Abstract
Introduction
The therapeutic management of calcaneal fractures is currently a major source of controversy in the literature. There is no consensus on the need to treat these injuries conservatively or surgically, nor on the criteria for deciding one option or the other. Although the gold standard has classically been the open approach and osteosynthesis, there are currently minimally invasive techniques that also report good results. Our objective is to present our results and experience with the MBA® Orthofix external fixator in a series of cases of calcaneal fractures.
Methods
We performed a retrospective observational study in our center, between the years 2019 and 2021, of Sanders types II–IV calcaneal fractures operated with MBA® Orthofix external fixator. We recorded a total of 38 patients, 42 fractures. We registered demographic information, intraoperative, postoperative, radiological and functional parameters, using the American Orthopedic Foot and Ankle Society (AOFAS), Manchester-Oxford Foot Questionnaire (MOXFQ), EQ-5D and VAS scales.
Results
A total of 26 men and 12 women were included, and the median age was 38 years. Mean follow-up was 24,4 months (6, 8–40, 1). The average time to surgery was 7 days and partial loading was started at 2.5 weeks after external fixation, which was removed at 9.2 weeks. The average Böhler angle correction was 7, 4°, Gissane − 12,2°, length 2 mm and calcaneal width was reduced by 5 mm. We recorded two superficial infections, one peroneal entrapment and three subtalar arthrodesis due to post-traumatic osteoarthritis. The AOFAS obtained was 79.1 + / − 15.7 points, MOXFQ 20.1 + / − 16.1 points, EQ-5D 0.84 + / − 0.2 and VAS 3.3 + / − 1.9.
Conclusion
The external fixator is an excellent surgical alternative for complex articular fractures of the calcaneus, obtaining clinical and radiological results comparable to other osteosynthesis techniques and significantly reducing soft tissue complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcaneal fractures account for a low percentage of all fractures in the body, representing approximately 2% of them. Nevertheless, it is the most frequently fractured tarsal bone and up to 75% of these fractures are intra-articular [1,2,3,4,5,6,7,8,9,10,11,12,13,14].
These injuries usually occur due to high energy trauma [15]. The wide morbidity of this injury and the large number of long-term sequelae it may involve is well known, in some cases described to be similar to myocardial infarction or chronic kidney disease [2, 7, 15,16,17]. Many patients who suffer these injuries are not able to return to their previous activity. They may as well report complications such as chronic pain and difficulty in walking, among others, and may even require surgery for their sequelae [18].
However, up to date, treatment for calcaneal fractures remains controversial despite its continuous analysis for more than two decades [2, 4,5,6, 8,9,10, 12, 13, 20, 21].
There are meta-analyses [5, 12], which found no significant functional differences between conservative and surgical treatment. However, other studies recommend surgical treatment in order to obtain better results and earlier return to work, as well as a lower rate of post-traumatic osteoarthritis [1, 4, 6, 7, 18]. The initial purpose of the surgery was to reestablish the articular surface of the subtalar joint [22]. Some studies, however, already consider that the objective should be to reestablish the height and width of the calcaneus, restoring its three-dimensional morphology, and to perform premature mobilization and loading [1, 16, 22].
There is also no consensus as to which of the different surgical treatment options is most effective. There is a wide range of possibilities, which goes from open reduction with an extended lateral approach, to mini-open and minimally invasive techniques, such as the tarsal sinus approach, percutaneous techniques and even external fixation [17, 23]. None of them is free of complications, such as material intolerance, wound dehiscence and infections, etc., which in some series amounts to 25% [1, 10, 16,17,18, 24]. Open reduction and internal fixation are still considered to be the gold standard [1, 4, 6, 12, 15, 16, 23, 24], although recently there has been an increase in minimally invasive techniques [1, 7, 10, 15,16,17,18, 21, 23].
Our objective with this review is to analyze and present our experience with the synthesis of displaced intra-articular calcaneal fractures using the Orthofix external fixation device (MBA®) and to carry out a brief review of the literature on this injury and its treatment options today. We seek to expose a surgical therapeutic alternative that could obtain as good results as open surgeries, minimizing its complications, and serve as a basis for further studies.
Materials and methods
We conducted a retrospective observational and descriptive study at our center in Madrid, between the years 2019 and 2021. We obtained a total of 38 patients, with 42 calcaneal fractures, classified according to the Sanders classification, and surgically intervened using the Orthofix MBA® external fixation device. All surgeries were performed by members of the Complex Trauma Unit of our hospital.
The following data were analyzed for these patients:
-
1.
Demographic data:
-
a.
Age
-
b.
Sex
-
c.
Laterality
-
d.
Fracture classification according to Sanders
-
a.
-
2.
Parameters related to the surgery performed:
-
a.
Average time to surgery
-
b.
Closed reduction or association with mini-open
-
c.
Filling or not with graft
-
a.
-
3.
Postoperative protocol:
-
a.
Time to weight bearing
-
b.
Time until external fixator removal
-
a.
-
4.
Radiographic measurements:
-
a.
Böhler and Gissane angles preoperatively and at the end of follow-up.
-
a.
-
5.
Average calcaneal length and width correction.
-
6.
Complications at follow-up.
-
7.
Functional results:
-
a.
Return to work
-
b.
Return to sports
-
c.
Functional scales:
-
i.
American Orthopedic Foot and Ankle Society (AOFAS): Validated scale that takes into account pain, function and limb alignment, with 100 being the best possible outcome and 0 the worst possible outcome.
-
ii.
Manchester-Oxford Foot Questionnaire (MOXFQ): Validated questionnaire to assess the outcome of foot and ankle surgeries by means of 16 items, divided into three domains, which analyze problems in walking or standing, pain and social interaction. 0 is the best possible outcome, while 100 is the worst possible outcome.
-
iii.
¡EQ-5D: This is not a foot and ankle specific scale, but analyzes self-perceived health status in 5 dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). The average self-perceived value in Spain, according to a national health survey in the years 2011/12 was 0.914 (SD 0.15).
-
i.
-
d.
Pain scales: Visual Analogical Scale (VAS).
-
e.
Patient’s personal satisfaction with the surgery
-
a.
Details of the implant
The Orthofix Calcaneal Fixator (MBA®) is a device designed to restore calcaneal height and width and to reduce the articular surface in a minimally invasive manner.
It comprises two arms, connected by a central clamp. The fixed rail is in an anteroposterior plane, parallel to the longitudinal axis of the foot, with two pin holes at the anterior end and two at the posterior end. It allows to restore the length of the calcaneus (it can slide up to 35 mm). It also has an articulated arm (more than 100º of mobility), to find the best position according to the posterior facet with another rail, with two pin holes for the subtalar surface. This arm allows us to recover the lost height (it allows distraction up to 15 mm). All pinholes allow 35º of angulation. The pins are self-drilling and self-tapping, with a 4 mm diameter. They come in two lengths, 70 and 90 mm.
Reduction can be supplemented with percutaneous Kw and even minimally invasive approaches, if necessary.
This device is especially useful when there is poor soft tissue condition. The design is universal for both left and right foot. It comes in complete and sterile kits.
Surgical technique
All patients were operated under intradural anesthesia, by the same team of the Trauma Unit of our center.
We perform this procedure in lateral decubitus, with the patient lying on the healthy side, exposing the lateral side of the calcaneus. The C-arm fluoroscopy device enters from on-side the patient, and the surgeon is positioned at the feet.
At first, with a lateral fluoroscopy, we assess the correct position of the articulated arm under the subtalar surface. When appropriate, it is fixed with a first pin. We repeat the process with the most posterior pin, for the posterior apophysis of the calcaneus. The most anterior pin can be located on either the anterior tuberosity of the calcaneus or on the cuboid. The correct position is confirmed with an axial projection. If correct, the second pin is placed in each of these positions (subtalar, anterior and posterior).
After locking the pins to the fixator, height (hinged arm) and length (fixed arm) are restored using a hex wrench, on the rials that provide distraction. Most of the time, this indirect reduction is usually sufficient to restore the three-dimensional configuration of the calcaneus. The reduction can be assisted by a percutaneous Kw, using it as a joystick, if necessary.
If the reduction is not satisfactory, the fixator is removed, keeping the pins in place, and a minimal sinus tarsi approach is performed to lift the articular surface with a periosteal elevator. In cases where this maneuver left a large residual defect, it was filled with bone graft, available in the tissue bank of our center. Subsequently, the external fixator is repositioned and fixed.
Postoperative treatment
Three doses of antibiotics were administered, according to our center protocol. Patients were admitted for 24 h in most cases, prolonged up to 48 h if there was poor analgesic control.
Antithrombotic prophylaxis with low-molecular-weight heparin was maintained during the time the patients remained without weight-bearing. Patients were authorized to perform crutch-assisted partial weight bearing from the second-third week after surgery.
The external fixator was removed after the ninth week, as an ambulatory procedure.
Results
During the aforementioned study period, 38 patients were identified in our center, a total of 42 fractures, who underwent surgery using the Orthofix MBA® external fixator. Of these, 26 were men versus 12 women, and the median age was 38 years (30.8–52). Mean follow-up was 24,4 months (6,8–40,1).
According to the Sanders classification, based on computed tomography, 12 cases (29%) were Sanders type II, 18 cases (43%) were Sanders type III and 12 cases (29%) were Sanders type IV.
The average time to surgical intervention was 7 days (2–12). While all surgeries consisted of external fixation, on the lateral side of the calcaneus, 29 cases (69%) were reduced indirectly while 13 cases (31%) required a mini-open to the tarsal sinus and reduction assisted with a periostotome. Four of the latter cases also required bone grafting.
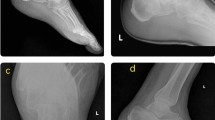
Postoperative follow-up was performed by the same surgeons of the Complex Trauma Unit. The average time to initiate partial weight bearing was 2.5 weeks. Partial weight bearing consisted of bilateral crutch assistance. The average time to removal of the external fixator was 9.2 weeks. Three radiographs from a patient who sustained this injury are provided in Fig. 1.
Radiographic evolution of one the patients included in this paper. It was a 42-year-old male, who suffered the fracture after a fall while recreational climbing. No other injuries were associated. Soft tissues were compromised around the fracture a Initial lateral X-ray on arrival at the emergency department. Calcaneus fracture can be observed b Lateral X-ray during follow-up (7th week), with external fixation device. c Lateral X-ray during follow-up, on loading, after removal of the fixator
Radiographically, the average preoperative Böhler angle was 8.4° (− 3.2°–14.7°) compared to 15.8° (10.5–20°) at the end of follow-up, an average improvement of 7,4° (0.6°–27.7°). As for the Gissane angle, the average preoperative value was 127º (108–131.4º), with a value at the end of follow-up of 114.8º (107º–123.8º), which means, an average correction of 12, 2º (5,3º–14.3º). At the end of follow-up, the calcaneal length gained with treatment was 2 mm (1–4.3 mm) and the width was reduced 5 mm (2–9 mm). A graphic summary of the Böhler and Gissane angle corrections can be seen in Figs. 2 and 3.
At the end of follow-up, there were two cases of superficial pin infection (representing 4.76%), which required antibiotic treatment without added gestures, until external fixator removal; we registered one peroneal entrapment, which improved after removal of the external fixator, without further procedures; and three cases of subtalar osteoarthritis requiring arthrodesis (7.9%). All of them had suffered initially a Sanders IV type calcaneal fracture. These patients showed the worst results in in the different functional scales.
At the end of follow-up, 33 patients (87%) were able to resume their pre-injury work activity. Of the total number of patients, 21 were involved in sports on a regular basis before the fracture and of these, 15 (71% of the total number of sportsmen) were able to totally or partially resume this activity.
If we expose the results obtained in the different functional scales, the average AOFAS score was 79.1 + / − 15.7 points; in the MOXFQ, an average value of 20.1 + / − 16.1 points was obtained; our patients presented an EQ-ED index of 0.84 + / − 0.2 points (average value of the Spanish population, according to the national survey in Spain 2011/12 of 0.914 with an E.D. of 0.15); the average VAS at the end of follow-up that we obtained was 3.3 + / − 1.9; finally, 87% of the patients declared themselves satisfied (18 cases) or very satisfied (15 cases) with the surgery. A summary of the functional results is shown in Fig. 4.
Discussion and review of the literature
The calcaneus is the most voluminous tarsal bone and the most frequently fractured, accounting for 2% of the total number of fractures in the body. Of these fractures, 75% involve the subtalar joint [1,2,3,4,5,6,7,8,9,10,11,12,13,14] and up to 15% result in open fractures and 5–10% bilateral fractures [15]. It also results in an injury that may involve significant long-term morbidity, as well as great economic impact [15, 16]. Factors such as advanced age, male gender, occupation, work compensation, etc., have been shown to play a role in the long-term outcomes of this injury, as demonstrated by the 2014 work of Agren et al. [4]. It is estimated that approximately 20% of individuals will not be able to return to their job at 1 year of this injury [16]. In our work, 87% of the patients could return to their pre-injury work activity. Of those who previously practiced any sports, 71% totally or partially resumed this activity.
Despite its frequency and the economic and social impact it entails, there is still much controversy about the need to treat these injuries conservatively or surgically and what criteria the orthopedic surgeon should use to choose one treatment option or the other. There is a wide variety of papers, literature reviews and meta-analyses that obtain very different results. In 2010 and 2013 Sutherland et al. [12, 13] conducted a Cochrane review analyzing the differences in outcomes of calcaneal fractures managed with and without surgery. For their 2013 work they included a total of 602 participants and concluded that there was no consensus or criteria for choosing the most appropriate treatment option. However, from two small of the included studies there was a trend toward earlier return to work in operated cases. In 2012, Jian et al. [11] performed another meta-analysis that included a total of 891 patients with this fracture. The operated patients had a significantly higher rate of complications, up to 22.8%. Nevertheless, they conclude that this is the price to pay for a better three-dimensional reconstruction of the calcaneus, which in their work resulted in better functional and radiological results. They recommend surgical management for displaced intra-articular calcaneal fractures. They found no significant differences in terms of residual pain. Another meta-analysis, from 2013, by Agren et al. [9] found no functional differences in surgical vs. conservative treatment at 1 year after injury. Nevertheless, they did find differences in longer follow-up periods, up to 8 and 12 years, in favor of surgery, since surgical treatment reduced the risk of post-traumatic subtalar osteoarthritis by up to 41%, among other differences. The review by Sharr et al. [18] deduces that there is a tendency to better functional results the more anatomical and stable the reduction of the lesion, something that other authors ratify in later works, such as Meena et al. [6] or Gotha et al. [7], meta-analysis and review, respectively, where the best functional, occupational and radiographic results were in the surgical treatment group, at the expense of a greater risk of complications. Wei et al. [5] carried out a meta-analysis in 2017 where they concluded that although surgical treatment presented a higher rate of complications with respect to conservative treatment, it also implied better anatomical restoration and, probably derived from this, also a better functional level, similar reincorporation to the pre-injury level, less discomfort with shoes and, in general, better physical activity. However, they emphasize that their result contrasts with other similar ones that do not obtain these differences, such as the 2016 meta-analysis by Luo et al. [8], whose conclusion was that with the published studies there is insufficient evidence to ensure that surgical treatment is superior to conservative treatment in the management of intra-articular calcaneal fractures. Only a lower rate of subtalar joint arthrodesis was found in those patients managed surgically, although high quality evidence is insufficient.
One of the reasons for arguing in favor of surgical treatment is the lower rate of subtalar arthrodesis due to premature osteoarthritis. Liu et al. [19] conducted a study in 2010, based on randomized clinical trials, recruiting a total of 966 patients, where they concluded that patients treated conservatively had a 4.4 higher risk of requiring subtalar arthrodesis. Radnay et al. [14] compared patients who required subtalar arthrodesis and retrospectively evaluated whether they received conservative versus surgical treatment. Those who underwent initial surgery had fewer wound complications, better functional outcomes and improved calcaneal length and width, which gave a chance for better long-term outcomes. According to Gotha et al. [7], the risk of needing a subtalar arthrodesis is 23% in Sanders type III fractures, but rises to 73% in type IV fractures, a factor that should perhaps be taken into account when choosing the type of treatment. In our study, all the patients that eventually required a subtalar arthrodesis had suffered a Sander type IV fracture. These patients showed the worst results in the different functional scales.
Among those who advocate surgical treatment, open reduction, through a lateral approach, and osteosynthesis have classically been chosen, with no differences between whether the plates used are locking plates or not [3]. Although there is consensus that it is the best option for adequate visualization of the fracture and the articular surface, as well as to reestablish the correct anatomy [7, 15], it is not free of complications, which in some series range between 20 and 37%, especially due to problems with the wound, dehiscence and infection [7, 10, 15, 21]. However, open reduction and internal fixation remains gold standard treatment option for these injuries [1, 4, 6, 12, 15, 16, 23, 24].
Minimally invasive techniques and approaches probably arise from the desire to obtain the best possible radiographic and functional results, with the need to minimize the potential complications of an open and extensive approach. In this regard, authors such as Hsu et al. [21] in 2015 already predicted intervention of the calcaneus with minimal approaches, such as the tarsal sinus approach, with percutaneous fixations and arthroscopic assistance to obtain the same results with fewer complications of the classic approach, similar to what Gotha et al. [7] obtained in 2016. Van Hoeve et al. [16] obtained very good clinical and radiographic results with osteosynthesis through minimal approaches and percutaneous reduction. On the other hand, in their analysis of the literature, they report a high rate of infection with the external fixator (they do not specify), something that contrasts with our work, where we only obtained two cases of superficial infection. Allegra et al. [15] carried out a study in 2020, updating concepts on intra-articular calcaneal fractures. They recommend surgical treatment in displaced intra-articular fractures and confirm the advantages of approaches to the tarsal sinus. They review the literature on percutaneous fixation and analyze several studies in which excellent values are obtained on the AOFAS scales with this technique, up to 92.6/100, with a 2.9% infection rate. The disadvantages of percutaneous fixation, even if complemented with a minimally invasive approach, include the possibility of residual displacement of the subtalar joint and the inability to manage the posterior articular facet when the fracture has more than 7–10 days.
External fixation as a definitive treatment for calcaneal fractures has been proposed as an alternative for years. In 2008, Magnan et al. [10] treated 54 calcaneal fractures with the Orthofix external fixator (MBA®) and analyzed their results. They obtained 26 excellent and 23 good results on the Maryland Foot Score scale. Although we have not used this functional scale, the promising results are similar to those obtained in our work (AOFAS 79.1/100; MOXFQ 20.1; EQ-5D 0.84; VAS: 3.3). In addition, they also evaluated the postoperative radiographic result by CT, where they obtained, according to the SAVE scale, an excellent reduction in 24 of 54 cases and good in 25 of 54 cases. In our series we did not perform postoperative CT in any patient; instead, our results were obtained from plain radiographs. We consider that there is little clinical-radiological correlation, with good clinical and functional results, despite radiographic measurements that could be improved. Regarding complications, they obtained a 5.6% infection rate, which only required antibiotic management without associated gestures, and which is higher than the rate of 4.76% obtained in our review. As a difference with respect to our work, which we consider important to mention, the protocol’s discharge time of their patients was 8 weeks, compared to 2,5 weeks in our review. However, our sample was relatively small and we did not use a control group to compare to, nor did we perform a statistical analysis. Kisel et al. [24] carried out a similar study, analyzing the early clinical and radiographic results through the use of external fixation, also using the Maryland scale for evaluation, with an average value of 85.8. They also analyzed the pre- and post-operative changes in length and width of the calcaneus and in the Böhler and Gissane angles. The length increased, on average, 5.2 mm, and the width decreased, on average 4.4 mm (in our work 2 and 5 mm, respectively). The Böhler angle was corrected by 4.9° (lower than our review) and the Gissane angle by 16.2° (12, 2° in our analysis). Corina et al. [17] analyzed the results of treatment with external fixator, according to subtypes of calcaneal fractures, and concluded that, although the radiographic results may not be ideal, the final functional result was excellent with this therapeutic alternative, analyzed, again, according to the Maryland scale (92.8% of good and excellent functional results). Again, we should mention, as a difference with respect to our work, that the average unloading time was 8 weeks, compared to 2.5 weeks for our patients; and that the external fixator was maintained until 12 weeks, compared to 9.2 weeks in our analysis. Premature loading, while it could have negatively influenced radiologic results, does not appear to have had a negative impact on functional outcomes and could make the immediate postoperative period more bearable. They obtained 8% of infections, compared to 4.76% in our work, and reconverted one case to arthrodesis (3 cases in our series). In Sanders type II fractures, Pan et al. [23] analyzed the biomechanical stability and functional outcome of treatment with external fixation versus open reduction and osteosynthesis, concluding that the external fixator is biomechanically stable, even superior, to osteosynthesis, and that it reduces surgery and hospitalization time, blood loss and the rate of wound complications. In this regard, other studies have been carried out comparing both surgical options, such as the 2020 study by Ortu et al. [1], which concluded that there are no differences in functional scales between performing osteosynthesis versus external fixation, with the advantages of the shorter surgical time of the fixator, lower complication rate and lower cost. The time to surgery was 4 times shorter in the external fixation group, since there is less concern for soft tissue. The AOFAS result of the osteosynthesis group was 73.31/100 versus 75.40/100 in the fixation group, values that agree with those obtained in our work (average AOFAS value obtained 79.1/100). Recently, in the year 2021, Wang et al. [22] emphasize that external fixation with minimally invasive reduction is equally effective as the tarsal sinus approach for Sanders II and III calcaneal fractures, with the advantage of minimizing complications derived from large approaches, and without the need to worry about patient-dependent circumstances, such as peripheral vasculopathies, poorly controlled diabetes or excessive tobacco abuse.
Conclusions
Despite the extensive literature on the subject, intra-articular calcaneal fractures continue to pose a therapeutic challenge for orthopedic surgeons, without being able to establish clear decision algorithms on which management option is the most appropriate.
Although open reduction and internal fixation remains the gold standard, the external fixator is an excellent surgical alternative for complex articular calcaneal fractures when there is concern about the soft tissues, obtaining clinical and radiological results comparable to other osteosynthesis techniques and significantly reducing soft tissue complications.
In our review we have allowed early partial loading of our patients, unlike many other works and treatments, without a negative translation in the functional results.
Further studies are required, with bigger samples, which compare external fixation with control groups of open osteosynthesis.
Limitations
The present study has some limitations.
First of all, this is a retrospective and descriptive study, with the limitations this implies. It would be adviseable to carry out prospective, randomized studies, with control groups, which analyze this injury and its treatments.
Secondly, the sample analyzed is relatively small, not sufficient to change the management of this injuries, so it would be convenient to carry out future work with larger study groups.
Finally, the radiographic measurements were carried out by a single evaluator, which may lead to measurement errors.
References
Ortu S, Brusoni M, Pisanu F, Caggiari G, Ciurlia E, Bienati F et al (2020) Functional and radiological outcomes in displaced heel fractures: open reduction and internal fixation versus external fixation. Orthop Rev (Pavia) 12(2):83–86
Ojeda-Jiménez J, Rendón-Díaz D, Martín-Vélez P, González-Martín D, Boluda-Mengod J, Méndez-Ojeda M et al (2020) Surgically treated calcaneal joint fractures: What does postoperative computed tomography give us? Rev Esp Cir Ortop Traumatol 64(6):393–400
Correoso Castellanos S, García Galvez A, Lajara Marco F, Blay DE (2019) Intra-articular calcaneal fractures. Do locking plates keep the reduction better than conventional plates? Rev Esp Cir Ortop Traumatol. 63(6):383–388
Ågren H, Mukka S, Tullberg T, Wretenberg P, Sayed-Noor AS (2014) Factors affecting long-term treatment results of displaced intraarticular calcaneal fractures: a post hoc analysis of a prospective, randomized Controlled Multicenter Trial. J Orthop Trauma 28:564–568
Wei N, Yuwen P, Liu W, Zhu Y, Chang W, Feng C et al (2017) Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a meta-analysis of current evidence base. Medicine 96:e9027
Meena S, Kumar Gangary S, Sharma P (2016) Review article: operative versus non-operative treatment for displaced intra-articular calcaneal fracture: a meta-analysis of randomised controlled trials. J Orthop Surg 24(3):411–416
Heather EG, Zide JR (2017) Current controversies in management of calcaneus fractures. Orthop Clin N Am 48:91–103
Luo X, Li Q, He S, He S (2016) Operative versus nonoperative treatment for displaced intra-articular calcaneal fractures: a meta-analysis of randomized controlled trials. J Foot Ankle Surg 55:821–828
Ågren PH, Wretenberg P, Sayed-Noor AS (2013) Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg 95(15):1351–1357
Magnan B, Bortolazzi R, Marangon A, Marino M, Dall’oca C, Bartolozzi P et al (2006) External fixation for displaced intra-articular fractures of the calcaneum. J Bone Joint Surg 88(B):1474–1479
Jiang N, Lin QR, Diao XC, Wu L, Yu B (2012) Surgical versus nonsurgical treatment of displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. Int Orthop 36:1615–1622
Bruce J, Sutherland A (2013) Surgical versus conservative interventions for displaced intra-articular calcaneal fractures (Review). Cochrane Database Syst Rev (1):CD008628. https://doi.org/10.1002/14651858.CD008628.pub2
Baliga SM, Sutherland A, Bruce J (2010) Surgical versus conservative interventions for displaced intra-articular calcaneal fractures (Protocol). Cochrane Database Syst Rev (8):CD008628. https://doi.org/10.1002/14651858.CD008628
Radnay CS, Clare MP, Sanders RW (2009) Subtalar fusion after displaced intra-articular calcaneal fractures: Does initial operative treatment matter? J Bone Joint Surg 7(3):541–546
Allegra PR, Rivera S, Desai SS, Aiyer A, Kaplan J, Gross CE (2020) Intra-articular calcaneus fractures: current concepts review. Foot Ankle Orthop 5:2473011420927334
van Hoeve S, Poeze M (2016) Outcome of minimally invasive open and percutaneous techniques for repair of calcaneal fractures: a systematic review. J Foot Ankle Surg 55(6):1256–1263
Corina G, Mori C, Vicenti G, Galante VN, Conserva V, Speciale D et al (2014) Heel displaced intra-articular fractures treated with mini-calcaneal external fixator. Injury 45(S6):S64-71
Sharr PJ, Mangupli MM, Winson IG, Buckley RE (2016) Current management options for displaced intra-articular calcaneal fractures: non-operative, ORIF, minimally invasive reduction and fixation or primary ORIF and subtalar arthrodesis. A contemporary review. Foot Ankle Surg 22:1–8
Liu Y, Li Z, Li H, Zhang Y, Wang P (2015) Protective effect of surgery against early subtalar arthrodesis in displaced intra-articular calcaneal fractures. Medicine 94:e1984
Roukis TS, Wünschel M, Lutz HP, Kirschner P, Zgonis T (2008) Treatment of displaced intra-articular calcaneal fractures with triangular tube-to-bar external fixation: long-term clinical follow-up and radiographic analysis. Clin Podiatr Med Surg 25:285–299
Hsu AR, Anderson RB, Cohen BE (2015) Advances in surgical management of intra-articular calcaneus fractures. J Am Acad Orthop Surg 23:399–407
Wang J, Qin S, Wang T, Liu J, Wang Z (2021) Comparison of the curative effect of percutaneous reduction with plastic calcaneal forceps combined with medial external fixation in the treatment of intra-articular calcaneal fractures. Orthop Surg 13(8):2344–2354
Pan M, Chal L, Xue F, Ding L, Tang G, Lv B (2017) Comparisons of external fixator combined with limited internal fixation and open reduction and internal fixation for Sanders type 2 calcaneal fractures. Finite element analysis and clinical outcome. Bone Joint Res. 6(7):433–438
Kissel CG, Husain ZS, Cottom JM, Scott RT, Vest J (2011) Early clinical and radiographic outcomes after treatment of displaced intra-articular calcaneal fractures using delta-frame external fixator construct. J Foot Ankle Surg 50(2):135–140
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this paperwork declare that there is no conflict of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Checa-Betegón, P., Valle-Cruz, J., Llanos-Sanz, S. et al. External fixation in intra-articular fractures of the calcaneus: Is it a valid option as definitive treatment?. Eur J Orthop Surg Traumatol 34, 201–208 (2024). https://doi.org/10.1007/s00590-023-03621-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-023-03621-y