Abstract
Introduction
This study was designed to evaluate the true accuracy of patient specific instrumentation (PSI) for total knee arthroplasty (TKA) using a new 3D measurement method.
Materials and methods
Consecutive 21 patients (30 knees) who underwent TKA using computed tomography (CT)-based PSI were retrospectively evaluated. Mean patient age was 69.2 years (62 to 77). The postoperative three-dimensional (3D) CT image were superimposed onto the preoperative 3D CT plan and measured the absolute difference in the prosthetic alignment using six parameters: coronal, sagittal, and axial alignment of the femoral and tibial prostheses. Cases in which the difference in the prosthetic alignment was greater than 3° were considered outliers.
Results
For the femoral prosthesis, mean absolute differences between the preoperative 3D CT plan and postoperative 3D CT image were not significantly different and the rates of outliers were 10.0, 33.3, 23.3% in the coronal, sagittal, and axial planes. For the tibial prosthesis, mean absolute differences were significantly larger in the axial plane than in the coronal and sagittal planes (p < 0.001) and the rates of outliers were 23.3, 36.7, 63.3% in the coronal, sagittal, and axial planes. The rates of outliers for the axial alignment of tibial prosthesis were significantly higher than for the other five planes (p = 0.006).
Conclusions
The rotation of the tibial prosthesis with CT-based PSI was less accurate in the axial plane than in the other five planes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Alignment of the prosthesis is one of the most important factors that affects the long-term clinical results of total knee arthroplasty (TKA) [1–5]. To improve the prosthetic alignment and decrease cases of prosthetic outlier, patient specific instrumentation (PSI) have recently been introduced for TKA.
PSI is based on data from either magnetic resonance imaging (MRI) or computed tomography (CT). Preoperatively, a three-dimensional (3D) plan for prosthetic alignment is performed using computer software. PSI is designed to correctly reproduce the preoperative 3D plan during the operation. Intraoperatively, PSI is fit on the distal femur and proximal tibia. According to the PSI, distal femur and proximal tibia are cut and femoral and tibial prostheses are implanted. Therefore, to evaluate the true accuracy of PSI, the preoperative 3D plan and postoperative 3D prosthetic alignment should be directly compared. However, previous reports on PSI have only measured the postoperative prosthetic position from the postoperative mechanical axis or anatomical landmarks of femur and tibia [6–8]; thus, these reports did not consider the preoperative 3D plan, and they did not evaluate the accuracy of PSI. It was hypothesized that PSI provided accurate postoperative prosthetic position.
The present study aimed to compare the alignment of the preoperative 3D CT plan and postoperative 3D CT, and evaluate the accuracy of PSI for use during TKA.
Patients and methods
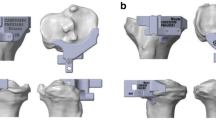
Consecutive 30 knees (21 patients) which underwent TKA using PSI (Prophecy; MicroPort Orthopedics, Inc., Arlington, TN, USA) were retrospectively evaluated (Fig. 1). Four knees were male and 26 knees were female. Mean patient age was 69.2 years (range 62–77 years) and mean body mass index was 27.0 kg/m2 (range 20.9–36.9 kg/m2). Mean preoperative hip knee ankle angle was 12.0 degrees varus (range −0.5–30.0 degrees varus). The preoperative plan was developed using 3D CT data of the whole leg (Fig. 2). PSI was designed on the basis of this preoperative 3D CT plan. A posterior stabilized prosthesis (Evolution PS; MicroPort Orthopedics, Inc.) was used in all cases. All operations were performed by one surgical team. The knees were exposed using a medial parapatellar approach, and the anterior and posterior cruciate ligaments were resected. This study was approved by the institutional review boards of our hospitals, and all patients provided informed consent. A postoperative CT scan was obtained 2 weeks after TKA. 3D data of femoral and tibial components were fit to postoperative 3D CT image (Fig. 3) The femur and tibia of the postoperative 3D CT image were superimposed onto the femur and tibia of the preoperative 3D CT plan using computer software (ZedView, ZedKnee; LEXI Co., Ltd., Tokyo, Japan) (Fig. 4). The absolute difference in the prosthetic alignment between the preoperative 3D CT plan and postoperative 3D CT image was measured using six parameters: coronal, sagittal, and axial alignment of the femoral and tibial prostheses. Cases in which the difference in the prosthetic alignment between the preoperative 3D CT plan and postoperative 3D CT image was greater than 3°, were considered outliers [9]. Translations of components were also measured in anterior-posterior (AP), mediolateral (ML), and superior-inferior (SI) directions. The computer software expressed the alignment (degrees) to one decimal place and the translation (mm) to two decimal places.
a The femur of the postoperative 3-dimensional (3D) computed tomography (CT) image was superimposed onto the femur of the preoperative 3D CT plan. b The tibia of the postoperative 3D CT image was superimposed onto the tibia of the preoperative 3D CT plan. Differences in the prosthetic alignment between the preoperative 3D CT plan (red) and postoperative 3D CT image (blue) were measured
Statistical analysis
To evaluate the intraobserver reliability, all six parameters were repeatedly measured by an expert surgeon (K.Y.) in 20 knees at 4-week intervals to evaluate reproducibility. To evaluate the interobserver reliability, all six parameters were repeatedly measured by another assessor (H.H.) in these 20 knees. Results of the interobserver and intraobserver reliability were analyzed using intraclass and interclass correlation coefficients (ICCs). The ICCs were considered poor (less than 0.40), moderate (0.40–0.60), good (0.61–0.80), and very good (0.81–1.00) [10, 11]. One-way analysis of variance was used to compare the absolute difference in prosthetic alignment among the six parameters. The Pearson’s Chi-square test and Fisher’s exact test were used to determine the outliers. A sample size calculation was performed using EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [12], and the results showed that a sample of 24 knees was required to achieve a power of 0.8 to detect a significant difference (α = 0.05, two-sided significance level). All data analyses were performed with SPSS, version 23.0 (SPSS Inc., Chicago, IL, USA). The level of significance was set at 0.05.
Results
The intraobserver and interobserver reliabilities of this measurement method are shown in Table 1. The ICCs of all six parameters were more than 0.9 (very good). Absolute differences between two measurements of one observer and between two observers were less than 1°.
Absolute differences in the prosthetic alignment between the preoperative 3D CT plan and postoperative 3D CT image are shown in Table 2. For the femoral prosthesis, absolute differences between the preoperative 3D CT plan and postoperative 3D CT image were not significantly different in the coronal, sagittal, and axial planes. For the tibial prosthesis, absolute differences between the preoperative 3D CT plan and postoperative 3D CT image were significantly larger in the axial plane than in the coronal and sagittal planes (p < 0.001). The outliers are shown in Table 3. The rates of outliers for the axial alignment of tibial prosthesis were significantly higher than for the other five planes (p = 0.006). Translations of component (AP, ML, and SI) are shown in Table 4.
Discussion
This is the first study that superimposed a preoperative 3D CT plan on a postoperative 3D CT image, and directly compared the prosthetic alignment between the preoperative 3D CT plan and postoperative 3D CT image after TKA using PSI. The most important finding of this study was that this new method for 3D analysis of PSI had a very high intraobserver and interobserver reliabilities. PSI have been introduced to improve the prosthetic alignment and decrease cases of prosthetic outlier [13–18]. Some previous reports have shown that PSI improved the prosthetic alignment [19, 20], whereas others have shown that compared to conventional methods, PSI did not improve the prosthetic alignment [21, 22]. Therefore, it is still controversial whether PSI improves the prosthetic alignment. One of the reasons why the accuracy of PSI is still controversial is that the measurement methods of prosthetic alignment in previous reports were not accurate. Most of previous reports used postoperative radiographs [8, 23, 24]. However, measuring prosthetic alignment using radiographs has several limitations. First, the measurement of prosthetic alignment using radiographs is affected by the rotation of the leg [25]. Therefore, a two-dimensional measurement using radiographic data is theoretically less accurate than a 3D measurement using CT [26]. Second, although the preoperative plan using PSI was 3D, a postoperative evaluation using radiographs can only provide 2D data. Prosthetic alignment should be evaluated three-dimensionally, because the preoperative plan using PSI was 3D. Furthermore, rotational alignment cannot be evaluated using radiographs. To evaluate the accuracy of 3D PSI, postoperative 3D analysis should be performed. Evaluating prosthetic alignment using CT will improve the measurement accuracy of PSI. Previous reports that used CT data measured the angle between the prosthetic position and the coronal, sagittal, and axial baselines that were drown on the postoperative CT data [6, 27]. It is difficult to draw the same baselines on preoperative CT and postoperative CT data, because the bony landmarks on the distal femur and proximal tibia are resected postoperatively. The error in the baseline set-up between preoperative CT and postoperative CT may results in a measurement error [28]. To eliminate such a measurement error, the postoperative 3D CT image was superimposed on the preoperative 3D CT plan and directly compared the prosthetic alignment of the preoperative 3D plan and the prosthetic alignment of the postoperative 3D image. The present study showed that this new measurement method had excellent interobserver and intraobserver reliabilities. Regarding the use of PSI for a femoral prosthesis, outliers greater than 3 degrees have been reported in 0–15.0% of cases in the coronal plane [6–9, 18, 19, 22, 23, 29–31], 9.5–52.5% in the sagittal plane [7–9, 22, 23, 29, 31], and 2.2–23.0% in the axial plane [7, 9, 31, 32]. Regarding the use of PSI for a tibial prosthesis, outliers have been reported in 0–18.4% of cases in the coronal plane [7–9, 19, 22, 23, 29, 31, 33], and 20.0–65.0% in the sagittal plane [7–9, 22, 29, 31, 33]. No studies have evaluated outliers in the axial plane in terms of using PSI for a tibial prosthesis. The present study showed that more outliers occurred in the axial plan of tibial prosthesis than in the other five parameters. There will be two reasons why more outliers occurred in the axial plan of tibial prosthesis. First, the contact area between the bone and PSI was smaller in the tibia than in the femur (Fig. 1). A smaller contact area may result in errors in the tibial PSI. Second, no markers were used to guide the tibial component rotation after the proximal tibia was resected. The pins used to fix the tibial cutting jig are not parallel; instead, they are 20° external to the tibial component rotation. Tibial rotation was determined manually; thus, the tibial rotation became less accurate. To improve rotational alignment of the tibial component, the design of the PSI should be improved. The contact area between the bone and PSI should be enlarged, and a rotational guide should be added even after tibial bone resection. This precise 3D analysis can clarify these problems associated with PSI, and it will help improve the PSI design.
This study has a limitation. Only one PSI system was evaluated. There are several PSI with different design features. Therefore, the results of this study cannot be applied to other PSI systems. Further study should be performed to clarify the accuracy of each PSI system.
Conclusions
This is the first study that superimposed a preoperative 3D CT plan on a postoperative 3D CT image and directly compared the prosthetic alignment between the preoperative 3D CT plan and postoperative 3D CT image after TKA using PSI. This new measurement method had a high reliability. In addition, the rotation of the tibial prosthesis was less accurate in the axial plane than in the other five planes. This reliable measurement method will be useful for evaluating PSI, and it may help improve the design of PSI.
References
Lombardi AV Jr, Berend KR, Ng VY (2011) Neutral mechanical alignment: a requirement for successful TKA: affirms. Orthopedics 34(9):e504–e506. doi:10.3928/01477447-20110714-40
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 24(6 Suppl):39–43. doi:10.1016/j.arth.2009.04.034
Liu HX, Shang P, Ying XZ, Zhang Y (2015) Shorter survival rate in varus-aligned knees after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3781-7
Halder A, Kutzner I, Graichen F, Heinlein B, Beier A, Bergmann G (2012) Influence of limb alignment on mediolateral loading in total knee replacement: in vivo measurements in five patients. J Bone Joint Surg Am 94(11):1023–1029. doi:10.2106/JBJS.K.00927
Ritter MA (2009) The anatomical graduated component total knee replacement: a long-term evaluation with 20-year survival analysis. J Bone Joint Surg Br 91(6):745–749. doi:10.1302/0301-620X.91B6.21854
Marimuthu K, Chen DB, Harris IA, Wheatley E, Bryant CJ, MacDessi SJ (2014) A multi-planar CT-based comparative analysis of patient-specific cutting guides with conventional instrumentation in total knee arthroplasty. J Arthroplasty 29(6):1138–1142. doi:10.1016/j.arth.2013.12.019
Roh YW, Kim TW, Lee S, Seong SC, Lee MC (2013) Is TKA using patient-specific instruments comparable to conventional TKA? A randomized controlled study of one system. Clin Orthop Relat Res 471(12):3988–3995. doi:10.1007/s11999-013-3206-1
Boonen B, Schotanus MG, Kerens B, van der Weegen W, van Drumpt RA, Kort NP (2013) Intra-operative results and radiological outcome of conventional and patient-specific surgery in total knee arthroplasty: a multicentre, randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 21(10):2206–2212. doi:10.1007/s00167-013-2620-y
Jiang J, Kang X, Lin Q, Teng Y, An L, Ma J, Wang J, Xia Y (2015) Accuracy of patient-specific instrumentation compared with conventional instrumentation in total knee arthroplasty. Orthopedics 38(4):e305–e313. doi:10.3928/01477447-20150402-59
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Walter SD, Eliasziw M, Donner A (1998) Sample size and optimal designs for reliability studies. Stat Med 17(1):101–110
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48(3):452–458. doi:10.1038/bmt.2012.244
Anwar R, Kini SG, Sait S, Bruce WJ (2016) Early clinical and radiological results of total knee arthroplasty using patient-specific guides in obese patients. Arch Orthop Trauma Surg 136(2):265–270. doi:10.1007/s00402-015-2399-z
Hommel H, Perka C (2015) Gap-balancing technique combined with patient-specific instrumentation in TKA. Arch Orthop Trauma Surg 135(11):1603–1608. doi:10.1007/s00402-015-2315-6
Hommel H, Perka C, Pfitzner T (2016) Preliminary results of a new surgical technique in total knee arthroplasty (TKA) using the native ligament tension for femoral implant positioning in varus osteoarthritis. Arch Orthop Trauma Surg 136(7):991–997. doi:10.1007/s00402-016-2480-2
Hafez MA, Chelule KL, Seedhom BB, Sherman KP (2006) Computer-assisted total knee arthroplasty using patient-specific templating. Clin Orthop Relat Res (444):184–192. doi:10.1097/01.blo.0000201148.06454.ef
Howell SM, Kuznik K, Hull ML, Siston RA (2008) Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics 31(9):857–863
Noble JW Jr, Moore CA, Liu N (2012) The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty 27(1):153–155. doi:10.1016/j.arth.2011.07.006
Chareancholvanich K, Narkbunnam R, Pornrattanamaneewong C (2013) A prospective randomised controlled study of patient-specific cutting guides compared with conventional instrumentation in total knee replacement. Bone Joint J 95-B(3):354–359. doi:10.1302/0301-620X.95B3.29903
Daniilidis K, Tibesku CO (2014) A comparison of conventional and patient-specific instruments in total knee arthroplasty. Int Orthop 38(3):503–508. doi:10.1007/s00264-013-2028-9
Sassoon A, Nam D, Nunley R, Barrack R (2015) Systematic review of patient-specific instrumentation in total knee arthroplasty: new but not improved. Clin Orthop Relat Res 473(1):151–158. doi:10.1007/s11999-014-3804-6
Yan CH, Chiu KY, Ng FY, Chan PK, Fang CX (2015) Comparison between patient-specific instruments and conventional instruments and computer navigation in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 23(12):3637–3645. doi:10.1007/s00167-014-3264-2
Boonen B, Schotanus MG, Kort NP (2012) Preliminary experience with the patient-specific templating total knee arthroplasty. Acta Orthop 83(4):387–393. doi:10.3109/17453674.2012.711700
Chen JY, Yeo SJ, Yew AK, Tay DK, Chia SL, Lo NN, Chin PL (2014) The radiological outcomes of patient-specific instrumentation versus conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(3):630–635. doi:10.1007/s00167-013-2638-1
Lee YS, Lee BK, Lee SH, Park HG, Jun DS, Moon do H (2013) Effect of foot rotation on the mechanical axis and correlation between knee and whole leg radiographs. Knee Surg Sports Traumatol Arthrosc 21(11):2542–2547. doi:10.1007/s00167-013-2419-x
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Joint Surg Br 93(5):629–633. doi:10.1302/0301-620X.93B5.25893
Leeuwen JA, Grogaard B, Nordsletten L, Rohrl SM (2015) Comparison of planned and achieved implant position in total knee arthroplasty with patient-specific positioning guides. Acta Orthop 86(2):201–207. doi:10.3109/17453674.2014.985154
Okamoto S, Mizu-Uchi H, Okazaki K, Hamai S, Tashiro Y, Nakahara H, Iwamoto Y (2016) Two-dimensional planning can result in internal rotation of the femoral component in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24(1):229–235. doi:10.1007/s00167-014-3370-1
Hamilton WG, Parks NL, Saxena A (2013) Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty 28(8 Suppl):96–100. doi:10.1016/j.arth.2013.04.049
MacDessi SJ, Jang B, Harris IA, Wheatley E, Bryant C, Chen DB (2014) A comparison of alignment using patient specific guides, computer navigation and conventional instrumentation in total knee arthroplasty. Knee 21(2):406–409. doi:10.1016/j.knee.2013.11.004
Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J (2014) Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res 472(1):263–271. doi:10.1007/s11999-013-2997-4
Heyse TJ, Tibesku CO (2014) Improved femoral component rotation in TKA using patient-specific instrumentation. Knee 21(1):268–271. doi:10.1016/j.knee.2012.10.009
Conteduca F, Iorio R, Mazza D, Caperna L, Bolle G, Argento G, Ferretti A (2012) Are MRI-based, patient matched cutting jigs as accurate as the tibial guides? Int Orthop 36(8):1589–1593. doi:10.1007/s00264-012-1522-9
Acknowledgements
We thank Hidenori Harigae for his assistance in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yukihide Minoda has received research grants from Microport Japan.
Rights and permissions
About this article
Cite this article
Yamamura, K., Minoda, Y., Mizokawa, S. et al. Novel alignment measurement technique for total knee arthroplasty using patient specific instrumentation. Arch Orthop Trauma Surg 137, 401–407 (2017). https://doi.org/10.1007/s00402-017-2628-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-017-2628-8