Abstract
Aims
To compare the impact of triglyceride–glucose index (TyG-index), the product of fasting plasma glucose (FPG) and triglycerides (TG) with FPG, 2 h post-challenge plasma glucose (2 h-PCPG), TG/high-density lipoprotein cholesterol (TG/HDL-C), and homeostasis model assessment of insulin resistance (HOMA-IR) indices for prediction of type 2 diabetes (T2D) in Iranian adults during a median follow-up of 12 years.
Methods
Study population included 4419 (1858 men) subjects with mean age of 40.6 ± 13.2 years. Multivariable Cox proportional hazard models were used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for each 1-standard deviation increase in each predictor. Areas under the receiver operating characteristics curves (AUC) and 95% CIs were calculated.
Results
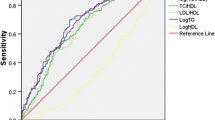
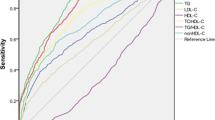
During follow-up, 215 men and 288 women developed T2D. The multivariable HRs for FPG, 2 h-PCPG, TyG-index, HOMA-IR, HOMA2-IR, and TG/HDL-C were 2.20, 1.97, 1.71, 1.33, 1.30, and 1.35 in men and 2.13, 2.11, 1.44, 1.37, 1.32, and 1.36 in women (all P < 0.001). Among the total population, the AUC for FPG [0.752 (0.727–0.776)] was similar to 2 h-PCPG but higher than TyG-index [0.697 (0.673–0.720)], TG/HDL-C [0.644 (0.620–0.669)], HOMA-IR [0.684 (0.659–0.710)], and HOMA2-IR [0.656 (0.630–0.682)]. In men, AUC of TyG-index was higher than TG/HDL-C but did not differ with HOMA-IR indices. In women, the AUC of TyG-index was higher than HOMA2-IR and TG/HDL-C, but was similar to that of HOMA-IR.
Conclusions
FPG is a stronger predictor of T2D than the TyG-index, TG/HDL-C, and HOMA-IR indices. Although TyG-index was better than TG/HDL-C in both genders, it did not rank above HOMA-IR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The high prevalence and incidence of type 2 diabetes (T2D) among Middle Eastern populations, such as Iran, has simultaneously occurred with the increasing trends of obesity and adoption of sedentary lifestyle and Westernization of dietary habits [1,2,3]. T2D is a major risk factor for premature cardiovascular diseases among Iranian adults [4] and the population attributable fraction of diabetes for mortality events is reported to be above 20%, a value higher than those of hypertension and current smoking [5]. It is hence important to identify subjects at high risk of developing T2D for timely prevention and early effective implementation of intervention strategies.
The pathophysiology of T2D is characterized by insulin resistance (IR), the decreased peripheral tissues’ sensitivity to insulin and beta cell dysfunction [6] which are already present years before T2D diagnosis [7]. This theory supports the usefulness of homeostasis model assessment of IR (HOMA-IR) as a valuable and widely used method to measure IR, which aids the prediction of incident diabetes. However, laboratory measurement of serum insulin level is not provided in all healthcare services or is costly for daily practice [8].
Among Iranian adults, a simple model including systolic blood pressure (SBP), family history of diabetes, waist to height ratio (WHtR), triglycerides/high-density lipoprotein cholesterol (TG/HDL-C) and fasting plasma glucose (FPG) was considered superior to depending entirely on the 2 h post-challenge plasma glucose (2 h-PCPG) for identifying individuals at high risk of developing diabetes [9].
Triglyceride–glucose index (TyG-index), the product of FPG and TG has been suggested to be a simple surrogate of IR [10,11,12,13]. A population-based study conducted among Korean adults without T2D, demonstrated the superiority of the TyG-index over HOMA-IR and TG/HDL-C, although no comparison with simple measurement of FPG per se was performed [12]. Two studies, one conducted among high-risk Iranian adults [14] and another in a White European population with normal FPG at baseline [13] showed paradoxical results about the superiority of the TyG-index compared to FPG in prediction of T2D, without any comparison with HOMA-IR indices. In the current study, we extend previous observations by comparing the impact of the TyG-index with IR indices, FPG, TG/HDL-C and 2 h-PCPG for incident diabetes over a decade long follow-up in a population-based cohort study called Tehran Lipid and Glucose Study (TLGS).
Materials and methods
Study participants
TLGS is a dynamic prospective population-based study being conducted on a representative sample of Tehranians recruited from among residents of district 13 of Tehran with the aim of determining the prevalence and incidence of non-communicable disease risk factors and developing and implementing healthy lifestyle. Age distribution of the TLGS population at baseline, is representative of the overall population of Tehran (Iran National Census, 1996). Data collection is ongoing, designed to continue for at least 20 years with approximately 3-year intervals [15]. Details of the study methods including the study participants, collection and documentation of medical history and demographic data, clinical examinations, blood sample collections and laboratory evaluations have been explained elsewhere; these are repeated using same methods in every phase of TLGS [15].
Current study used the data from 5437 subjects, aged ≥ 20 years, who had baseline serum insulin measurement.
Participants with prevalent T2D (n = 557), missing data on glucose status (n = 277), and other covariates (n = 184) were excluded, resulting in a total of 4419 (1858 men) individuals, who had had at least one follow-up visit until January 2015 (Fig. 1). Written informed consent was obtained from all participants, and the ethics committee of Research Institute for Endocrine Sciences (RIES) approved the study.
Clinical, anthropometric, and laboratory measurements
Using a pretested questionnaire, a trained interviewer collected data which included demographic information, family history of diabetes, education status, and drug history. Methods of clinical measurements including body weight, height, waist circumference (WC), systolic and diastolic blood pressures have been reported elsewhere [1]. Body mass index (BMI) was calculated as the body weight (kg) divided by the square of body height (m2).
A blood sample was taken between 7∶00 and 9∶00 a.m. from all study participants, after 12–14 h overnight fasting. All the blood analyses were carried out at the TLGS research laboratory on the day of blood collection. The standard oral glucose tolerance test (OGTT) was performed for all subjects, aged ≥ 20 years, not on glucose-lowering drugs. FPG and 2 h-PCPG were measured using an enzymatic colorimetric method with glucose oxidase; inter- and intra-assay coefficients of variation (CV) at baseline and follow-up phases were both less than < 2.3%.
TG was assayed using an enzymatic colorimetric method with glycerol phosphate oxidase. HDL-C was measured after precipitation of the apolipoprotein B containing lipoproteins with phosphotungistic acid. Both intra- and inter-assay CVs were below 2.1 and 3.0% for TG and HDL-C, respectively, in all baseline and follow-up assays. Analyses were performed using Pars Azmon kits (Pars Azmon Inc., Tehran, Iran) and a Selectra 2 auto-analyzer (Vital Scientific, Spankeren, Netherlands). All samples were analyzed when internal quality control met the acceptable criteria.
Fasting serum insulin was analyzed by the electrochemiluminescence immunoassay method, using Roche Diagnostic’s kits and a Roche/Hitachi Cobas e-411 analyzer (Roche GmbH, Mannheim, Germany). Lyophilized quality control materials (Lyophochek Immunoassay Plus Control, Bio-Rad Laboratories, Irvin, CA, USA) were used to monitor the accuracy of the assays; intra- and inter-assay CVs were 1.2 and 3.5%, respectively.
Definition of terms
The diagnosis of T2D was defined as meeting at least one of the following criteria: FPG ≥ 7 mmol/L; 2 h-PCPG ≥ 11.1 mmol/L or taking anti-diabetic medications. Having at least one parent or sibling with T2D was defined as a positive family history of diabetes. Education was categorized according to self-reported data into three groups: illiterate or below 6 years, 6–12 years, and over 12 years of education. The TyG-index was calculated for each participant using the ln [fasting TG (mg/dL) × FPG (mg/dL)/2] [10,11,12,13]. IR indices included HOMA-IR calculated as: FPG (mmol/L) × fasting serum insulin (µU/mL)/22.5; and an updated HOMA model (HOMA2-IR) calculated by the HOMA2 calculator for specific insulin version 2.2.3 available from http://www.dtu.ox.ac.uk/homacalculator using fasting glucose and fasting insulin in a steady-state condition [fasting glucose: 3–25 mmol/L and fasting insulin: 2.88– 43.16 µU/mL(20–300-pmol/L)] [16].
Statistical analysis
Continuous variables are expressed as the mean ± standard deviation (SD) or interquartile range for normal and skewed distributed variables, respectively, and percentages for categorical variables. Comparisons of baseline characteristics between men and women were performed using independent samples t test, Mann–Whitney test, and Pearson’s Chi-squared test as appropriate.
We conducted a Cox proportional hazard analysis to estimate the hazard ratios (HRs) and their 95% confidence interval (CI) of T2D per 1-SD increase in FPG, 2 h-PCPG, TG/HDL-C, HOMA-IR, HOMA2-IR and TyG-index. The event date for the failed cases was defined as the mid-time between the date of follow-up visit at which the T2D was first diagnosed, and the most recent follow-up visit before diagnosis; the follow-up time was drawn from the difference between the calculated mid-time date and the date on which the subject entered the study. We fitted both age and multivariate adjusted models controlling for age (continuous) and sex (in pooled sample), BMI, WC, SBP, TG/HDL-C (for all exposures excluding TG/HDL-C) and HDL-C only for TyG-index, anti-hypertensive medications, education (below 6 years as reference) and family history of diabetes, the main cofounders which were shown for incident T2D among Iranian populations [1]. The proportional hazards assumption in the Cox model was assessed with the Schoenfeld residual test and all proportionality assumptions were appropriate. Areas under curve (AUC) of the receiver operating characteristics (ROC) curves and their 95% CI were calculated and all six exposures were compared using the Delong test [17], to assess their predictive powers. Statistical analyses were performed using SPSS for windows version 20 and STATA version 14 and P value below 0.05 considered statistically significant.
Results
The study population included 4419 individuals (men = 1858), with mean age 40.6 ± 13.2 years. Table 1 illustrates the basic characteristics of the study participants; men were older, more educated and had higher WC, systolic and diastolic blood pressures, FPG, TG and TyG-index; however, they had lower BMI, HDL-C, serum insulin, HOMA-IR indices and 2 h-PCPG.
During a median follow-up of 12.0 years, there were 215 and 288 incident cases of T2D among men and women, respectively; corresponding incidence rates were 10.51 (95% CI 9.20–12.0) and 9.92 (95% CI 8.84–11.1) per 1000 person-years of follow-up.
Since significant interaction was found only between HOMA-IR and sex (P = 0.04), all analyses were sex-stratified. Furthermore, for comparing our findings with other studies in this field we performed sex-adjusted analysis. As shown in Table 2, each 1-SD increase in FPG, 2 h-PCPG, TyG-index, HOMA-IR, HOMA2-IR, and TG/HDL-C in both genders was significantly associated with T2D in multivariate analyses; corresponding values for men were 2.20 (95% CI 1.93–2.50), 1.97 (1.73–2.25), 1.71 (1.47–1.98), 1.33 (1.21–1.46), 1.30 (1.16–1.45), and 1.35 (1.17–1.56); and for women were 2.13 (1.90–2.38), 2.11 (1.89–2.35), 1.44 (1.25–1.66), 1.37 (1.26–1.49), 1.32 (1.20–1.44), and 1.36 (1.20–1.53), respectively (all P values < 0.001).
Figure 2 shows the ROC curves of FPG, 2 h-PCPG, TyG-index, TG/HDL-C, HOMA-IR, and HOMA2-IR, for incident T2D in each gender. Among men (Fig. 2a), the AUC for FPG [0.756 (0.720–0.793)] was similar to 2 h-PCPG [0.721 (0.681–0.761)] but significantly higher than the TyG-index [0.686 (0.650–0.722)], HOMA-IR [0.671 (0.631–0.712)], HOMA2-IR [0.645 (0.604–0.687)], and TG/HDL-C [0.627 (0.588–0.664)]; however, the AUC of the TyG-index was significantly higher than TG/HDL-C but there was no difference between AUC of the TyG-index compared with HOMA-IR indices. Regarding women (Fig. 2b), similar to men, AUC for FPG [0.749 (0.716–0.781)] was similar to 2 h-PCPG [0.756 (0.624–0.788)], values which were significantly higher than the TyG-index [0.707 (0.677–0.737)], HOMA-IR [0.697 (0.665–0.729)], HOMA2-IR [0.667 (0.634–0.700)], and TG/HDL-C [0.662 (0.629–0.694)]. Among women, the AUC of the TyG-index was significantly higher than HOMA2-IR and TG/HDL-C but similar to HOMA-IR. Similar to both genders, in the total population (Fig. 2c), the AUC for FPG [0.752 (0.727–0.776)] was similar to 2 h-PCPG [0.740 (0.714–0.765)] but significantly higher than the TyG-index [0.697 (0.673–0.720)], TG/HDL-C [0.644 (0.620–0.669)], HOMA-IR [0.684 (0.659–0.710)], and HOMA2-IR [0.656 (0.630–0.682)].
Discussion
During more than a decade long follow-up, among an adult Iranian population, we examined the impact of FPG, 2 h-PCPG, TG/HDL-C, TyG-index, and HOMA-IR indices for incident T2D. Accordingly, each 1-SD increase in any of these parameters was significantly associated with incident T2D, independent of major traditional risk factors, HRs ranged from 1.30 for HOMA2-IR to 2.20 for FPG among men; corresponding values for women were 1.32 and 2.13, respectively. Regarding discriminatory powers as shown by AUC, among men the highest AUC was attributable to FPG, i.e., ≈ 76% (which was similar to 2 h-PCPG), and there was no superiority for TyG-index compared with HOMA-IR indices. In women, FPG and 2 h-PCPG had similar AUC (≈ 75%) which was higher than TyG-index and HOMA-IR indices, however, the TyG-index showed higher discriminatory power compared to the HOMA2-IR. Using data of fasting insulin and FPG levels, in 1985 Matthews et al. proposed HOMA-IR as an index to examine IR state [18]. Guerrero-Romero et al. recommended TyG-index as a simple and inexpensive tool for identification of individuals at risk of IR. They also applied hyperinsulinemic-euglycemic clamp test and showed that TyG-index was moderately associated with IR among both obese and non-obese as well as subjects with and without T2D [19]. Abassi et al. showed TyG-index has a relatively modest and comparable relationship with steady-state plasma glucose (SSPG) concentration during the insulin suppression test in subjects without T2D; actually, they found calculations of the TG/HDL-C ratio and the TyG-index correlated with SSPG concentration to a similar degree, and the associations were comparable to estimates using fasting insulin [11].
A few studies conducted among East Asians, European populations and one study among Iranian first degree relatives of patients with T2D, examined the association between the TyG-index and incident T2D. In the first study conducted in Korean adults (mean age 61.6 years) free of diabetes and pre-diabetes at baseline, it was shown that the TyG-index was better than other IR indices such as HOMA-IR or TG/HDL-C for identifying those at risk of T2D; in their data analysis, the AUC of TyG-index (0.645) was significantly higher than those of TG/HDL-C (0.609) and HOMA-IR (0.592) [12]. In another study conducted among younger Korean subjects (mean age 44 years), it was shown that baseline TyG-index was significantly associated with incident T2D, regardless of obesity status [20]. In a White European population, it was shown that 1-SD increment in the TyG-index was associated with 54% increase in risk of T2D in multivariate analysis, a risk that was highlighted in all metabolic health categories [21]; in this cohort with normal FPG at baseline the AUC of TyG-index, FPG, and TG were 0.75, 0.66, and 0.71, respectively [13]. In a recent population-based study conducted among rural Chinese subjects with normal weight, increasing TyG-index was also associated with incident T2D, although the AUC of TyG-index was not better than WC or WHtR among men [22]. In contrast to the above studies in our data analysis, FPG and 2 h-PCPG appeared to be more reliable predictors of T2D than TyG-index, HOMA-IR indices and TG/HDL-C. Altogether, TG/HDL-C seemed to be a weak predictor for incident T2D in the current study. Furthermore, Akour et al. demonstrated that the level of TG/HDL-C was comparable between pre-diabetes/T2D and normoglycemic groups in Jordanian population [23]. On the other hand, Wang et al. reported that 2 h-PCPG had higher AUC compared to FPG (≈ 93% vs 87%) among Chinese population [24]; the finding that highlights important role of ethnicity difference. Among different risk factors of incident T2D, using multivariate analysis, we showed a 1 mmol/L increase in FPG was associated with more than a threefold risk [3.39 (2.93–3.91)], a value that cannot be attributed to changes in TG [1.05 (0.99–1.10)], 2 h-PCPG [1.42 (1.35–1.49)] and positive family history of diabetes [1.64 (1.40–1.92)] [1]. Furthermore, we also showed that FPG level as low as 5.0–5.5 mmol/L was a stronger predictor of T2D than other risk factors [9]. Hence, it is possible that using TyG-index as a surrogate of IR by multiplying FPG and TG, weakened the impact of FPG for incident T2D.
To predict incident T2D, regardless of superiority of FPG to other measures, considering different surrogates of IR, we confirmed the superiority of the TyG-index over HOMA2-IR only among women; however, we found no difference between AUC of HOMA-IR and TyG-index in either gender. Superiority of the TyG-index over HOMA2-IR (AUC of 0.79 vs 0.77) was also reported in a cross-sectional study conducted on 82 Brazilian subjects [25]. In postmenopausal women without T2D from the Montreal-Ottawa New Emerging team population database it was shown that the TyG-index and insulin sensitivity/resistance indices were only modestly related to the hyperinsulinemic–euglycemic clamp test and both fasting and OGTT derived surrogate indices appeared to be more precise in estimating insulin sensitivity/resistance [26].
As regards to limitations, first, since we only had data for fasting insulin, we had to use the fasting indices of IR, which are not as accurate as using both fasting and 2 h post-challenge levels of insulin. Second, as inherent to any prospective study, levels of baseline risk factors might change during the follow-up. Third, we had no data on other biomarkers such as glycosylated hemoglobin (HbA1C) and 1 h-PCPG, which has been recently reported to be superior to HbA1C for detecting those at risk of T2D [27]. In a systematic review evaluating predictive values of 94 suggested risk models for incident T2D, it has been shown that more than 80 models included available clinical parameters and simple low cost laboratory biomarkers, which were similar to components of our models and only few studies included haematological parameters (such as white blood cell count) or other biochemical markers (such as uric acid, C-reactive protein, HbA1C, or adipokines); the markers which were also not included in 7 diabetes risk models (scores) that are potential for adaptation for use in routine clinical practice [28]. As the last limitation, the present study was conducted among Persian ethnicities resident in Tehran with high prevalence and incidence of T2D [1, 29]; however, it remains to be determined if our findings are applicable to other ethnicities with different risk for T2D. The strengths of the current study include: its large sample size, population-based design, long-term follow-up, and comparing the TyG-index with FPG, 2 h-PCPG, TG/HDL-C, and HOMA- IR indices in both genders.
To conclude, among Iranian populations using FPG as a simple, low cost test shows it to be the strongest predictor of T2D compared to different surrogates of IR including TyG-index, TG/HDL-C, and HOMA-IR indices. Although the TyG-index was better than TG/HDL-C in both genders and HOMA2-IR in women, it did not rank higher to HOMA-IR in prediction of T2D.
References
Derakhshan A, Sardarinia M, Khalili D, Momenan AA, Azizi F, Hadaegh F (2014) Sex specific incidence rates of type 2 diabetes and its risk factors over 9 years of follow-up: Tehran Lipid and Glucose Study. PLoS One 9:e102563
Guariguata L (2012) By the numbers: new estimates from the IDF Diabetes Atlas Update for 2012. Diabetes Res Clin Pract 98:524–525
Ghassemi H, Harrison G, Mohammad K (2002) An accelerated nutrition transition in Iran. Public Health Nutr 5:149–155
Eslami A, Mozaffary A, Derakhshan A, Azizi F, Khalili D, Hadaegh F (2017) Sex-specific incidence rates and risk factors of premature cardiovascular disease. A long term follow up of the Tehran Lipid and Glucose Study. Int J Cardiol 227:826–832
Sardarinia M, Akbarpour S, Lotfaliany M, et al (2016) Risk factors for incidence of cardiovascular diseases and all-cause mortality in a middle eastern population over a decade follow-up: Tehran Lipid and Glucose Study. PLoS One 11:e0167623
Kahn S (2003) The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia 46:3–19
Warram JH, Martin BC, Krolewski AS, Soeldner JS, Kahn CR (1990) Slow glucose removal rate and hyperinsulinemia precede the development of type II diabetes in the offspring of diabetic parents. Ann Internal Med 113:909–915
Wallace TM, Levy JC, Matthews DR (2004) Use and abuse of HOMA modeling. Diabetes Care 27:1487–1495
Bozorgmanesh M, Hadaegh F, Ghaffari S, Harati H, Azizi F (2010) A simple risk score effectively predicted type 2 diabetes in Iranian adult population: population-based cohort study. Eur J Public Health 21:554–559
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F (2008) The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metabol Syndrome Relat Disord 6:299–304
Abbasi F, Reaven GM (2011) Comparison of two methods using plasma triglyceride concentration as a surrogate estimate of insulin action in nondiabetic subjects: triglycerides × glucose versus triglyceride/high-density lipoprotein cholesterol. Metabolism 60:1673–1676
Lee S-H, Kwon H-S, Park Y-M, Ha H-S, Jeong SH, Yang HK et al (2014) Predicting the development of diabetes using the product of triglycerides and glucose: the Chungju Metabolic Disease Cohort (CMC) study. PLoS One 9:e90430
Navarro-González D, Sánchez-Íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez JA (2016) Triglyceride–glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: the Vascular-Metabolic CUN cohort. Prev Med 86:99–105
Janghorbani M, Almasi SZ, Amini M (2015) The product of triglycerides and glucose in comparison with fasting plasma glucose did not improve diabetes prediction. Acta Diabetol 52:781–788
Azizi F, Ghanbarian A, Momenan AA, Hadaegh F, Mirmiran P, Hedayati M et al (2009) Prevention of non-communicable disease in a population in nutrition transition: Tehran Lipid and Glucose Study phase II. Trials 10:5
Ghasemi A, Tohidi M, Derakhshan A, Hasheminia M, Azizi F, Hadaegh F (2015) Cut-off points of homeostasis model assessment of insulin resistance, beta-cell function, and fasting serum insulin to identify future type 2 diabetes: Tehran Lipid and Glucose Study. Acta Diabetol 52:905–915
Unger G, Benozzi SF, Perruzza F, Pennacchiotti GL (2014) Triglycerides and glucose index: a useful indicator of insulin resistance. Endocrinología y Nutrición (English Edition) 61:533–540
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R (1985) Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Guerrero-Romero F, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Ramos-Zavala MAG, Hernández-González SO et al (2010) The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic clamp. J Clin Endocrinol Metabol 95:3347–3351
Lee ES, Kim JH, Park SE, Park C-Y, Oh K-W, Park S-W et al (2016) Predictive value of triglyceride glucose index for the risk of incident diabetes: a 4-year Retrospective Longitudinal Study. PLoS One 11:e0163465
Navarro-González D, Sánchez-Íñigo L, Fernández-Montero A, Pastrana-Delgado J, Martinez JA (2016) TyG Index change is more determinant for forecasting type 2 diabetes onset than weight gain. Medicine 95:e3646
Zhang M, Wang B, Liu Y, Sun X, Luo X, Wang C et al (2017) Cumulative increased risk of incident type 2 diabetes mellitus with increasing triglyceride glucose index in normal-weight people: the Rural Chinese Cohort Study. Cardiovasc Diabetol 16:30
Akour A, Kasabri V, Boulatova N, Bustanji Y, Naffa R, Hyasat D et al (2017) Levels of metabolic markers in drug-naive prediabetic and type 2 diabetic patients. Acta Diabetol 54:163–170
Wang Y, Yuan Y, Zhang Y, Lei C, Zhou Y, He J et al (2017) Serum 1, 5-anhydroglucitol level as a screening tool for diabetes mellitus in a community-based population at high risk of diabetes. Acta Diabetol 54:425–431
Vasques ACJ, Novaes FS, de Oliveira MdS, Souza JRM, Yamanaka A, Pareja JC et al (2011) TyG index performs better than HOMA in a Brazilian population: a hyperglycemic clamp validated study. Diabetes Res Clin Pract 93:e98–e100
Bastard JP, Lavoie ME, Messier V, Prud’homme D, Rabasa-Lhoret R (2012) Evaluation of two new surrogate indices including parameters not using insulin to assess insulin sensitivity/resistance in non-diabetic postmenopausal women: a MONET group study. Diabetes Metabol 38:258–263
Jagannathan R, Sevick MA, Fink D, Dankner R, Chetrit A, Roth J et al (2016) The 1-hour post-load glucose level is more effective than HbA1c for screening dysglycemia. Acta Diabetol 53:543–550
Noble D, Mathur R, Dent T, Meads C, Greenhalgh T (2011) Risk models and scores for type 2 diabetes: systematic review. BMJ 343:d7163
Hadaegh F, Bozorgmanesh MR, Ghasemi A, Harati H, Saadat N, Azizi F (2008) High prevalence of undiagnosed diabetes and abnormal glucose tolerance in the Iranian urban population: Tehran Lipid and Glucose Study. BMC Public Health 8:176
Acknowledgements
The authors wish to thank the study participants for their enthusiastic cooperation. We would also like to acknowledge Ms. Niloofar Shiva, for critical editing of English grammar and syntax of the manuscript. This manuscript is the result of the MD thesis of Dr Aidin Baghbani-Oskouei.
Funding
This study was supported in part by grant No. 12545-2 from the Shahid Beheshti University of Medical Sciences and by grant No. 121 from the National Research Council of the Islamic Republic of Iran.
Author information
Authors and Affiliations
Contributions
MT, ABO, FH, and FA participated in the conception and design of the study; MT, ABO, and NA carried out the literature search and participated in data collection and analysis; FH, MT, ABO, and NA participated in interpretation of analysis and writing the manuscript; FA and FH participated in final approval of the version to be submitted. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Managed by Massimo Porta.
Rights and permissions
About this article
Cite this article
Tohidi, M., Baghbani-Oskouei, A., Ahanchi, N. et al. Fasting plasma glucose is a stronger predictor of diabetes than triglyceride–glucose index, triglycerides/high-density lipoprotein cholesterol, and homeostasis model assessment of insulin resistance: Tehran Lipid and Glucose Study. Acta Diabetol 55, 1067–1074 (2018). https://doi.org/10.1007/s00592-018-1195-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1195-y