Abstract
Purpose
Controversy still surrounds the optimal treatment for patients with displaced intra-articular calcaneal fractures (DIACF). An up-to-date meta-analysis was performed to evaluate clinical effectiveness of surgical treatment for DIACF compared with nonsurgical treatment.
Methods
We systematically searched four electronic databases (Medline, BIOSIS, Cochrane library and Google Scholar) to identify randomised controlled trials (RCTs) and clinical controlled trials (CCTs) in which surgical treatment was compared with nonsurgical treatment of DIACF from 1980 to 2011. Trial quality was assessed using the modified Jadad scale and effective data were pooled for meta-analysis.
Results
Ten studies (six RCTs and four CCTs) with a total of 891 participants were screened. Results showed that surgical treatment was superior to nonsurgical treatment in better recovery of the Böhler angle (P < 0.0001), more stable calcaneal height (P = 0.0009) and width (P < 0.00001). Moreover, fewer surgically treated patients needed increased shoe size (P = 0.0004) and more were able to resume pre-injury work (P = 0.004) than the nonsurgical patients. No significant difference was identified between the two methods regarding the incidence of residual pain (P = 0.49). However, operative management was associated with a higher risk of complications (P = 0.008).
Conclusions
Although surgical repair may increase the complication probability, it is the price that has to be paid for better reconstruction of the calcaneus and better functional results. Taken as a whole, surgery is probably the optimal choice in DIACF treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Calcaneal fracture, the most frequent injury of tarsal bones, accounts for about 1–2 % of all fractures in the human body [1]. According to a recent study [2], 75 % of the calcaneal fractures affect the foot function. Of all the calcaneal fractures, approximately 75 % are intra-articular [3], involving the subtalar joint. The intra-articular fracture is mostly caused by a fall from a height [4, 5, 21] with the heel directly hitting the ground. Vertical violence delivered to the foot often leads to the displaced intra-articular calcaneal fractures (DIACF).
Although conventional management of DIACF can be surgical or nonsurgical, controversy remains as to the optimal treatment of the injury, because both surgical and nonsurgical treatments have pros and cons. Outcomes from previous randomised controlled trials (RCTs) have varied. Some indicated [5–7] that surgical treatments may be superior to nonsurgical treatment, while others [8, 9] found no significant differences between the two methods. However, their conclusions were based on single studies and thus lack sufficient evidence to identify the optimal choice in DIACF treatment.
The aim of our meta-analysis was to determine the advantages and disadvantages of surgical versus nonsurgical DIACF treatments reported in all the related RCTs and clinical controlled trials (CCTs) available. We believe such a meta-analysis will yield stronger evidence to answer the question concerning clinical treatment of DIACF.
Methods
Study design and search strategy
All published RCTs and CCTs comparing surgical with nonsurgical treatments of DIACF were searched by two authors independently. Databases used for searching included Medline, BIOSIS, Cochrane library and Google Scholar. The eligible time was from 1980 to 1st December 2011. There was no restriction to publication language. Key words used for searches were: displaced intra-articular calcaneal fracture, displaced intra-articular fracture of the calcaneus, operation, non-operation, surgery, non-surgery, conservation, randomised controlled trials, clinical controlled trials, controlled trials and randomisation.
Selection criteria
Only RCTs and CCTs that compared surgical with nonsurgical methods for DIACF were taken into consideration. RCTs consist of randomised and quasi-randomised trials. CCTs are trials that test a treatment involving two or more groups with the same disease but without randomisation among the patients. Studies without effective reporting of primary results and those with inadequate data for meta-analysis were excluded.
In all the studies screened for the present meta-analysis, patients recruited were adults with a definite diagnosis and a written informed consent. Their exclusion criteria included operational contraindications, previous calcaneal abnormalities or injuries (e.g. an infection or a tumour), co-existent foot injuries, extra-articular fractures and open injuries [7].
Study identification
Two reviewers independently screened titles of all articles obtained. The abstract of any study that was potentially relevant to the topic was reviewed; a full text was referred to when the information was inadequate from the abstract. Discrepancies were resolved by consensus after discussion.
Data extraction
Two reviewers participated in the extraction of effective data from all eligible studies. One reviewer extracted all the data onto a table prepared in advance. Then, a second reviewer verified the data for accuracy. Disagreement was resolved by discussion and a third reviewer’s opinion was asked for when necessary. Effective data collected from all trials included data available for meta-analysis and information on general characteristics of studies and participants (study setting, study type, number of cases in each group, etc.).
Methodological assessment
Methodological assessment was conducted using the modified Jadad scale [10]. It is an eight-item scale designed to assess randomisation, blinding, withdrawals and dropouts, inclusion and exclusion criteria, adverse effects and statistical analysis (Table 1). The score for each article can range from 0 (lowest quality) to 8 (highest quality). Scores of 4–8 denote good to excellent (high quality) and 0 to 3 poor or low quality. The critical appraisal was conducted by one viewer and verified by another.
Outcomes for meta-analysis
Primary outcomes were classified as anatomical restoration, functional recovery and incidence of complications. Anatomical measurements included changes in Böhler angle, calcaneal height and width. Functional measures covered problems with wearing shoes, resuming pre-injury work and residual pain. Secondary outcome was a sensitivity analysis to compare meta-analyses outcomes between all trials and only RCTs included.
Statistical analysis
Statistical heterogeneity was evaluated using I2 statistics, complying with Quality of Reporting of Meta-Analyses (QUOROM) guidelines [11], which describe the percentage of total variation across studies that is due to heterogeneity rather than chance. I2 can be readily calculated from basic results obtained from a typical meta-analysis as I2 = 100 % × (Q − df)/Q, where Q is Cochrane’s heterogeneity statistic and df is the degrees of freedom [12]. Substantial heterogeneity exists when I2 >50 %. For outcomes when P > 0.05, a fixed-effects model was used in the meta-analysis. Otherwise, a random-effects model was adopted for P ≤ 0.05. Dichotomous data are presented as relative risk (RR) and continuous variables as mean difference (MD), both with 95 % confidence interval (CI). The meta-analysis was performed by RevMan5.1 software (Cochrane Collaboration, Oxford, UK) for outcome measures. A P value of ≤0.05 was considered statistically significant.
Results
Literature search results
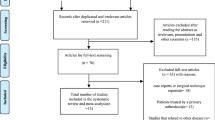
A total of 283 potentially relevant articles were identified (Fig. 1) [13–19]. After reference to titles, abstracts and even full texts, six published RCTs [5–9, 20] and four CCTs [21–24] with a total of 891 patients met all inclusion criteria. Information on general characteristics of studies and participants was listed in Table 2.
Methodological quality assessment
Total trial scores (Table 2) indicate that the quality of most trials was poor based on current rating system. Only four designs [5, 7, 8, 20] scored 4 or more, with a maximum of 6.5 points [7]. The main problem reflected in nearly all studies was absence of methods to assess adverse effects. Apart from three studies [5, 7, 21] using single-blind assessment, most studies failed to use any blinding methods for assessment, which might bring a certain detection bias to the results.
Meta-analysis
Anatomy measures—Böhler angle, calcaneal height and width
Three trials [8, 22, 24] compared the recovery of Böhler angle after surgical and nonsurgical treatments. Results showed that nonsurgically treated patients had a significantly smaller mean Böhler angle than those surgically treated [MD 17.81, 95 % CI (8.96–26.65), P < 0.0001] (Fig. 2).
Changes in post-treatment calcaneal height indicated that the surgical group had significantly less height loss than the non-surgical group [MD 6.55, 95 % CI (2.67–10.43), P = 0.0009] (Fig. 3).
Similarly, patients managed by surgery had a significantly more stable calcaneal width than the nonsurgical patients [MD −7.05, 95 % CI (−7.83 to −6.27), P < 0.00001)] (Fig. 4).
Functional measures—problems in wearing shoes, unable to return to work and residual pain
With regard to shoe fitting difficulties after treatment, outcome according to four RCTs [5, 6, 9, 20] showed that surgically treated patients had fewer problems in wearing shoes than the nonsurgically treated patients [RR 0.42, 95 % CI (0.26–0.68), P = 0.0004] (Fig. 5).
Three RCTs [5, 6, 9] and three CCTs [21, 23, 24] compared the number of patients who failed to resume pre-injury work. Results showed that more surgically treated patients were able to return to pre-injury work [RR 0.59, 95 % CI (0.41–0.84), P = 0.004] (Fig. 6).
A total of 75 of 119 patients in the surgical group compared with 85 of 121 patients in the nonsurgical group had residual pain during the follow-up period. But no significant difference was found between the two groups [RR 0.90, 95 % CI (0.68–1.20), P = 0.49] (Fig. 7).
Incidence of complications
A total of 77 of 338 surgically treated patients compared with 53 of 328 nonsurgically treated patients had complications (22.8 % versus 16.2 %). The significant difference indicated a higher complication rate in the surgical group [RR 1.51, 95 % CI (1.11–2.06), P = 0.008] (Fig. 8).
Sensitivity analysis
Sensitivity analysis was performed by excluding CCTs. We did not perform meta-analyses for the anatomical measurements, as there was only one left for a second analysis after exclusion of the CCTs. The I2, risk ratios, 95 % confidence intervals and P values regarding inability to resume pre-injury work, residual pain and incidence of complications were still similar to the results before exclusion of CCTs (Table 3), indicating that CCTs had no bias on the results of our meta-analyses in functional recovery assessment and complication rate.
Discussion
Results of our meta-analysis confirmed that in DIACF treatment, surgery can effectively restore the anatomical structures of the calcaneus and lead to better functional recovery, though there is a high risk of complications.
Better results in restoring the anatomical structures are probably due to the efficacy of open reduction and internal fixation (ORIF) [25] as well as external fixation [26]. But Ibrahim et al. [8] indicated that no significant difference was found between the two methods in restoration of the Böhler angle [MD 6.50, 95 % CI (−0.34 to 13.34), P = 0.06] and the calcaneal height [MD 1.00, 95 % CI (−2.47 to 4.47), P = 0.57] at 15-year follow-up time. However, this conclusion was based upon a small sample size of only 26 patients. On the other hand, the follow-up durations in the studies included in the present analysis ranged only from 1.2 to five years, far shorter than in the Ibrahim’s [8] study. To clarify this advantage of surgery over non-surgery in DIACF treatment, RCTs or CCTs with much longer follow-ups are needed.
Surgically treated patients had fewer problems in wearing shoes than the nonsurgical group although a potential reduction in such a difference may be due to the tight internal fixation that ensures little change in calcaneal width. Surgery can also result in better functional recovery (more were able to resume pre-injury work). However, as Buckley et al. [7] proposed in a multi-centre RCT, light or moderate workload may lead to better recovery from DIACF, but patients with heavy workload are unlikely to recover well regardless of treatment type. Therefore, subgroup analysis should be performed in sorting of different workload intensities for an accurate conclusion. No significant difference existed in residual pain after surgical and nonsurgical treatments. This is probably because pain tolerance is a subjective assessment or because pain control is essential regardless of treatment choice.
Except for the above three measures to evaluate the efficacy of functional recovery between surgical and nonsurgical treatments, some data not available for meta-analysis were also reported in the eligible studies. O'Farrell et al. [6] reported that surgically treated patients had a significantly longer mean pain-free walking distance (4 km versus 1 km, P < 0.05). They also compared the mean range of subtalar movement and found a significantly larger range of joint motion in the surgical group (P < 0.05). Leung et al. [22] observed that patients managed by surgery had a significantly shorter absence from work (P < 0.05). Many different kinds of assessment scores or scales were adopted for comparisons, such as Creighton-Nebraska Health Foundation assessment sheet, American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot scale, Short Form-36 (SF-36, a general health survey), visual analogue scale (VAS). However, little effective data could be pooled for meta-analysis from these scores or scales, as there was no consistent assessment system or presentation of the results in means and standard deviations.
Although better outcomes were obtained by surgical treatment in anatomical restoration and functional recovery, surgically treated patients had a significantly higher risk of complications than the nonsurgical ones (22.8 % versus 16.2 %, P = 0.008). This is because nearly all the surgical treatments investigated were open. As reported in most eligible trials, an extended lateral L-shaped approach was adopted as a regular surgical procedure. Although this surgical approach may reduce the complication rate complications, such as skin necrosis and wound infection may be difficult to avoid.
In order to reduce the high complication rate caused by open repair surgery, recently, percutaneous repair surgery has been applied in clinical treatment and shows promising results. Tomesen et al. [27] showed excellent results using percutaneous screw fixation in DIACF treatment. Schepers et al. [28] indicated percutaneous distractional reduction and fixation to be a safe technique with overall good results and an acceptable complication rate. Dewall et al. [29] in a retrospective cohort study found that the percutaneous method of reducing and fixing calcaneus fractures minimised complications. Results from Woon et al. [30] showed that the percutaneous approach could avoid soft tissue complications associated with open reduction. According to a recent study, Rammelt et al. [31] found that percutaneous fixation was a reasonable alternative for moderately displaced Type II fractures and provided adequate control over anatomical joint reduction with either subtalar arthroscopy or high-resolution (3-D) fluoroscopy. However, RCTs or CCTs are needed to compare the effectiveness of percutaneous repair versus open repair in DIACF treatment, especially regarding the anatomical joint reconstruction.
After comprehensive search in databases, only six RCTs fulfilled our selection criteria, one of which [8] was a 15-year follow-up report from a previous study [9]. Since the sample size of RCTs was limited, we also searched for CCTs related to the topic. The chief limitations of the studies we recruited are small sample size and short follow-up time, which may affect the stability and reliability of the conclusions. Another limitation is lack of compatible assessment systems or outcome measures, which may lead to loss of abundant data for meta-analysis. The recruitment of CCTs might be the main weakness of our meta-analysis, as they may cause a certain degree selection bias to our results, especially those regarding anatomical measurements. Therefore, CCTs-related results and conclusions should be treated cautiously. One point should be emphasised, that is, outcomes from the sensitivity analysis suggest that surgical treatment can at least bring better functional recovery.
Conclusions
In summary, our meta-analyses confirm that surgical DIACF treatment can result in better restoration of anatomical structures and thus better functional recovery, but it may carry a high risk of complications. Consequently, surgical DIACF treatment may be superior to nonsurgical therapy after trade-off of functional recovery and the price for the functional recovery. We hope there will be more multicentre, large-scale and high quality RCTs with consistent assessment systems comparing DIACF strategies, especially percutaneous with open repairs.
References
Zwipp H, Rammelt S, Barthel S (2004) Calcaneal fractures—the most frequent tarsal fractures. Ther Umsch 61:435–450
McBride D, Ramamurthy C, Laing P (2005) The hindfoot: calcaneal and talar fractures and dislocations, part I. Fractures of the calcaneum. Curr Orthop 94–100
Bajammal S, Tornetta PR, Sanders D, Bhandari M (2005) Displaced intra-articular calcaneal fractures. J Orthop Trauma 19:360–364
Stulik J, Stehlik J, Rysavy M, Wozniak A (2006) Minimally-invasive treatment of intra-articular fractures of the calcaneum. J Bone Joint Surg Br 88:1634–1641
Thordarson DB, Krieger LE (1996) Operative vs. nonoperative treatment of intra-articular fractures of the calcaneus: a prospective randomized trial. Foot Ankle Int 17:2–9
O'Farrell DA, O'Byrne JM, McCabe JP, Stephens MM (1993) Fractures of the os calcis: improved results with internal fixation. Injury 24:263–265
Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, Galpin R (2002) Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am 84-A:1733–1744
Ibrahim T, Rowsell M, Rennie W, Brown AR, Taylor GJ, Gregg PJ (2007) Displaced intra-articular calcaneal fractures: 15-year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury 38:848–855
Parmar HV, Triffitt PD, Gregg PJ (1993) Intra-articular fractures of the calcaneum treated operatively or conservatively. A prospective study. J Bone Joint Surg Br 75:932–937
Oremus M, Wolfson C, Perrault A, Demers L, Momoli F, Moride Y (2001) Interrater reliability of the modified Jadad quality scale for systematic reviews of Alzheimer's disease drug trials. Dement Geriatr Cogn Disord 12:232–236
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
O'Brien J, Buckley R, McCormack R, Pate G, Leighton R, Petrie D, Galpin R (2004) Personal gait satisfaction after displaced intraarticular calcaneal fractures: a 2–8 year followup. Foot Ankle Int 25:657–665
Brauer CA, Manns BJ, Ko M, Donaldson C, Buckley R (2005) An economic evaluation of operative compared with nonoperative management of displaced intra-articular calcaneal fractures. J Bone Joint Surg Am 87:2741–2749
Howard JL, Buckley R, McCormack R, Pate G, Leighton R, Petrie D, Galpin R (2003) Complications following management of displaced intra-articular calcaneal fractures: a prospective randomized trial comparing open reduction internal fixation with nonoperative management. J Orthop Trauma 17:241–249
Kundel K, Funk E, Brutscher M, Bickel R (1996) Calcaneal fractures: operative versus nonoperative treatment. J Trauma 41:839–845
Robb CA, Deans V, Iqbala MJ, Cooper JP (2007) Comparison of non-operative and surgical treatment of displaced calcaneal fractures. Foot 17:169–173
Thornes BS, Collins AL, Timlin M, Corrigan J (2002) Outcome of calcaneal fractures treated operatively and non-operatively. The effect of litigation on outcomes. Ir J Med Sci 171:155–157
Basile A (2010) Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures in elderly patients. J Foot Ankle Surg 49:25–32
Nouraei MH, Moosa FM (2011) Operative compared to non-operative treatment of displaced intra-articular calcaneal fractures. J Res Med Sci 16:1014–1019
Jarvholm U, Korner L, Thoren O, Wiklund LM (1984) Fractures of the calcaneus. A comparison of open and closed treatment. Acta Orthop Scand 55:652–656
Leung KS, Yuen KM, Chan WS (1993) Operative treatment of displaced intra-articular fractures of the calcaneum. Medium-term results. J Bone Joint Surg Br 75:196–201
Rodriguez-Merchan EC, Galindo E (1999) Intra-articular displaced fractures of the calcaneus. Operative vs non-operative treatment. Int Orthop 23:63–65
Xia S, Shi D, Wang Z, Wang X, Lu Y, Wang H, Wu Z, Zhu H (2010) Operative versus nonoperative managements for displaced intraarticular fractures of calcaneus. Chin J Orthop Trauma 12:1089–1091
Grala P, Twardosz W, Tondel W, Olewicz-Gawlik A, Hrycaj P (2009) Large bone distractor for open reconstruction of articular fractures of the calcaneus. Int Orthop 33:1283–1288
Oznur A, Komurcu M, Marangoz S, Tasatan E, Alparslan M, Atesalp AS (2008) A new perspective on management of open calcaneus fractures. Int Orthop 32:785–790
Tomesen T, Biert J, Frolke JP (2011) Treatment of displaced intra-articular calcaneal fractures with closed reduction and percutaneous screw fixation. J Bone Joint Surg Am 93:920–928
Schepers T, Patka P (2009) Treatment of displaced intra-articular calcaneal fractures by ligamentotaxis: current concepts' review. Arch Orthop Trauma Surg 129:1677–1683
DeWall M, Henderson CE, McKinley TO, Phelps T, Dolan L, Marsh JL (2010) Percutaneous reduction and fixation of displaced intra-articular calcaneus fractures. J Orthop Trauma 24:466–472
Woon CY, Chong KW, Yeo W, Eng-Meng YN, Wong MK (2011) Subtalar arthroscopy and flurosocopy in percutaneous fixation of intra-articular calcaneal fractures: the best of both worlds. J Trauma 71:917–925
Rammelt S, Amlang M, Barthel S, Gavlik JM, Zwipp H (2010) Percutaneous treatment of less severe intraarticular calcaneal fractures. Clin Orthop Relat Res 468:983–990
Acknowledgment
The authors thank Professor Allen P. Liang for revision and editing of this manuscript.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jiang, N., Lin, Qr., Diao, Xc. et al. Surgical versus nonsurgical treatment of displaced intra-articular calcaneal fracture: a meta-analysis of current evidence base. International Orthopaedics (SICOT) 36, 1615–1622 (2012). https://doi.org/10.1007/s00264-012-1563-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1563-0