortality was higher in patients above mean age than in patients below mean age in the whole cohort (HR = 7.23, 95% CI 5.14–10.17) (Fig. 3a). A similar effect was seen among no-surgery patients (HR = 8.55, 95% CI 5.77–12.68) (Fig. 3b), and a reduced effect, still significant, was seen in surgery patients (HR = 3.76, 95% CI 1.87–7.58) (Fig. 3c). A similar effect was seen among non-diabetic patients, with reduction in HR (from HR = 8.89, 95% CI 5.39–14.66, p = 0.001 to HR = 5.04, 95% CI 1.87–13.56, p = 0.001 (Fig. 4a, b). In contrast, among diabetic patients the effect of mean age was significant in the absence of surgery (HR = 3.76, 95% CI 1.97–7.18, p = 0.001) and not significant in the presence of surgery (HR = 0.70, 95% CI 0.26–1.90, p = 0.488) (Fig. 4c, d).
Exemptions, a proxy of incident diseases, were less frequent in surgery than in no-surgery patients, both below and above mean age (Table 2), except for cancer below mean age.
Exemptions were less frequent below than above mean age among surgery and no-surgery patients (Table 3).
Supplemental Table 2 reports risk factors for mortality in the first set of analysis (aimed at comparing death rates of surgery and no-surgery in the whole cohort of patients, as well as a function of diabetes) and in the second set of analysis (comparing death rates linked to mean age in the whole cohort of patients, and as a function of surgery and of diabetes mellitus). The data underline the interplay of age, surgery, sex, and diabetes.
Discussion
Reduction in long-term mortality through bariatric surgery is almost universally acknowledged, with a very few exceptions [20, 21], and this post hoc analysis confirms the results of previous studies performed with restrictive and with malabsorptive surgery [7,8,9,10,11]. Also, as previously suggested, the benefit of bariatric surgery against mortality is restricted to patients above mean age and of interest the fact that in most studies the mean age was around 42–44 years [9,10,11]. Below the mean age, we observed no effect in non-diabetic patients and a possibly negative effect in diabetic patients. One likely explanation for our and others’ findings is that below a given age mortality is too low to detect a possible improvement through bariatric surgery. As a matter of fact, in the SOS study patients aged < 37 years were intentionally excluded because of the low mortality [22, 23].
We also evaluated the effect of age itself on mortality and the effect of bariatric surgery on age-related death. We found that age-related mortality is extremely significant in no-surgery patients and is reduced by surgery in the whole cohort as well as in non-diabetic patients; in contrast, in diabetic patients, age-related mortality was not significant, with a trend (albeit non significant) to worsening of mortality by bariatric surgery. Also for this analysis, the most likely explanation is that, below a given age, mortality is too low to make it possible to detect a possible improvement through bariatric surgery. As a matter of fact, supplemental Table 1A and supplemental Table 1B suggest that the most likely explanation is that aging is accompanied by worsening of health conditions, with a significant increase in risk factors for mortality.
From these data, the question of the best age to perform bariatric surgery, i.e., whether patients should undergo surgery as soon as possible, or whether patients might undergo surgery later in their life, is only partially addressed.
It is tempting to hypothesize that (1) the benefit of bariatric surgery is always present, but is significant only in older patients (likely at higher risk), or (2) the benefit of bariatric surgery exists only in older patients (likely at higher risk). Since mortality was similar (non-diabetic patients) or even greater (diabetic patients) with surgery that with medical treatment in patients below mean age (43 years), the benefit appears to be limited to older patients. Therefore, the concept “the sooner the better” to perform bariatric surgery is not supported by the present analysis. On the contrary, our data suggest that bariatric surgery reduces mortality in aged (high-risk) patients, but is neutral or can increase mortality in younger (low-risk) patients.
In agreement with previous studies [9, 24], exemptions, a proxy of incident diseases, were less frequent in surgery than in no-surgery patients, both below and above mean age (Table 2a), except for cancer below mean age. Exemptions were less frequent below than above mean age among no-surgery patients, and the differences were reduced among surgery patients (Table 2b). This suggests that bariatric surgery prevents incident diseases more than medical treatment; also, the effect of age on incident diseases is reduced by surgery, with no apparent differences between younger and older patients.
The study has limitations/weaknesses and strengths in common with other retrospective studies. Potential weaknesses are: (1) lack of randomization, even though obese patients were from the same cohort, the reason being that in fact, at the beginning of the study, randomization was deemed unethical; (2) most of the information about increased mortality comes from diabetic patients, where low number of deaths which were 4 versus 6, respectively, and among non-diabetic patients were 5 and 15, respectively, i.e., rather small absolute numbers; (3) if we do not consider these deaths, which might seem random event because of the low numerosity, possibly unrelated to surgery or no-surgery, the fact remains that in younger patients there was no beneficial effect of bariatric surgery; (4) treatments received by control patients could not be fully established, even though, through registries of surgeons and the Regional Lombardy Administrative Database, it was possible to ascertain that these patients had no bariatric surgery procedures; (5) even though diabetic patients were in slight excess among no-surgery than surgery patients, the comparisons were made in diabetic and non-diabetic patients separately; on the strength side, (6) HRs were almost identical after matching surgery and control patients for diabetes and this is in line with the finding that patients died much more frequently of cancer (which is significantly associated with obesity) than of cardiovascular diseases (143 vs. 78) [9, 11]; (7) another strength of this study is that it was unbiased, since physicians assigning the diseases exemptions were hundreds and were unaware of the future performance of this retrospective analysis.
The American Diabetes Association suggests that “metabolic surgery should be recommended as an option to treat type 2 diabetes in appropriate surgical candidates with BMI > 40 kg/m2 (BMI > 37.5 in Asian Americas), regardless of the level of glycemic control or complexity of glucose-lowering regimens, and in adults with BMI 35–39.9 kg/m2 (32.5–37.4 in Asian Americans) when hyperglycemia in inadequately controlled despite lifestyle and optimal medical therapy (degree of scientific evidence: A) [25]. Further ADA suggests that “Metabolic surgery should be considered as an option for adults with type 2 diabetes and BMI 30-34.9 kg/m2 (27.5–32.4 kg/m2 in Asian Americans) if hyperglycemia in inadequately controlled despite optimal medical control by either oral or injectable medications (including insulin) (degree of scientific evidence: B) [25]. Other studies have also cautioned on the importance of stringent criteria to perform bariatric surgeries [26, 27]. We would like to emphasize that the importance of age-connected reduction in mortality through bariatric surgery seems to persist even after very long follow-ups, suggesting that this difference is not limited to short follow-ups [28].
We suggest that, based on the present data, which also could be confirmed by larger future multicenter studies, age should also be taken into consideration as an important factor, in the decision whether or not perform bariatric surgery, because of an apparent lack of benefit of bariatric surgery in non-diabetic patients younger than 43 years or even potential harm in performing bariatric surgery in diabetic patients younger than 43 years of age.
Conclusion
While confirming that bariatric surgery reduces long-term mortality in comparison with medical and dietary treatment of obesity, this post hoc analysis indicates that surgery reduces mortality in older (> 43 years old) (likely at high-risk) patients, but has no effect, or it can increase mortality in younger (likely at low-risk) patients. In contrast, reduction in morbidity after bariatric surgery occurs at any age. These results, to be confirmed, require larger studies with longer follow-up periods.
Abbreviations
- BMI:
-
Body mass index
- BG:
-
Blood glucose
- HbA1c:
-
Glycated hemoglobin
- e-GFR:
-
Estimated glomerular filtration rate (ml/min/1.73 m2)
- AST:
-
Aspartate transaminase
- ALT:
-
Alanine transaminase
- CHD:
-
Coronary heart disease
- LAGB:
-
Laparoscopic gastric banding
- RYGB:
-
Gastric bypass
- BPD:
-
Biliopancreatic diversion
- BIBP:
-
Biliointestinal bypass
References
Buchwald H, Avidor Y, Braunwald E et al (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Pratt JSA, Browne A, Browne NT et al (2018) ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis 14:882–901
Campoverde Reyes KJ, Misra M, Lee H, Stanford FC (2018) Weight loss surgery utilization in patients aged 14–25 with severe obesity among several healthcare institutions in the United States. Front Pediatr 6:251
Pontiroli AE, Morabito A, Paganelli M, Saibene A, Busetto L (2013) Metabolic syndrome, hypertension, and diabetes mellitus after gastric banding: the role of aging and of duration of obesity. Surg Obes Relat Dis 9:894–900
Kaplan U, Penner S, Farrokhyar F et al (2018) Bariatric surgery in the elderly is associated with similar surgical risks and significant long-term health benefits. Obes Surg 28:2165–2170
Pontiroli AE, Osio C, Ceriani V, Folli F (2018) Advanced age and success of bariatric surgery. Obes Surg 28:2053
Pontiroli AE, Morabito A (2011) Long-term prevention of mortality in morbid obesity through bariatric surgery. A systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg 253:484–487
Cardoso L, Rodrigues D, Gomes L, Carrilho F (2017) Short- and long-term mortality after bariatric surgery: a systematic review and meta-analysis. Diabetes Obes Metab 19:1223–1232
Pontiroli AE, Zakaria AS, Mantegazza E et al (2016) LAGB10 working group. Long-term mortality and incidence of cardiovascular diseases and type 2 diabetes in diabetic and nondiabetic obese patients undergoing gastric banding: a controlled study. Cardiovasc Diabetol 15:39
Davidson LE, Adams TD, Kim J et al (2016) Association of patient age at gastric bypass surgery with long-term all-cause and cause-specific mortality. JAMA Surg 151:631–637
Ceriani V, Sarro G, Micheletto G et al (2019) On behalf of the LAGB10 working group. Long-term mortality in obese patients undergoing malabsorptive surgery (biliopancreatic diversion and biliointestinal bypass) versus medical treatment. Int J Obes (Lond) 43:1147–1153
www.agenziafarmaco.it, www.epicentro.iss.it/farmaci. Rapporto OSMED 2011, first published 2012. Accessed 22 June 2018
Corrao G, Ibrahim B, Nicotra F et al (2014) Statins and the risk of diabetes: evidence from a large population-based cohort study. Diabetes Care 37:2225–2232
Freedman LS (1982) Tables of the number of patients required in clinical trials using the logrank test. Stat Med 1:121–129
Schoenfeld DA (1983) Sample-size formula for the proportional-hazards regression model. Biometrics 39:499–503
Merlotti C, Morabito A, Pontiroli AE (2014) Prevention of type 2 diabetes; a systematic review and meta-analysis of different intervention strategies. Diabetes Obes Metab 16:719–727
Sjöström L, Gummesson A, Sjöström CD et al (2009) Swedish obese subjects study. Effects of bariatric surgery on cancer incidence in obese patients in Sweden (Swedish Obese Subjects Study): a prospective, controlled intervention trial. Lancet Oncol 10:653–662
Zhou X, Yu J, Li L et al (2016) Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg 26:2590–2601
Vandenbroucke JP, von Elm E, Altman DG et al (2007) STROBE Initiative. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 4:e297
Maciejewski ML, Livingston EH, Smith VA et al (2011) Survival among high-risk patients after bariatric surgery. JAMA 305:2419–2426
Gribsholt SB, Thomsen RW, Svensson E, Richelsen B (2017) Overall and cause-specific mortality after Roux-en-Y gastric bypass surgery: a nationwide cohort study. Surg Obes Relat Dis 13:581–587
Sjöström L, Narbro K, Sjöström CD et al (2007) Swedish obese subjects study. Swedish obese patients study. Effects of bariatric surgery on mortality in Swedish obese patients. N Engl J Med 357:741–752
Sjöström L, Peltonen M, Jacobson P et al (2012) Bariatric surgery and long-term cardiovascular events. JAMA 307:56–65
Pontiroli AE, Ceriani V, Sarro G et al (2019) On behalf of the LAGB10 working group. Incidence of diabetes mellitus, cardiovascular diseases, and cancer in patients undergoing malabsorptive surgery (biliopancreatic diversion and biliointestinal bypass) vs medical treatment. Obes Surg 29:935–942
American Diabetes Association (2018) 7. Obesity management for the treatment of type 2 diabetes: standards of medical care in diabetes 2018. Diabetes Care 41(Suppl. 1):S65–S72
Halpern B, Mancini MC (2019) Metabolic surgery for the treatment of type 2 diabetes inpatients with BMI lower than 35 kg/m2: why caution is still needed? Obes Rev 20:633–647
Craig H, le Roux C, Keogh F, Finucane FM (2018) How ethical is our current delivery of care to patients with severe and complicated obesity? Obes Surg 28:2078–2082
Pontiroli AE, Zakaria AS, Fanchini M et al (2018) A 23-year study of mortality and development of co-morbidities in patients with obesity undergoing bariatric surgery (laparoscopic gastric banding) in comparison with medical treatment of obesity. Cardiovasc Diabetol 29(17):161
Funding
Università degli Studi di Milano, Milano; Ospedale San Paolo, Milano; Istituto Multimedica, Milano; Harvard Medical School, Boston Children’s Hospital; Grant “Ricerca Corrente” to Istituto Multimedica from Ministero della Salute (Ministry of Health), Italy.
Author information
Authors and Affiliations
Contributions
AEP, VC, and IZ planned the research, contributed to discussion, wrote the manuscript; ASZ and AMV searched data, prepared the database, contributed to analysis, and contributed to discussion; ET performed statistical analysis and contributed to discussion; FF searched data, contributed to discussion, and edited the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was funded by Università degli Studi di Milano, Milano; Ospedale San Paolo, Milano; Istituto MultiMedica, Milano; Harvard Medical School, Boston Children’s Hospital; the Grant “Ricerca Corrente” was issued to Istituto MultiMedica from Ministero della Salute (Ministry of Health), Italy.
Informed consent
For this type of study, formal consent is not required.
Additional information
Managed by Massimo Federici.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pontiroli, A.E., Ceriani, V., Tagliabue, E. et al. Bariatric surgery, compared to medical treatment, reduces morbidity at all ages but does not reduce mortality in patients aged < 43 years, especially if diabetes mellitus is present: a post hoc analysis of two retrospective cohort studies. Acta Diabetol 57, 323–333 (2020). https://doi.org/10.1007/s00592-019-01433-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01433-3