Abstract
Purpose
The minimally invasive Chevron-Akin (MICA) is considered the third generation of minimally invasive hallux valgus (HV) surgery, and its original description included fixation of the Akin osteotomy with a screw. The aim of this study is to evaluate a series of patients undergoing HV correction using the MICA technique without screw fixation of the Akin osteotomy.
Methods
We retrospectively evaluated 58 consecutive patients who underwent surgical correction for HV between August 2018 and March 2020. A total of 69 feet were evaluated with a minimum follow-up of 2 years. Clinical outcomes such as pain (VAS), function (AOFAS), range of movement, criteria personal satisfaction and complications were evaluated.
Results
The AOFAS score (mean ± standard deviation) significantly improved from 57.0 ± 8.6 preoperatively to 93.9 ± 8.7 postoperatively (p < .001) with a minimum follow-up of 2 years. The VAS score improved from 6.0 ± 1.8 preoperatively to 0.6 ± 1.4 at 2-year follow-up (p < .001), and the hallux valgus angle reduced from 39.7 ± 6.9 to 8.9 ± 9.0 (p < .001). The majority of patients (95.6%) reported the result as excellent or good, and the most common complication was the need to remove the screw (7.2%).
Conclusions
The use of MICA without Akin osteotomy fixation resulted in successful correction of hallux valgus with improvements in clinical and radiographic parameters.
Level of evidence
IV, case series.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Several published studies show that the third generation of the minimally invasive Chevron-Akin technique (MICA) is a technique that presents good clinical and radiographic results in hallux valgus (HV) correction, comparable to open surgery, but with smaller scars and a less painful postoperative period [1,2,3,4,5,6,7].
The technique described by Redfern and Vernois consists of an extracapsular osteotomy in the neck of the first metatarsal associated with an Akin osteotomy, both of which are fixed with screws [8]. In an Akin osteotomy, a medial wedge is removed from the proximal phalanx of the hallux in order to correct the deforming forces of the flexor hallucis longus and extensor hallucis longus tendons [9].
It is still under discussion whether Akin fixation is mandatory and indeed what form of fixation would be the gold standard. Studies have been published on the outcomes of Akin osteotomies without fixation associated with open and minimally invasive techniques, with good results [10, 11].
Fixing the osteotomy increases the cost and surgical time, but on the other hand, it allows mobilization of the hallux earlier and reduces the chance of malunion of the osteotomy. Not fixing the Akin osteotomy, in addition to the advantages already mentioned, allows some accommodation of the hallux correction in the postoperative dressings if the surgeon deems it necessary.
The objective of this study is to evaluate a series of patients who underwent HV correction using the MICA technique without fixation of the Akin osteotomy.
Methods
Study design
This is a retrospective case series of consecutive patients diagnosed with HV who underwent surgical correction using the MICA technique. All patients were operated on in the same center and by the same team of surgeons experienced in minimally invasive surgery (M.V.P.F., G.F.F.) based in São Paulo, Brazil. The surgical procedure was only recommended after failure of conservative treatment with a change of shoes, physiotherapy and specific guidelines.
Ethical approval
We adhered to the Declaration of Helsinki and the Guidelines for Good Clinical Practice in conducting this study, which was approved by the local ethics committee. Only patients who had read, agreed to and signed the informed consent form were included. Additionally, we reported this study in accordance with the STROBE guidelines for reporting of observational studies [12].
Participants
Inclusion criteria were: 1) Patients aged 18 years or older; 2) moderate or severe hallux valgus: hallux valgus angle (HVA) > 20 or 1–2 intermetatarsal angle (IMA) > 11; and 3) patients undergoing surgical correction using the MICA technique with a minimum follow-up of 2 years.
Patients with previous degenerative lesions in the foot or ankle or previous surgeries and sequelae of fractures of the tibial pilon, ankle and foot were excluded. Patients with additional surgeries such as percutaneous osteotomy of the metatarsals and percutaneous correction of the smaller toes were included.
Outcome measures
This study evaluated clinical and radiographic outcomes. The pain visual analog scale (VAS) and the American Orthopedic Foot and Ankle Society (AOFAS) Great Toe Metatarsophalangeal-Interphalangeal Scale scoring system were used to assess clinical outcomes pre- and postoperatively [13]. We also performed an evaluation of the range of motion (ROM) before and after the surgical procedure.
The radiographic evaluation was performed through six angles measured on the anteroposterior radiograph of the weight-bearing foot: hallux valgus angle (HVA), intermetatarsal angles between the first and second rays (IMA), the intermetatarsal angle between the proximal fragment of the osteotomy and the second ray (IAPF), the hallux interphalangeus angle (HIA) denotes the angular measurement formed between the midshaft axis of the proximal and distal phalanges, the proximal phalangeal articular angle (PPAA), which is formed by the midshaft axis of the proximal phalanx and the line running through the edges of the proximal articular surface of the phalanx and the proximal to distal phalangeal articular angle (PDPAA), which is the angle formed by tangential lines to the proximal and distal phalangeal articular surfaces.
The HIA, PPAA and PDPAA angles were only evaluated in the postoperative period due to the high degree of hallux pronation and the risk of measurement bias [14].
On lateral radiographs, we evaluated the angle between the proximal and distal fragments of the Akin osteotomy. Furthermore, the bone consolidation of osteotomies was considered in the last medical evaluation of patients included in the study.
The Coughlin score was used to evaluate the final outcome of personal satisfaction [15]. The questionnaire was used at the last visit of the study participant, and the score is divided into four grades: excellent, good, fair and poor. We also asked the patient if they could go back in time would they have maintained the decision to undergo the surgical procedure.
Data collection
We retrospectively identified consecutive patients who underwent MICA for moderate and severe hallux valgus between August 2018 and March 2020 from a prospective database. The authors of this study summoned and evaluated patients in person.
Study data were collected and managed using REDCap electronic data capture tools hosted at the Instituto Prevent Senior [16]. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing: 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.
Surgical procedure and postoperative protocol
The patients underwent the surgical procedure in the supine position, without the use of a tourniquet, and the anesthesia used was spinal anesthesia with sedation (institutional protocol). All patients were admitted and discharged on the same day (day-hospital).
Chevron osteotomy
The operative technique was third-generation MICA as described by Redfern and Vernois [8]. An extra-articular Chevron osteotomy was performed proximal to the metatarsal head with a 2.2 mm Shannon burr. The distal fragment was pushed to the lateral region with a periosteum reamer for percutaneous surgery, seeking to correct pronation, varus and flexion–extension. The osteotomy was then fixed with two 3.5 mm cannulated screws (beveled or conical headless) from the metatarsal base to the distal fragment. The medial prominence was removed or a closing wedge was performed, according to the technique described by Ferreira et al. [17].
Akin osteotomy without fixation
The Akin osteotomy starts with a 2 mm incision in the region of the base of the proximal phalanx, close to the metatarsophalangeal joint. Thus, the osteotomy is performed with a 2.2 mm Shannon burr under radioscopy visualization. The burr is directed dorsally and plantarly, preserving the lateral cortex. Finally, the maneuver is performed with the hands to close the wedge. No fixing is done (Fig. 1), and the osteotomy is stabilized with a surgical dressing at the end of the procedure.
Minimally invasive lateral release
The decision to perform percutaneous soft tissue release was made intraoperatively after completion of the MICA technique. The additional procedure was performed when the surgeon judged that the big toe still had a clinical tendency to valgus.
Closure
Finally, the surgical incisions should be washed with saline solution and the skin sutured with 4-0 nylon. A dressing with sterile gauze is performed, and then an elastic bandage is made.
Postoperative care
After the surgical procedure, patients were instructed to start full weight bearing immediately using rigid-sole sandals for at least six weeks. The dressing was changed weekly by the medical team for three weeks, and then the patient uses a toes separator until completing six weeks (Fig. 2).
Statistical data analysis
Statistical analysis was conducted using the Stats package of R [18]. Numerical variables were summarized using mean, standard deviation, maximum and minimum values, while nominal variables were analyzed using descriptive statistics. The Shapiro test was used to determine whether the data were parametric or nonparametric, and the means were compared using either the Wilcoxon Sign Rank or Student’s T test [19]. A statistical level of evidence of p ≤ 0.05 was considered significant.
Results
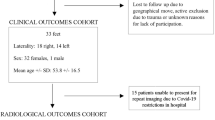
Between August 2018 and March 2020, 101 patients diagnosed with moderate or severe hallux valgus underwent surgical correction using the MICA technique. However, 36 patients were lost to follow-up and 7 did not want to participate in the study. Thus, the final evaluation consisted of 58 patients (53 female; 5 male) and 69 feet (11 bilateral).
The mean age (± standard deviation) of the patients was 69.0 ± 9.8 years (range 39–89) years. The mean follow-up time was 27.0 months (range 24–39). Regarding laterality, in most cases the left foot was the one affected, totaling 36 feet (52.2%). Most deformities of the hallux valgus were classified as moderate, representing 56.5% of the sample.
Regarding the associated procedures, DMMO was performed on 35 feet (50.7%), correction of lesser toes in 21 (30.4%) and oblique osteotomy to the 5th metatarsal for bunionette treatment in 2 (2.8%). In 24 feet (34.7%), it was necessary, intraoperatively, to release percutaneously the lateral structures to correct residual valgus deformity.
Clinical outcomes
Clinical outcomes are shown in Table 1.
There was an improvement in function and pain with significant differences between the values collected before and after the surgical procedure (p < 0.001), with a mean increase in the AOFAS of 36.9 points and a reduction of 5.4 in the VAS. Regarding the ROM, there was a reduction in dorsal and plantar flexion of the metatarsophalangeal joint after the hallux valgus correction procedure, with statistical significance (p < 0.001).
Radiographic assessment
The radiographic outcomes are shown in Table 2.
The difference in radiographic measurements was also statistically significant, with a reduction in the HVA of 30.8° and IMA of 10.3° as an outcome after surgery. Recurrence of the deformity with HVA > 20° occurred in six cases, of which four had a severe deformity (> 40°) preoperatively.
All Akin osteotomies achieved bone union (Fig. 3).
In 14 feet (20.2%), there was malunion of the Akin osteotomy, with the distal fragment remaining in hyperextension. In none of them was the angulation greater than 10°, no patient evolved to radiographic arthrosis in the tarsometatarsal joint. There was no breakage of the screws in any case.
Personal satisfaction with the procedure
Regarding personal satisfaction with the end result of surgery, the personal satisfaction score published by Coughlin et al. was used [15]. The questionnaire was given in the last visit, and the responses were rated as follows: 85.5% excellent, 10.1% good, 2.9% fair and 1.5% poor. When the patient was asked if he could go back in time if he would do the procedure again, the majority said yes (85.5%).
Complications
The most common complication was discomfort in the site of the screws (11.6%). The sample had five cases (7.2%) that required an additional surgical procedure, with four of them only removing the screw and another in which it was necessary to remove the screws and perform an additional percutaneous exostectomy.
No patient had surgical wound dehiscence, superficial or deep infection. Furthermore, no patient developed pain in the topography of the tarsometatarsal joint.
Discussion
There are clear advantages of not performing Akin osteotomy fixation: It makes the procedure cheaper, faster and avoids implant-related complications such as migration or irritation of tendons or skin. This is the first case series of modified third-generation MICA with non-fixation of Akin.
The results obtained about pain improvement and functional assessment are like those found in the series in which Akin was fixed. Pain intensity in this series, assessed using the visual analog scale (VAS), dropped from 6.0 to 0.6 at the end of follow-up. The largest MICA case series that included 292 feet found a reduction in pain from 3.1 to 0.8 [20].
We used the AOFAS scale for functional assessment, and the result obtained was an improvement from 57.0 preoperatively to 93.9. Other studies that used the AOFAS scale to evaluate the results of the third-generation MICA technique obtained results between 83 and 92 at the end of follow-up [1, 3, 5].
The radiographic outcomes of this study were consistent with those reported in previous studies. Significant reductions were observed in both hallux valgus angle (HVA) and intermetatarsal angle (IMA), from 39.7 to 8.9 and 16.7 to 6.4, respectively. Previous case series using Akin fixation techniques reported mean HVA values ranging from 7.6 to 12.1 and mean IMA values ranging from 4.9 to 7.6 [1, 3, 5, 21].
We did not measure HIA, PDPAA and PPAA in the preoperative radiographs. Previous studies have shown that preoperative AP weight-bearing radiographs have low sensitivity evaluating the interphalangeal hallux valgus due to hallux pronation and some angles are underestimated [14, 22] This series has many patients with moderate to severe deformity including pronation.
The results obtained for these angles at the end of the follow-up were 13.3, 0.3 and − 6.0, respectively. Other studies that performed Akin osteotomy percutaneously obtained an HIA of 10.7 and 5.0 [11, 23]. As for the other angles, there is a wide variation in the literature regarding the results obtained, ranging from − 4.0 to 3.1 for PDPAA and 2.1 to 6.1 for PPAA [11, 24].
In this series, there was recurrence of the deformity, with HVA greater than 20°, in 6 (8.7%) patients, a number similar to that found in other studies [2, 4, 21]. These data show that Akin fixation probably has little impact on the final radiographic result.
All Akin osteotomies healed, but in 14 feet (20.2%), the distal fragment healed in hyperextension. None of these patients complained about the deformity, and no further intervention was required. The malunion rate in the literature varies between 0 and 24%, and some authors consider that it may be associated with disruption of the lateral cortex [10, 25,26,27].
Some studies have evaluated the frequency at which lateral cortical disruption can occur. Douthett et al. [28] identified 47 cases (35%) in a series where the Akin procedure was performed open. Testa et al. [10] delineated 86 cases out of 286 (30%), additionally executing procedures through open methods, contrasting with the present study where all procedures were conducted minimally invasively.
In Schilde’s comparative study, violation occurred in 51.6% of percutaneous osteotomies and only 13.9% of open procedures [23]. A study published by Kauffmann et al. [11] included 81 feet where percutaneous Akin osteotomy was performed without fixation. At the end of the follow-up, all osteotomies healed and there was correction of all radiographic parameters, but no assessment of sagittal plane malunion was performed.
The ROM assessment performed showed a loss of 20.1° of plantarflexion and 13.9° of dorsiflexion. Frigg et al. [29], in their comparative study between a technique similar to MICA and an open technique (Scarf), obtained an average of 10° and 5° of gain in dorsiflexion and plantar flexion, respectively. At the end of the follow-up, there were 8 cases of moderate stiffness and 1 patient with less than 30° of dorsiflexion out of 15 operated on using the minimally invasive technique.
Harrasser et al. [30] recently published a series of 55 feet and found moderate stiffness with loss of ROM greater than 10° in relation to the preoperative period in only 3 cases (5.4%) after 12 months of follow-up; there were no cases of severe stiffness.
Our series had worse results regarding ROM preservation compared to these two studies. One plausible explanation is that the average age of patients in our series (69 years) significantly exceeds that observed in the other two studies (48 and 50 years). This higher incidence of stiffness, however, did not negatively impact patient satisfaction, which was high with 95% of excellent or good results.
It is regarded as a specific strength of our study that it is the first study to examine a large case series of third-generation MICA osteotomy with non-fixed Akin. Our study, also, has some limitations: First, this is a case series with a relatively small sample compared to the largest series ever published; second, the lack of a control group; and finally, the absence of patient-reported outcomes measures (PROMs).
Conclusion
The use of MICA without Akin osteotomy fixation resulted in successful correction of hallux valgus with improvements in clinical and radiographic parameters.
Data availability
Not available.
References
Lee M, Walsh J, Smith MM, Ling J, Wines A, Lam P (2017) Hallux Valgus correction comparing percutaneous chevron/akin (PECA) and open scarf/akin osteotomies. Foot Ankle Int 38:838–846. https://doi.org/10.1177/1071100717704941
Tay AYW, Goh GS, Koo K, Yeo NEM (2022) Third-generation minimally invasive chevron-akin osteotomy for hallux valgus produces similar clinical and radiological outcomes as scarf-akin osteotomy at 2 years: a matched cohort study. Foot Ankle Int 43:321–330. https://doi.org/10.1177/10711007211049193
de Carvalho KAM, Baptista AD, de Cesar NC, Johnson AH, Dalmau-Pastor M (2022) minimally invasive chevron-akin for correction of moderate and severe hallux valgus deformities: clinical and radiologic outcomes with a minimum 2-year follow-up. Foot Ankle Int 43:1317–1330. https://doi.org/10.1177/10711007221114123
Lewis TL, Ray R, Robinson P, Dearden PMC, Goff TJ, Watt C, Lam P (2021) Percutaneous chevron and akin (PECA) osteotomies for severe hallux valgus deformity with mean 3-year follow-up. Foot Ankle Int 42:1231–1240. https://doi.org/10.1177/10711007211008498
Holme TJ, Sivaloganathan SS, Patel B, Kunasingam K (2020) Third-generation minimally invasive chevron akin osteotomy for hallux valgus. Foot Ankle Int 41:50–56. https://doi.org/10.1177/1071100719874360
Ferreira GF, Borges VQ, Moraes LVM, Stefani KC (2021) Percutaneous chevron/akin (PECA) versus open scarf/Akin (SA) osteotomy treatment for hallux valgus: a systematic review and meta-analysis. PLoS ONE 16:e0242496. https://doi.org/10.1371/journal.pone.0242496
Nunes GA, de Carvalho KAM, Ferreira GF, Filho MVP, Baptista AD, Zambelli R, Vega J (2023) Minimally invasive chevron akin (MICA) osteotomy for severe hallux valgus. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-023-04849-3
Redfern D, Vernois J (2016) Minimally invasive chevron akin (MICA) for correction of hallux valgus. Tech Foot Ankle Surg 15:3–11. https://doi.org/10.1097/btf.0000000000000102
Akin O (1925) The treatment of hallux valgus: a new operative procedure and its results. Med Sentinel 33:678–679
Testa EA, Porreca A, Nasarre AR, Cano DP, Goenaga FA, Ledermann G, Baduell A, Riquelme PR (2023) The Akin osteotomy without fixation in open hallux abducto-valgo correction surgery - A single center retrospective analysis of cases. Foot Ankle Surg. https://doi.org/10.1016/j.fas.2023.01.002
Kaufmann G, Handle M, Liebensteiner M, Braito M, Dammerer D (2018) Percutaneous minimally invasive Akin osteotomy in hallux valgus interphalangeus: a case series. Int Orthop 42:117–124. https://doi.org/10.1007/s00264-017-3638-4
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 4:e296. https://doi.org/10.1371/journal.pmed.0040296
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353. https://doi.org/10.1177/107110079401500701
Dixon AE, Lee LC, Charlton TP, Thordarson DB (2015) Increased incidence and severity of postoperative radiographic hallux valgus interphalangeus with surgical correction of hallux valgus. Foot Ankle Int 36:961–968. https://doi.org/10.1177/1071100715579905
Coughlin MJ (1991) Treatment of bunionette deformity with longitudinal diaphyseal osteotomy with distal soft tissue repair. Foot Ankle 11:195–203. https://doi.org/10.1177/107110079101100402
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Ferreira GF, Nunes GA, Mattos EDMC, Pedroso JP, Lewis TL, Lam P, Filho MVP (2022) Technique tip: medial prominence bone spur resection in the third-generation percutaneous chevron-akin osteotomy technique (PECA) for hallux valgus correction. Foot Ankle Surg 28:460–463. https://doi.org/10.1016/j.fas.2021.11.004
Team RC (2013) R: A language and environment for statistical computing. Foundation for Statistical Computing, Vienna, Austria.
Shapiro SS, Wilk MB (1965) Analysis of variance test for normality (complete samples). Biometrika 52:591–611
Lewis TL, Ray R, Miller G, Gordon DJ (2021) Third-generation minimally invasive chevron and akin osteotomies (MICA) in hallux valgus surgery: two-year follow-up of 292 cases. J Bone Joint Surg Am 103:1203–1211. https://doi.org/10.2106/JBJS.20.01178
Mikhail CM, Markowitz J, Di Lenarda L, Guzman J, Vulcano E (2022) Clinical and radiographic outcomes of percutaneous chevron-akin osteotomies for the correction of hallux valgus deformity. Foot Ankle Int 43:32–41. https://doi.org/10.1177/10711007211031218
Park JY, Jung HG, Kim TH, Kang MS (2011) Intraoperative incidence of hallux valgus interphalangeus following basilar first metatarsal osteotomy and distal soft tissue realignment. Foot Ankle Int 32:1058–1062. https://doi.org/10.3113/FAI.2011.1058
Schilde S, Delank KS, Arbab D, Gutteck N (2021) Minimally invasive vs open akin osteotomy. Foot Ankle Int 42:278–286. https://doi.org/10.1177/1071100720962411
Kilinc BE, Oc Y, Erturer RE (2018) Modified lindgren-turan osteotomy for hallux valgus deformity - a review of 60 cases. Acta Chir Orthop Traumatol Cech 85:325–330
Frey C, Jahss M, Kummer FJ (1991) The Akin procedure: an analysis of results. Foot Ankle 12:1–6. https://doi.org/10.1177/107110079101200101
Montiel V, Suarez A, Riera L, Villas C, Alfonso M (2020) Akin osteotomy: is the type of staple fixation relevant? Int Orthop 44:1435–1439. https://doi.org/10.1007/s00264-020-04563-4
Schlefman BS (1999) Akin osteotomy with horizontal interosseous wire-loop fixation. J Am Podiatr Med Assoc 89:194–198. https://doi.org/10.7547/87507315-89-4-194
Douthett SM, Plaskey NK, Fallat LM, Kish J (2018) Retrospective analysis of the akin osteotomy. J Foot Ankle Surg 57:38–43. https://doi.org/10.1053/j.jfas.2017.06.026
Frigg A, Zaugg S, Maquieira G, Pellegrino A (2019) Stiffness and range of motion after minimally invasive chevron-akin and open scarf-akin procedures. Foot Ankle Int 40:515–525. https://doi.org/10.1177/1071100718818577
Harrasser N, Hinterwimmer F, Baumbach SF, Pfahl K, Glowalla C, Walther M, Horterer H (2022) The distal metatarsal screw is not always necessary in third-generation MICA: a case-control study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04740-7
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Author information
Authors and Affiliations
Contributions
GFF and MVPF designed the study, submitted it to the ethics committee, performed the surgeries, collected the data, performed the statistical analysis and wrote the article. GMP and JPP also collected the data. MCMD, GANGS and TLL wrote and revised the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article. ICMJE forms for all authors are available online.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ferreira, G.F., Nunes, G.A., Pugliese, G.M. et al. Minimally invasive Chevron-Akin (MICA) osteotomies without Akin fixation in hallux valgus correction: a case series with 2-year follow-up. Eur J Orthop Surg Traumatol 34, 2339–2345 (2024). https://doi.org/10.1007/s00590-024-03924-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-024-03924-8