Abstract
Purpose
Primary Spontaneous osteonecrosis of the knee (SPONK) was a result of a subchondral insufficiency fracture based on histopathological examinations. There were few studies examining patients who underwent unicompartmental knee arthroplasty (UKA) for the treatment of primary SPONK. The aim of this study was to investigate (1) patient-reported outcome measure (PROM), (2) survivorship of revision as end point and (3) survivorship of complication as end point in patients with primary SPONK.
Methods
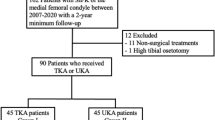
The clinical examinations of a consecutive series of 61 medial UKAs for primary SPONK of the medial femoral condyle from 2008 to 2012 were evaluated retrospectively at our institution. There were 18 males and 43 females with a mean age of 73.7 years (60–91). In all patients, preoperative radiographs were analyzed according to the stage of primary SPONK. We conducted Kaplan–Meier survival analyses using revision and complications for any reasons as the end point.
Results
Mean follow-up was 6.6 years (range 6–10). UKA using Physica ZUK (LIMA Corporate. UD, Italy) for SPONK improved patients’ 2011 Knee Society symptom score, patient satisfaction, patient activities, EQ-5D and postoperative ranges of motion compared with their preoperative status (P < 0.01). Revision surgery was required in one knee (1.6%) due to postoperative fracture of the medial tibial plateau after a fall that occurred 6 months postoperatively. The projected rate of survivorship of UKA was 90.4% at 10 years (95% confidence interval 0.80–1). The projected rate of survivorship with complication at end point was 87.7% at 10 years (95% confidence interval 0.76–0.99).
Conclusion
The present study demonstrated that primary spontaneous osteonecrosis of the knee (SPONK) can be successfully be treated with UKA at a mean follow-up of 6.6 years.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The spontaneous osteonecrosis of the knee (SPONK) was first described in 1968 by Ahlbäck et al. [1]. It is synonymously called avascular necrosis. In 2000, Yamamoto and Bullough [2] proposed a new concept suggesting that SPONK lesion was a result of a subchondral insufficiency fracture based on histopathological examinations. Zywiel et al. [3] described three types of SPONK: type (1) primary development in aged patients; type (2) secondary osteonecrosis following corticosteroid treatment or sickle cell anemia; and type (3) post-arthroscopic osteonecrosis. SPONK may lead to severe pain and dysfunction, resulting in limited available treatment options.
For the treatment of SPONK, Myers et al. [4] and Zhang et al. [5] reported that unicompartmental knee arthroplasty (UKA) is comparable to total knee arthroplasty (TKA), while Heyse et al. [6] and Choy et al. [7] revealed that UKA is an inferior construct. The use of UKA in patients with SPONK, therefore, remains controversial.
We asked whether (1) UKA for primary SPONK improved patient-reported outcome measure (PROM) and (2) UKA for primary SPONK was as durable (as measured by survivorship to revision at a mean follow-up of 6.6 years). The aim of this study was to provide the survivorship of UKAs and patient-reported outcome measure (PROM) for primary SPONK at a mean follow-up of 6.6 years after UKA.
Patients and methods
A consecutive series of 61 medial UKAs operated at our institution between June 2008 and July 2011 were reviewed retrospectively. Mean follow-up was 6.6 years (range 6–10). There were 18 males and 43 females with a mean age of 73.7 years (60–91). Physica ZUK (LIMA Corporate. UD, Italy), a UKA system that is characterized by a metal-backed cemented tibial components, was used for all cases. The inclusion criteria are patients with primary SPONK at the medial femoral condyle of the knee, no flexion contracture more than 15° and no dysfunction of cruciate and collateral ligaments. Patients exhibiting lateral compartment and patellofemoral osteoarthritis were excluded from the study. The present study protocol was reviewed and approved by the institutional review board at our institution.
Surgical procedure
All procedures were operated by the same surgeon (TK) with minimally invasive sub-vastus approach without flip-over or subluxation of the patella. At first, the proximal tibia was prepared using extramedullary system. The resection angle was adjusted to be perpendicular to the mechanical axis of the tibia in the coronal plane and to be parallel to the posterior slope of the original medial plateau in the sagittal plane. The rotational alignment of the tibia was adjusted to be parallel to the medial wall of the intercondylar notch in 90° of flexion. After the resection of the proximal tibia, a spacer block with optimal thickness was inserted to obtain a neutral limb alignment and to fill the extension gap. The distal femur was resected in parallel to the tibial cut surface in order to accommodate the thickness of the femoral implant when the knee was extended. Similarly, the posterior femur was also resected in parallel to the tibial cut surface in flexion to accommodate the thickness of the implant. With trial components in place, the movement and laxity of the knee were confirmed. The thickness of the polyethylene surface was chosen to leave a 2-mm laxity between the components in both extension and flexion. On the first day after UKA surgery, patients were not restricted for weight bearing and were allowed to walk with or without assistive devices after the drainage tube had been removed.
The preoperative plan was developed using 3DCT data of the entire lower extremities in all cases. A postoperative CT scan was obtained 4 weeks after UKA. 3D data of femoral and tibial components were fit to postoperative 3DCT image (Fig. 1). The postoperative 3DCT images femur and tibial were superimposed onto those of the preoperative 3DCT plan using the computer software (ZedView, ZedKnee; LEXI Co., Ltd., Tokyo, Japan). The absolute differences in the prosthetic alignment between the preoperative 3DCT plan and postoperative 3DCT image were measured using six parameters: coronal, sagittal and axial alignment of the femoral and tibial prostheses [8].
Preoperative planning for three-dimensional computed tomography image (3DCT) is shown. Three-dimensional computer-aided design (CAD) data of femoral and tibial components was superimposed to 3DCT image. Blue components (preoperative plan image), yellow components (postoperative component) (color figure online)
Pre- and postoperative 2011 Knee Society score [9] and EQ-5D score [10] were obtained in all patients, and the rate of complications was evaluated.
Statistical analysis
A paired t test was performed in order to compare pre- and postoperative clinical examinations. Kaplan–Meier curves are constructed with 95% confidence intervals (CI) to present estimated survivorship of revision for any reason or radiographic loosening and estimated survivorship with complication as end point [11]. SPSS software (SPSS version 17.0 software: SPSS, Chicago, IL, USA) was used to analyze the data with the level of significance set up to P < 0.05.
Results
Sixty-one UKA knees due to SPONK were included (Aglietti classification [12]: stage III: 16, stage IV: 31, stage V: 14) for the radiological examination preoperatively.
The mean preoperative femoral tibial angle was 182.3° (SD 3.1, 181.3°–185.4°). In other words, all knees were constitutional varus. The mean postoperative femoral tibial angle was 179.5° (SD 3.1, 178.3°–182.8°). The absolute differences in the prosthetic alignment between the preoperative 3DCT plan and postoperative 3DCT image and the rate of outliers (> 3 degrees) are given in Table 1. The mean differences between the preoperative 3DCT plan and 3DCT image and the rate of outliers for prosthesis alignment in six parameters are larger in the axial plane of tibial component.
There were no cases of degenerative changes in the opposite tibiofemoral compartment and osteoarthritis at patellofemoral joint at the last follow-up examination.
The mean range of motion, flexion and extension including maximum and minimum range were significantly improved postoperatively (P < 0.01: Table 2). The Knee Society symptom scores, patient satisfaction scores, activity scores and EQ-5D scores were significantly improved at the last follow-up examination (P < 0.01: Table 2); however, the Knee Society patient expectation scores did not significantly improve at the last follow-up examination (Table 2).
Revision surgery was required in one knee (1.6%) due to postoperative fracture of the medial tibial plateau that occurred at 6 months postoperatively (Fig. 2). Three patients (4.9%) sustained insufficiency fracture of the medial tibial plateau that did not require revision surgery after UKA (5 years, 7 months, 2 years postoperatively), and were treated successfully with a brace immobilization.
In the Kaplan–Meier analysis, the projected rate of survivorship of revision at end point was 90.4% at 10 years (95% confidence interval 0.80–1; Fig. 2), and the projected rate of survivorship with complication at end point was 87.7% at 10 years (95% confidence interval 0.76–0.99; Fig. 3).
The present study did not observe fractures at the femoral and tibial component, deep infection, symptomatic deep vein thrombosis, symptomatic pulmonary embolism, nerve palsy or death that occurred as a result of the operative procedure.
Discussion
The most important fndings of the present study was that UKA for primary SPONK with constitutional varus provided excellent PROMs at a mean follow-up of 6.6 years (range 6–10). The Kaplan–Meier survivorship were 90.4% (95% confidence interval 0.80–1) at 10 years with implant revision at end point and 87.7% (95% confidence interval 0.76–0.99) at 10 years with complications at end point (Fig. 4).
The SPONK with subchondral insufficiency fracture is an uncommon disorder. The surgical technique of SPONK has been a controversial issue. The surgical technique for SPONK includes the joint-preserving method and knee arthroplasty. Koshino et al. described the joint-preserving technique for SPONK with high tibial osteotomy with and without bone grafting or drilling of the lesion in 36 patients at a follow-up ranging 2–8 years. Preoperative pain was relieved and walking ability was improved to 94.6% [13]. Additionally, Mont et al. [14] revealed that 97% of TKA for primary SPONK had a successful clinical outcome. Myers et al. [15] discussed the outcome of TKA and UKA after SPONK in their literature review from 2006. They described favorable postoperative results with both procedures among surgeries operated after 1985. Results seemed to be comparable to those seen after arthroplasty for OA. Poor UKA outcomes were described in their earlier studies as being secondary SPONK with inappropriate patient selection.
There were similar researches for UKA for primary SPONK. Recently, Chalmers et al. [16] reported that 41 UKAs were performed for primary SPONK and mean follow-up was 5 years (2–12). The survivorship that is free of any revision was 93% at both 5 and 10 years. Parratte et al. [17] retrospectively reviewed 31 knees with osteonecrosis. In this cohort, the Kaplan–Meier survivorship was 96.7% at 12 years. Bruni et al. [18] evaluated 84 patients with SPONK. The mean follow-up was 98 months (63–145 months). The Kaplan–Meier survivorship was 89% at 10 years. Langdown et al. [19] described their results of 29 knees (three knees including SPONK of medial tibial plateau) with SPONK operated with UKA at a mean follow-up of 5 years. They experienced no implant failure and concluded that UKA for SPONK was reliable for the investigated term. Similar results were found with primary osteoarthritis patients. Heyse et al. [20] reported that an implant survivorship of 92.7% at an average follow-up of 11 years shows that SPONK can successfully be treated with 52 cases with UKA at a good mid- to long-term follow-up. The Kaplan–Meier survivorship was 93.1% at 10 years with implant revision as end point. Furthermore, our findings in the present study were similar survivorship of UKA for primary SPONK.
None of previous reports have evaluated PROM. In the present study, PROM except patient expectation improved at the last follow-up examination; therefore, UKA for SPONK was better surgery as we expected.
There were a few studies evaluating Aglietti classification, femoral tibial angle and component alignment of patients with complication after UKA for primary SPONK. In this study, four patients who suffered from a medial tibial plateau fracture after UKA were stage V in Aglietti classification.
In finite element method, the risk of medial tibial plateau fracture after UKA elevates with increasing valgus inclination of the tibial component in coronal plane [21, 22]. In contrast, four patients who suffered from a medial tibial plateau (fracture) after UKA had varus inclination of the tibia.
Baker et al. [23] discussed that while UKA was revised for unexplained pain than total knee arthroplasty, and even when these revisions for unexplained pain were discounted, unicompartmental knee arthroplasty still had a significantly greater risk of revision from other reasons than it did for total knee arthroplasty. The revision rate itself only may not be a reliable way to compare different implant designs and should instead be considered based on the reason for failure..
We acknowledge several weaknesses to the present study. A first weakness is the patient population, due to the relative rarity of SPONK. In addition, this study did not establish a control group. A third weakness is that the present study is a retrospective study from single institution, which is susceptible to cause biased selection. We would like to believe that the present study and its findings to be a substantial contribution to the future literature.
In conclusion, primary spontaneous osteonecrosis of the knee (SPONK) can be successfully treated with UKA at a mean follow-up of 6.6 years.
References
Ahlbäck S, Bauer GC, Bohne WH (1968) Spontaneous osteonecrosis of the knee. Arthritis Rheum 11:705–733
Yamamoto T, Bullough PG (2000) Spontaneous osteonecrosis of the knee: the results of subchondral insufficiency fractures. J Bone Joint Surg Am 82(6):858–866
Zywiel MG, McGrath MS, Seyler TM et al (2009) Osteonecrosis of the knee: a review of three disorders. Orthop Clin North Am 40:193–211
Myers TG, Cui Q, Kuskowski M et al (2006) Outcomes of total and unicompartmental knee arthroplasty for secondary and spontaneous osteonecrosis of the knee. J Bone Joint Surg Am 88(Supple 3):76–82
Zhang Q, Guo W, Liu Z et al (2015) Minimally invasive unicompartmental knee arthroplasty in treatment of osteonecrosis versus osteoarthritis: a matched-pair comparison. Acta Orthop Belg 81(2):333–339
Heyse TJ, Khefacha A, Fuchs- Winkelmann S et al (2011) UKA after spontaneous osteonecrosis of the knee: a retrospective analysis. Arch Orthop Traum Surg 131(5):613–617
Choy WS, Kim KJ, Lee SK et al (2011) Medial unicompartmental knee arthroplasty in patients with spontaneous osteonecrosis of the knee. Clin Orthop Surg 3(4):279–284
Yamamura K, Minoda Y, Mizokawa S et al (2017) Novel alignment measurement technique for total knee arthroplasty using patient specific instrumentation. Ach Orthop Trauma Surg 137:401–407
Scuderi GR, Bourne RB, Noble PC et al (2012) The new Knee Society knee scoring system. Clin Orthop Relat Res 470:3–19
Brooks R (1996) The current state of play. Health Policy 37(1):53–72
Aglietti P, Insall JN, Buzzi R et al (1983) Idiopathic osteonecrosis of the knee. Aetiology, prognosis and treatment. BJJ 65(5):588–597
Kaplan EL, Meier P (1958) Nonparametric observation from incomplete observations. J Am Stat Assoc 53:457–481
Koshino T (1982) The treatment of spontaneous osteonecrosis of the knee by high tibial osteotomy with and without bone-grafting or drilling of the lesion. J Bone Joint Surg Am 64(1):47–58
Mont MA, Rifai A, Baumgarten KM et al (2002) Sheldon M, Hungerford DS. Total knee arthroplasty for osteonecrosis. J Bone Joint Surg Am 84(4):599–603
Myers TG, Cui Q, Kuskowski M, Mihalko WM, Saleh KJ (2006) Outcomes of total and unicompartmental knee arthroplasty for secondary and spontaneous osteonecrosis of the knee. J Bone Joint Surg Am 88:76–82
Chalmers BP, Mehrotra KG, Sierra RJ et al (2018) Reliable outcomes and survivorship of unicompartmental knee arthroplasty for isolated compartment osteonecrosis. Bone Joint J 100(4):450–454
Parratte S, Argenson JN, Dumas J et al (2007) Unicompartmental knee arthroplasty for avascular osteonecrosis. Clin Orthop Relat Res 464:37–42
Bruni D, Iacono F, Raspugli G et al (2012) Is unicompartmental arthroplasty an acceptable option for spontaneous osteonecrosis of the knee? Clin Orthop Relat Res 470(5):1442–1451
Langdown AJ, Pandit H, Price AJ et al (2005) Oxford medial unicompartmental arthroplasty for focal spontaneous osteonecrosis of the knee. Acta Orthop 76(5):688–692
Heyse TJ, Khefacha A, Fuchs-Winkelmann S et al (2011) UKA after spontaneous osteonecrosis of the knee: a retrospective analysis. Arch Orthop Trauma Surg 131(5):613–617
Sawatari T, Tsumura H, Iesaka K et al (2005) Three-dimensional finite element analysis of unicompartmental knee arthroplasty—the influence of tibial component inclination. J Orthop Sci 23:549–554
Inoue S, Akagi M, Asada S et al (2016) The valgus inclination of the tibial component increases the risk of medial tibial condylar fractures in unicompartmental knee arthroplasty. J Arthroplasty 31(9):2025–2030
Baker PN, Petheram T, Avery PJ et al (2012) Revision for unexplained pain following unicompartmental and total knee replacement. J Bone Joint Surg Am 94(17):126
Acknowledgements
The authors thank Hiroaki Suzuki for his assistance in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Kaneko, T., Kono, N., Sunakawa, T. et al. Reliable patient-reported outcome measure and survivorship of UKA for primary spontaneous osteonecrosis. Eur J Orthop Surg Traumatol 29, 119–124 (2019). https://doi.org/10.1007/s00590-018-2296-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2296-6