Abstract
Introduction
The minimally invasive Chevron Akin (MICA) osteotomy has been widely used to treat hallux valgus (HV). The purpose of this study was to present a case series of patients with severe HV undergoing surgical treatment using the MICA procedure and to evaluate the clinical and radiographic outcomes.
Materials and methods
Retrospective study including 60 consecutive feet (52 patients) undergoing MICA for severe HV. The data were collected pre- and post-operatively at the last follow-up. Patients were clinically evaluated by the visual analog pain scale (VAS) and AOFAS hallux MTP-IP score. Radiographic assessments included measurements of hallux valgus angle (HVA), intermetatarsal angle (IMA), metatarsal (MT) length, distal metatarsal articular angle (DMAA), and plantar translation of MT head. The complications were recorded during the follow-up.
Results
The mean age was 59.9 years, and the mean follow-up was 20.5 months. The average AOFAS increased from 41.2 to 90.9 points, and the VAS from 8.1 to 1.3 at the last follow-up. The average HVA decreased from 41.2º to 11.6º, the IMA from 17.1º to 6.9º, and the DMAA from 17.9º to 7.8º. The average shortening of the first metatarsal and the plantar translation of the MT head was 5.1 mm and 2.8 mm, respectively. The most observed complication was hardware discomfort, observed in 5 feet (8.3%). There were two cases of recurrence (3.3%).
Conclusion
MICA technique was demonstrated in this series of cases to be an effective procedure for severe HV, with a low rate of recurrence and an acceptable rate of complications.
Level of evidence
IV; case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hallux valgus (HV) is a common foot problem, and its treatment is widely discussed in the literature [1,2,3]. The etiology of HV is multifactorial, with anatomical, hereditary, and biomechanical factors involved. Unfortunate cases that do not improve with conservative measures can be treated surgically [4, 5]. HV is classified based on a radiographic assessment of weight-bearing radiographs. Severe hallux valgus is defined as a hallux valgus angle (HVA) greater than 40° and, or the intermetatarsal angle between the first and second rays (IMA) greater than 20° [6]. The treatment of severe deformities is a great challenge. Surgical option is not unique, and the variety of choices has been dictated by the multiplicity of causal factors and the surgeon's personal preference [7]. Traditionally, proximal metatarsal osteotomies have been used to correct severe HV deformities [8, 9]. However, they have been accompanied by significant complications such as recurrence, pseudarthrosis, overcorrection, and prolonged recovery [8, 9]. Another good option for severe cases is Lapidus arthrodesis [10]. However, this procedure is technically demanding and associated with a prolonged period of recovery and increased morbidity when compared to metatarsal osteotomies [11].
Several minimally invasive (MIS) techniques have recently emerged and gained popularity in treating HV deformity [7]. Redfern and Vernois developed the minimally invasive Chevron Akin (MICA) [12, 13]. MICA is a third-generation percutaneous procedure for symptomatic mild to severe HV deformity [14]. According to the literature, MICA has been reported to have had excellent results and low complication rates in treating mild to moderate HV deformity [15,16,17]. However, there is a lack of radiographic correction, clinical improvement, and complications following percutaneous third-generation to severe HV [18, 19]. There are only two case series of MICA, including just severe deformities [18, 19]. Additionally, one of these series evaluated the radiographic parameters correction only after a 6-weeks postoperative period [19].
The present study aims to evaluate the radiographic parameters, clinical improvement, and potential complications in a case series of severe HV. We hypothesized that the MICA technique could be able to correct severe deformities with good clinical outcomes and acceptable complications and recurrence rates for severe HV.
Methods
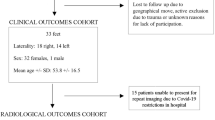
This multicenter study presents a retrospective evaluation of 60 consecutive feet (52 patients) diagnosed with severe HV that underwent MICA. Four different surgeons, with a minimum of 5 years of experience in MIS, from three different centers, did the surgery between January 2017 and December 2020. Inclusion criteria were patients with a diagnosis of severe HV (according to the radiographic angles) who did not improve with conservative treatment, which was carried out with the adaptation of shoes and symptomatic medication. Exclusion criteria were previous history of foot surgery, arthrosis of the metatarsophalangeal joint of the hallux, rheumatological and neurological disease, vascular problems, and patients that could not follow the postoperative protocol.
All patients were clinically and radiographically assessed pre- and postoperatively, with a mean follow-up of 20.5 months. Clinical preoperative assessment included the American Orthopedic Foot and Ankle Score (AOFAS) [20] and the visual analog pain scale (VAS) [21]. The VAS was used to assess pain in the metatarsophalangeal joint of the hallux. Pain in other places, such as central metatarsalgia, for example, was considered a complication. At the last follow-up appointment, patients answered the AOFAS and rated pain on the VAS once more. Complications were also documented.
Radiographic assessments were obtained in full weight-bearing, anteroposterior (AP), and lateral views. Utilizing the mechanical axis of the first and second metatarsals and the proximal phalanx of the hallux, the HVA, IMA, and distal metatarsal articular angle (DMAA) were measured [22, 23] (Fig. 1). The first metatarsal length (MTL) was measured in the axial plane as a distance between the center of the proximal and distal articular surface. The plantar translation of the first metatarsal was defined as the distance between the dorsal cortéx of the proximal and distal fragment of the osteotomy in the sagittal view.
Two fellowship-trained orthopedic foot and ankle surgeons not involved in the surgical procedure performed the radiographic analysis. The measurements were done preoperatively and postoperatively after 6 weeks, 6 months, and at the last follow-up. Radiographic recurrence was defined as a change in HVA > 2.6° between any two postoperative radiographs and an HVA > 15° according to the method of Kilmartin et al. [24].
All patients signed the consent form and accepted to be included in the study. Our institutional ethics committee approved this study (16213319.8.0000.5122).
Statistical data analysis
The statistical analysis was performed using the software R. Descriptive statistics were used for the nominal variables. Mean, standard deviation, maximum, and minimum were calculated for numerical variables. The Shapiro test was performed to determine whether the data were parametric or nonparametric. Nonparametric means were compared using the Wilcoxon signed rank paired test. The Student’s paired T test analyzed variables with parametric distribution to compare the means.
Surgical technique
The technique was performed as described by Redfern and Vernois [12, 13]. The patients underwent the surgical procedure under spinal anesthesia and antibiotic prophylaxis per hospital protocol. They were placed supine with their feet hanging from the operating table. The image intensifier was positioned with the detector beneath the operated foot.
An extracapsular portal was performed at the distal metaphyseal–diaphyseal transition at the medial side of the first metatarsal. Through this portal, a Shannon burr 2 × 20 mm was introduced at the base of the flare of the distal metaphysis of the first metatarsal (Fig. 2A). The osteotomy displacement plane was performed according to the cutter orientation in both transversal and coronal planes. A Chevron osteotomy of approximately 130º was performed, with a dorsal cut perpendicular to the first metatarsal axis.
A dorsomedial guidewire was introduced at the base of the first metatarsal until it breached the lateral cortex. After introducing the guidewire, the lateral displacement of the metatarsal head was performed using an elevator or a Kirschner wire inserted in the medullar canal (Fig. 2B). The guidewire was then progressed to fix the metatarsal head, and a 4.0 mm headless cannulated screw was inserted, passing through the medial and lateral cortices before fixing the metatarsal head. A second anti-rotational screw was inserted in the same plane, slightly distal to the first screw (Fig. 2C, D). Subsequently, the medial diaphyseal prominence was resected using a Shannon 2 × 12 mm through the proximal screw entry portal.
If there was an incongruity of the metatarsophalangeal joint of the hallux or if the lateral sesamoid remained uncovered, the release of lateral soft tissues (sesamoid-phalangeal ligament and lateral head of flexor hallucis brevis) was done by an extra lateral portal. The next step was to proceed to Akin’s osteotomy, performed through medial access to the base of the proximal phalanx. Using a 2 × 12 mm Shannon burr, the osteotomy was achieved in the proximal metaphyseal region cautiously to keep the lateral cortex intact (Fig. 2E). The washing and removal of bone debris were performed with abundant saline irrigation. The procedure was finished with the closure of the surgical incisions and applying a padded dressing and adhesive tape.
Postoperative protocol
Patients were allowed full weight-bearing according to tolerance when discharged from the clinic using a rigid sole orthopedic shoe worn for 6 weeks. Crutches were used if required. In the first 14 days after surgery, they were instructed to keep their foot elevated above the level of the ipsilateral hip to minimize postoperative swelling. After the 1st week, the surgical dressing was replaced by Steri-Strips applied to the portals. Thenceforth, the dressings were changed daily by the patients. Gentle exercises for the range of motion of hallux were introduced in the 2nd week and intensified during the follow-up according to the patient's evolution. After the 6th week, the patients were allowed to wear conventional shoes with a wide anterior chamber and a rigid sole.
Results
In this study, 60 feet (52 patients) with severe HV were evaluated pre- and post-operatively. The mean age of the patients was 59.9 (ranging from 32 to 82) years, and 45 patients were female. The mean follow-up was 20.5 months (ranging from 18 to 32). Additional minimally invasive procedures were performed on 20 (33%) feet, including nine osteotomies of the fifth metatarsal for bunionette, ten distal minimally invasive osteotomies of the second, third, and fourth metatarsals, and 14 proximal phalangeal osteotomies with a selective flexor longus tenotomy for lesser toe corrections.
Clinical outcomes and radiographic assessment
Clinical and radiographic variables assessed pre- and postoperatively showed statistically significant improvement, as demonstrated in Table 1.
Complications
There was a complication in 14 (23.3%) cases. The most common complication was the removal of screws in 5 feet (8.3%) due to discomfort from the hardware at the insertion point in the proximal metatarsal region. Two patients (3.3%) had medial dorsal cutaneous nerve neuropraxia that self-resolved, and another three (5%) had a superficial infection that resolved with oral antibiotics. Two cases (3.3%) of HV recurrence and two (3.3%) had a medial wall fracture of the first metatarsal 1 week after surgery treated conservatively. There was no delayed union, pseudarthrosis, or malunion. (Fig. 3).
Discussion
The most important contribution of this study was to demonstrate the clinical improvement and radiological correction in a case series of patients with severe HV who underwent surgical treatment with MICA. The results of this study collaborate to increase the scientific evidence on the safety and effectiveness of this technique for the treatment of severe HV.
Correcting severe deformities is challenging, since there is evidence of increased complication rates [25, 26]. Several open techniques are described in the literature, but there is still no unanimity [7]. Some studies emphasize that diaphyseal and proximal osteotomies are more appropriate to correct severe hallux valgus than distal osteotomies [6, 27]. Law et al. [28] analyzed 18 severe cases that achieved an open scarf osteotomy and a mean decrease in HVA and IMA of 32.1° and 10.4°, respectively. Wang et al. [29] treated 30 severe HV cases with open double metatarsal osteotomy, achieving a mean decrease in HVA and IMA of 29.5° and 9.3°, respectively. The present study demonstrated a similar improvement with a mean decrease in HVA and IMA of 29.6° and 10.2°, respectively. Although MICA is a distal metatarsal procedure, metatarsal osteotomy is extracapsular. It uses a specific fixation with screws that make it possible to perform large displacements of the metatarsal head and obtain excellent radiographic corrections to severe deformity.
Only two series cases included just severe HV that underwent the third-generation MIS technique. [18, 19]. The first one, described by Lewis et al. [18], reported the clinical and radiological outcomes of 53 severe HV in a long follow-up term. They achieved an average decrease in HVA and IMA of 32.5° and 12.4°, respectively. The second study [19] reported a 6-week postoperative radiographic result of 106 patients with severe HV, reaching an average decrease in HVA and IMA of 34.4° and 11.9°, respectively. The similarity of these radiographic results with our study reinforces the power of the third-generation MIS procedure in correcting severe HV deformities. Regarding the DMAA, a unique study analyzing this variable after MICA was described by Kepler et al. [30]. They showed an average decrease of 9.6°, while our study had a similar decrease of 10.1°. Although MICA does not remove a wedge to correct the tilt of the joint surface, it changes the anatomical axis of the first metatarsal preoperatively to the mechanical axis postoperatively, decreasing the DMAA [30].
The present study demonstrated an improvement in the function of the patients, with a mean increase of the AOFAS going from 41.2 to 90.9 points. Other studies involving the MICA technique for treating moderate to severe HV have shown similar clinical improvement [30, 31]. First, Kepler et al. [30] analyzed 70 feet and achieved an average increase in the AOFAS score from 43.9 to 90.1 points. Jowett and Bedi [31] improved AOFAS from 56 to 87 points in a study of 106 patients. It has been shown that there is a clinical improvement up to 2 years of follow-up after MICA [32]. Therefore, the positive clinical results of the present study can improve over time.
The complication rate of this study was 23.3% (14 patients). The most common complication was discomfort caused by the screws in 5 feet (8.3%) that improved after reoperation removing the screws. Despite this, a rigid fixation was essential to avoid major complications. There was no delayed union, pseudarthrosis, or malunion. A higher rate of these complications has been observed in the non-fixed MIS techniques [33, 34]. Two patients (3.3%) had a medial wall fracture of the first metatarsal one week after surgery, treated conservatively. They were maintained with an elastic bandage to keep the correction with non-weight bearing for 6 weeks. Two other patients (3.3%) had a recurrence of the deformity.
There is concern about the high recurrence rate with distal osteotomies for treating severe deformities [35]. In this series, two patients (3.3%) had a recurrence of HV. This rate compares well to the literature, with the reported recurrence rate for open surgery for severe hallux valgus ranging from 2.7 to 16% [36]. Lewis et al. [19], in a study with a similar follow-up to ours, obtained a resembling recurrence rate of 2.8% in 106 patients with severe HV treated by MICA. Despite being a distal technique, as suggested by Nunes et al., MICA locks the first metatarsal cuneiform joint in a maximum medial position, stabilizing the transverse plane and reducing the risk of recurrence [37]. Both recurrences of this study occurred due to an increase in HVA and developed a mild HV (Fig. 4).
There is criticism of minimally invasive surgery concerning the excessive metatarsal shortening caused by drills [38]. According to the burr orientation at the transverse plane, the surgeon can decide whether or not to shorten the metatarsal with MICA. For severe deformities, shortening is desirable and essential to achieving good correction, reducing soft tissue tension, and preventing recurrence [39]. To compensate for the shortening and to decrease the risk of a transfer metatarsalgia, the osteotomy can be done with an orientation of more than 10º from dorsal to plantar in the coronal plane, promoting a plantar translation of the metatarsal head. In this case series, the mean metatarsal shortening of 5.1 mm was accompanied by a mean plantar displacement of 2.8 mm (Fig. 5), and there were no cases of transfer metatarsalgia.
A Frontal view showing the plantar inclination of the burr used to achieve a plantar displacement of the metatarsal head. B Lateral postoperative radiograph demonstrating the plantar translation of the metatarsal head. Note the distance from the red lines that tangent the dorsal cortex of the proximal and distal fragments
Surgical treatment of severe HV cases is still challenging due to the heterogeneity of factors related to HV and the lack of the ideal procedure [1, 9]. The first metatarsal rotation directly correlates with HV recurrence [40, 41]. We believe that some degree of metatarsal rotation correction occurs automatically during the medial displacement of the head. After repositioning the metatarsal head, the force vector generated by the soft tissues fits into the correct axis and collaborates to correct the rotation. Recently Nunes and Baumfeld described an MIS third-generation rotational osteotomy [42]. However, it is only a technical report, and further studies will be required to evaluate the correction of the first metatarsal rotation.
This study has several limitations, such as the small number of patients, inhomogeneous cohort, additional surgeries in 30% of the cases, and the short follow-up period. A large number of patients and a long-term follow-up would increase the study’s validity, as correction of severe HV needs time to evaluate possible late complications and HV recurrence. In addition, a comparative study with open procedures will be required.
Conclusion
This study confirms our hypothesis that the MICA technique can correct severe deformities with good clinical outcomes and acceptable complications and recurrence rates. Prospective and comparative studies with a similar open comparison group would be fundamental to reinforce our results.
Availability of data and materials
The datasets generated during the current study are available from the corresponding author on reasonable request.
References
Smyth NA, Aiyer AA (2018) Introduction: Why are there so many different surgeries for hallux valgus? Foot Ankle Clin 23(2):171–182
Siddiqui NA, LaPorta G, Walsh AL et al (2019) Radiographic outcomes of a percutaneous, reproducible distal metatarsal osteotomy for mild and moderate bunions: a multicenter study. J Foot Ankle Surg 58(6):1215–1222
Nix S, Smith M, Vicenzino B (2010) Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res 3:21
Izzo A, Vallefuoco S, Basso MA et al (2022) Role of lateral soft tissue release in percutaneous hallux valgus surgery: a systematic review and meta-analysis of the literature. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04693-x
Souza Júnior E, Vieira M, Baumfeld T et al (2020) Patient’s perspective on the surgical treatment of hallux valgus. J Foot Ankle 14(1):36–40
Robinson AH, Limbers JP (2005) Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br 87(8):1038–1045
Bia A, Guerra-Pinto F, Pereira BS et al (2018) Percutaneous osteotomies in hallux valgus: a systematic review. J Foot Ankle Surg 57(1):123–130
Palmanovich E, Myerson MS (2014) Correction of moderate and severe hallux valgus deformity with a distal metatarsal osteotomy using an intramedullary plate. Foot Ankle Clin 19(2):191–201
Pinney SJ, Song KR, Chou LB (2006) Surgical treatment of severe hallux valgus: the state of practice among academic foot and ankle surgeons. Foot Ankle Int 27(12):1024–1029
Jagadale VS, Thomas RL (2020) A clinical radiological and functional evaluation of lapidus surgery for moderate to severe bunion deformity shows excellent stable correction and high long-term patient satisfaction. Foot Ankle Spec 13(6):488–493
Willegger M, Holinka J, Ristl R et al (2015) Correction power and complications of first tarsometatarsal joint arthrodesis for hallux valgus deformity. Int Orthop 39(3):467–476 (11)
Redfern D, Vernois J (2016) Minimally Invasive Chevron Akin (MICA) for correction of hallux valgus. Tech Foot Ankle Surg 15(1):3–11
Vernois J, Redfern DJ (2016) Percutaneous surgery for severe hallux valgus. Foot Ankle Clin 21(3):479–493
Redfern D (2020) Minimally Invasive Chevron Akin (MICA) for correction of hallux valgus. Tech Foot Ankle Surg 19(3):132–141
Mikhail CM, Markowitz J, Di Lenarda L et al (2022) Clinical and radiographic outcomes of percutaneous Chevron-Akin osteotomies for the correction of hallux valgus deformity. Foot Ankle Int 43(1):32–41
Nunes G, Magalhães J, Baumfeld T et al (2020) Minimally invasive Chevron-Akin osteotomy: clinical and radiographic results. Journal of the Foot & Ankle 14(3):264–268
Harrasser N, Hinterwimmer F, Baumbach SF et al (2022) The distal metatarsal screw is not always necessary in third-generation MICA: a case-control study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04740-7
Lewis TL, Ray R, Robinson P et al (2021) Percutaneous Chevron, and Akin (PECA) osteotomies for severe hallux valgus deformity with mean 3-year follow-up. Foot Ankle Int 42(10):1231–1240
Lewis TL, Ray R, Gordon DJ (2022) Minimally invasive surgery for severe hallux valgus in 106 feet. Foot Ankle Surg 28(4):503–509
Kitaoka HB, Alexander IJ, Adelaar RS et al (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15(7):349–353
Coughlin MJ (1991) Treatment of bunionette deformity with longitudinal diaphyseal osteotomy with distal soft tissue repair. Foot Ankle 11(4):195–203
Siddiqui NA, Fink JN, Sharma P et al (2023) Mechanical axis method to determine first intermetatarsal angle and tibial sesamoid position. J Foot Ankle Surg 62(1):55–60
Siddiqui NA, Mayer BE, Fink JN (2021) Short-term, retrospective radiographic evaluation comparing pre- and post-operative measurements in the chevron and minimally invasive distal metatarsal osteotomy for hallux valgus correction. J Foot Ankle Surg 60(6):1144–1148
Kilmartin TE, Barrington RL, Wallace WA (1992) The X-ray measurement of hallux valgus: an inter- and intra-observer error study. Foot 2(1):7–11
Filippi J, Briceno J (2020) Complications after metatarsal osteotomies for hallux valgus: malunion, nonunion, avascular necrosis, and metatarsophalangeal osteoarthritis. Foot Ankle Clin 25(1):169–182
Al-Nammari SS, Christofi T, Clark C (2015) Double first metatarsal and akin osteotomy for severe hallux valgus. Foot Ankle Int 36(10):1215–1222
Li C, Lu L, Zhang Y et al (2019) F-shaped osteotomy combined with basal opening wedge osteotomy for severe hallux valgus. Orthop Surg 11(4):604–612
Law GW, Tay KS, Lim JWS et al (2020) Effect of severity of deformity on clinical outcomes of scarf osteotomies. Foot Ankle Int 41(6):705–713
Wang X, Wen Q, Li Y et al (2019) Introduction the revolving scarf osteotomy for treating severe hallux valgus with an increased distal metatarsal articular angle: a retrospective cohort study. BMC Musculoskelet Disord 20(1):508
de Carvalho KAM, Baptista AD, de Cesar NC, Johnson H, Dalmau-Pastor M (2022) Minimally invasive chevron-akin for correction of moderate and severe hallux valgus deformities: clinical and radiologic outcomes with a minimum 2-year follow up. Foot Ankle Int 43(10):1317–1330
Jowett CRJ, Bedi HS (2017) Preliminary results and learning curve of the minimally invasive Chevron Akin operation for hallux valgus. J Foot Ankle Surg 56(3):445–452
Lewis TL, Ray R, Gordon DJ (2022) Time to maximum clinical improvement following minimally invasive Chevron and Akin osteotomies (MICA) in hallux valgus surgery. Foot Ankle Surg 28(7):928–934
Kadakia AR, Smerek JP, Myerson MS (2007) Radiographic results after percutaneous distal metatarsal osteotomy for correction of hallux valgus deformity. Foot Ankle Int 28(3):355–360
Li SY, Zhang JZ, Zhang YT (2016) Managing complications of percutaneous surgery of the first metatarsal. Foot Ankle Clin 21(3):495–526
Song JH, Kang C, Hwang DS et al (2019) Comparison of radiographic and clinical results after extended distal chevron osteotomy with distal soft tissue release with moderate versus severe hallux valgus. Foot Ankle Int 40(3):297–306
Raikin SM, Miller AG, Daniel J (2014) Recurrence of hallux valgus: a review. Foot Ankle Clin 19(2):259–274
Nunes GA, Ferreira GF, Baumfeld T et al (2022) Minimally invasive Chevron Akin: locking the metatarsal-cuneiform joint. Foot Ankle Spec. https://doi.org/10.1177/19386400221079155
Jung HG, Zaret DI, Parks BG et al (2005) Effect of first metatarsal shortening and dorsiflexion osteotomies on forefoot plantar pressure in a cadaver model. Foot Ankle Int 26(9):748–753
Li X, Guo M, Zhu Y et al (2018) The excessive length of first ray as a risk factor for hallux valgus recurrence. PLoS One 13(10):1–12
Okuda R, Kinoshita M, Yasuda T et al (2007) The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am 89(10):2163–2172
Zambelli R, Baumfeld D (2020) Intraoperative and postoperative evaluation of hallux valgus correction: What is important? Foot Ankle Clin 25(1):127–139
Nunes GA, Baumfeld T (2022) Third generation rotational percutaneous osteotomy to hallux valgus. Tech Foot Ankle Surg. https://doi.org/10.1097/BTF.0000000000000357
Funding
The authors received no financial support for this article's research, authorship, and/or publication. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by GAN, GFF, MVPF, ADB, KAMC, RZ, and JV. The first draft of the manuscript was written by GAN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Gustavo Araujo Nunes is Novastep Speaker. The authors declare no potential conflicts of interest with respect to the research, authorship, and publication of this article. ICMJE forms for all authors are available online.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Bioethics Committee of Medical Institution, CAAE (Ethics Evaluation Submission Certificate) number: 16213319.8.0000.5122.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Figs. 1, 2, and 3. The participant has consented to the submission of this case series to the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nunes, G.A., de Carvalho, K.A.M., Ferreira, G.F. et al. Minimally invasive Chevron Akin (MICA) osteotomy for severe hallux valgus. Arch Orthop Trauma Surg 143, 5507–5514 (2023). https://doi.org/10.1007/s00402-023-04849-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04849-3