Abstract
Objective
To compare clinical outcomes of unicompartmental knee arthroplasty (UKA) versus total knee arthroplasty (TKA).
Methods
A systematic review and meta-regression to compare postoperative outcomes of pain VAS, knee function score, range of motion, complications and revision surgery rates between UKA and TKA were conducted. Relevant randomized controlled trials were identified from MEDLINE and Scopus from inception to August 29, 2014.
Results
Three of 1056 studies were eligible; two, three, two, three and three studies were included in pooling of pain visual analog score (VAS), Knee Society Score (KSS) and Bristol Knee Score (BKS), maximum knee flexion, postoperative complications (aseptic loosening, progressive degenerative joint disease of lateral compartment, bearing dislocation, DVT, fractures and infection) and revision rates, respectively. The unstandardized mean difference (UMD) of the function scores (KSS, BS) for UKA was 1.62 (95 % CI −1.17, 4.42) better than TKA and for pain score was 0.1 (95 % CI −3.54, 3.73) higher than TKA, but both without statistical significance. UKA was more likely to show higher mean maximum knee flexion with a UMD of 1.88 (95 % CI −0.54, 4.30) when compared to TKA, but was also not statistically significant. UKA had a statistically significant lower chance of postoperative complications by 0.35 U (95 % CI 0.12, 0.98) when compared to TKA, but had higher revision rates than TKA with a value of 5.36 (95 % CI 1.06, 27.08).
Conclusion
In short-term outcomes (5 years or less, with follow-up of 0–5 years), TKA had higher postoperative complications than UKA, but had lower revision rates. There was only one study that reported long-term survivorship (more than 5 years, with follow-up of 5–15 years). Further research that assesses long-term survivorship is necessary to better evaluate UKA and TKA in the treatment of unicompartmental knee osteoarthritis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The best treatment options for patients with medial compartment osteoarthritis (OA) of the knee [18] are still controversial. Total knee arthroplasty (TKA) and unicompartmental knee arthroplasty (UKA) are both utilized to treat OA of the knee. TKA has long been considered the gold standard of operative intervention for knee arthrosis due to demonstrated predictability, durability and effectiveness in the treatment of pain and restoration of function [1, 4, 7, 9, 16]. Many authors have shown good long-term survivorship following UKA as well as better kinematics [3, 11, 13], pain scores, function, lower complication rates and increased longevity [16, 26, 27] in OA knee. Some studies report UKA results that are comparable to those of TKA [24]. The debate of whether UKA offers clinical and longevity advantages over TKA for isolated symptomatic OA of the knee has continued to generate substantial controversy in the orthopedic community. Randomized controlled trials (RCTs) represent the best study design to compare UKA with TKA. However, no consistent results have been shown in these published randomized trials [5, 20, 23]. To the best of our knowledge, one meta-analysis [28] that compares UKA with TKA has been published over the past few years that pooled only one RCT study [19, 20] with 6 other prospective cohort studies [2, 6, 12, 15, 17, 27], and found that there was no clinically relevant or statistically significant improvement in UKA when compared to TKA. However, this meta-analysis did not consider sources of heterogeneity (e.g., preoperative range of motion, age, sex, and body mass index), and publication bias was not assessed. Moreover, other RCTs [5, 23, 25] have since been published. Therefore, a meta-analysis and systematic review of randomized clinical studies were performed to compare UKA and TKA with the aim of updating current data regarding knee pain, knee scores, function and complications.
Materials and methods
MEDLINE and Scopus databases were used for identifying relevant studies published in English since the date of inception to September 11, 2014. The PubMed and Scopus search engines were used to locate studies with following search terms: UKA and TKA and clinical trial. Search strategies for MEDLINE and Scopus are described in detail in the appendix. References from the reference lists of included trials and previous systematic reviews were also explored.
Selection of studies
Identified studies were first selected based on titles and abstracts by two independent authors (J.K. and A.A.). Full papers were retrieved if a decision could not be made from the abstracts. Disagreements were resolved by consensus and discussion with a third party (S.M.). Reasons for ineligibility or exclusion of studies were recorded and described.
Inclusion criteria
Randomized controlled trials, quasi-experimental designs and prospective comparative studies that compared clinical outcomes between UKA and TKA were eligible if they met the following criteria:
-
Compared clinical outcomes between UKA and TKA.
-
Compared at least one of following outcomes: knee visual analog pain score (VAS), knee range of motion (ROM) in flexion and extension, Knee Society Score (KSS) and Knee Society Function Score (FS), Bristol Knee Score (BKS), early postoperative complications [aseptic loosening, progressive degenerative joint disease of lateral compartment, bearing dislocation, infection, deep vein thrombosis (DVT), fracture] and revision surgery.
-
Had sufficient data to extract and pool, i.e., the reported mean, standard deviation (SD), the number of subjects according to treatments for continuous outcomes, and the number of patients according to the treatment for dichotomous outcomes.
When eligible papers had insufficient information, we contacted authors by e-mail (up to three consecutive e-mails if there was no reply) for additional information. If authors did not provide additional data, the study was excluded from the review.
Data extraction
Two reviewers (J.K. and A.A.) independently performed data extraction using standardized data extraction forms. General characteristics of the study [i.e., mean age, gender, body mass index (BMI), mean follow-up time, range of motion (ROM) and functional scores (KSS, BKS) at baseline] were extracted. The number of subjects, mean and SD of continuous outcomes (i.e., knee ROM), knee functional scores (KSS, BKS) between the groups were extracted. Cross-tabulated frequencies between treatment and all dichotomous outcomes (early postoperative complications and revisions) were also extracted. Any disagreements were resolved by discussion and consensus with a third party (S.M.).
Risk of bias assessment
Two authors (J.K. and A.A.) independently assessed the risk of bias for each study following suggestion in the PRISMA guideline [14]. Six domains were assessed, which included sequence generation, allocation concealment, blinding (participant, personnel and outcome assessors), incomplete outcome data, selective outcome reporting and other sources of bias. Disagreements between two authors were resolved by consensus and discussion with a third party (S.M.). Level of agreement for each domain and the overall domains were assessed using the Kappa statistics.
Outcomes
The outcomes of interests included knee pain visual analog scores (VAS), Knee Society scores for pain, knee ROM, Knee Society scores for function, Bristol knee score, rates of early postoperative complications and revision. These outcomes were measured as reported in the original studies, which were by VAS and Knee Society pain scores, goniometer measurement of knee ROM for maximum knee flexion; Knee Society Score (KSS) and (BKS) for function. For knee pain VAS and KSS, lower values are equivalent to better outcomes. For knee ROM, higher values are equivalent to better outcomes. For the functional scores including KSS (0–100) and BKS (0–100) scores, higher scores reflect better function. Early postoperative complications (aseptic loosening, progressive degenerative joint disease of lateral compartment, bearing dislocation, infection, deep vein thrombosis, fracture) and revision were considered.
Statistical methods
For continuous outcomes (i.e., knee VAS, ROM, KSS and BKS), the mean difference between UKA and TKA was estimated for each study. Unstandardized mean difference was applied for pooling outcomes across studies. Before pooling, intervention effects were assessed on whether they varied or were heterogeneous across included studies. Heterogeneity of mean differences was checked using the Q statistic, and the degree of heterogeneity was also quantified using the I 2 statistic. If heterogeneity was significant or I 2 > 25 %, the UMD was estimated using a random effects model, otherwise a fixed effects model was applied.
For dichotomous outcomes, the odds ratio (OR) for complications (aseptic loosening, progressive degenerative joint disease of lateral compartment, bearing dislocation, infection, DVT and fracture) and for revision rates was estimated for each study. Heterogeneity of OR across studies was assessed using the same method as mentioned previously. If heterogeneity was present, the random effects by Dersimonian and Laird method were applied for pooling OR; otherwise, the fixed effects by inverse variance method was applied.
Meta-regression was applied for exploring the cause of heterogeneity by fitting a covariable [e.g., mean age, BMI, follow-up time, type of surgery (unilateral or bilateral), preoperative VAS, ROM and percentage of female] in the meta-regression model. Subgroup or sensitivity analysis was then performed according to the results of meta-regression. Publication bias was assessed using contour funnel plots [21, 22] and Egger tests [8]. Asymmetry of the funnel plot might be due to missing data in some studies, in which the results that were negative might not have been published and thus could not be identified. The metatrim and fill method was used to estimate the number of studies that might be missing and to adjust the pooled estimate [1]. All analyses were performed using STATA version 13.0. p value < 0.05 was considered statistically significant, except for the test of heterogeneity where <0.10 was used.
Results
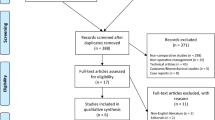
Eighty-three and 1026 studies were identified from MEDLINE and Scopus respectively, (Fig. 1); 55 studies were duplicates, leaving 1054 studies to review titles and abstracts. Of these, four RCT studies [5, 20, 23, 25] were reviewed and data were extracted. Characteristics of the four studies [5, 20, 23, 25] are described in Table 1. Two [20, 25] of the four studies were performed at the same center and the same time period, but difference outcome of interest. Knee function was reported using the KSS in two studies [5, 23] and BKS in one study [20]. Two studies [23, 25] reported postoperative ROM for maximum knee flexion. Knee pain was reported using the VAS in one study [25] and KSS in one study [5]. (composite outcomes of DVT, infection and fracture) were reported in three studies [5, 20, 23], and revision knee arthroplasty in three studies [5, 20, 23]. Mean age, BMI and mean follow-up of participants varied from 60.5 to 73 years, 30 years and 4–5 years, respectively. Percentages of female gender ranged from 44 to 66 %. All four studies were posterior stabilized TKA implants. Three studies [5, 20, 25] included fixed-bearing UKA implants, whereas only one study [23] used a mobile-bearing UKA implant.
Risk of bias in included studies
Risk of bias is described in Table 2.
Outcome
Knee function, pain and range of motion (ROM)
Knee function
Three studies reported mean function scores (two studies were KSS, and one study was BKS) between UKA and TKA groups with 112 and 114 patients. The pooled UMD varied moderately across studies (Chi-square = 4.17, df = 2, p = 0.124, I 2 = 52.1 %) were 1.62 (95 % CI −1.17, 4.42), indicating that the UKA group had function scores better than the TKA group, but without statistically significant (Fig. 2). None of the covariables could explain the heterogeneity. There was no evidence of publication bias on Egger’s test or contour funnel plot (coefficient = 5.72, SE = 2.87, p = 0.296).
Knee pain
Two studies with 84 and 86 patients, respectively, compared mean pain scores (one study was VAS, and another one study was KSS) between UKA and TKA groups (Table 3). Mean difference varied highly across studies (Chi-square = 5.57, df = 1, p = 0.018, I2 = 82.1 %) with an UMD of 0.1 (95 % CI −3.54, 3.73), indicating that the UKA group had no statistically significant difference of pain when compared to the TKA group (Fig. 2).
Postoperative knee range of motion for maximum knee flexion
Two studies with 78 and 80 patients compared the mean values of maximum knee flexion between UKA and TKA (Table 3). Mean difference varied highly across studies (Chi-square = 18.87, df = 1, p < 0.05, I 2 = 94.7 %) with an UMD of 3.56 (95 % CI −.52, 14.63). The mean difference of maximum knee flexion was 3.56°, but the two techniques did not show a significant difference (Fig. 2).
Complication and revision outcomes
Three studies reported early postoperative complications and revision surgery within the UKA and TKA groups (Table 4). Risk of complications was lower in the UKA group (Chi-square = 0.22, df = 2, p = 0.897, I 2 = 0 %, Fig. 3) with a pooled RR of 0.39 (95 % CI 0.16, 1.00) when compared to the TKA group, indicating that the chance of having postoperative complications was lower by approximately 60 percent in the UKA group when compared to the TKA group. However, the risk of revision surgery was higher in the UKA group (Chi-square = 2.13, df = 2, p = 0.345, I 2 = 6 %, Fig. 3) with a pooled RR of 5.36 (95 % CI 1.06, 27.08) when compared to the TKA group, indicating that the chance of requiring revision surgery was approximately 5.4 times higher in the UKA group when compared to the TKA group.
Neither contour funnel nor Egger’s test suggested evidence of publication bias.
Discussion
In the UK and North America, UKA has increased in popularity in recent years. Many authors have shown good long-term survivorship following UKA as well as better kinematics and function. However, some surgeons still regard UKA as a temporary procedure and believe that patients over 60 years of age are best treated with a TKA. Randomized controlled trials represent the best study design to compare UKA with TKA. However, no consistent results have been shown in these published randomized trials. The use of both UKA and TKA have been increasing worldwide.
This review suggests that UKA has no significant difference in outcomes for knee scores, function scores and ROM than total knee arthroplasty. Patients who underwent UKA were approximately five times more likely to undergo revision surgery than patients who underwent TKA. On the other hand, patients who underwent UKA were approximately 60 % less likely to have early postoperative complications after surgery than patients who underwent TKA.
Previous meta-analysis [28] has shown that UKA has a better postoperative ROM with improved pain relief and function compared to TKA, but in terms of knee function did not show a statistically significant difference. Postoperative complications in the TKA group were higher when compared to the UKA group, whereas revision rates were higher in the UKA group when compared to the TKA group. Only one study was a RCT with a total of 102 subjects, and six studies were cohort studies. This review included three more RCTs with a total of 226 subjects. There was no difference in postoperative function, pain and ROM in the knee between the two groups.
This study has several strengths. First of all, this study included 4 RCTs in the pooling of relevant clinical outcomes (i.e., postoperative functional scores, pain score, range of motion, early postoperative complications and revision rates) of UKA and TKA. Secondly, possible causes of heterogeneity were explored if covariate data at baseline (e.g., mean age, percent female, follow-up times, unilateral or bilateral TKA) were available. However, due to the small number of studies a sensitivity analysis could not be done. Publication bias for each outcome was also assessed. However, due to the small number of studies selected for this meta-analysis a funnel plot was not drafted to display publication bias.
There are some limitations in this study. This study did not pool a social outcome such as quality of life due to the fact that there was insufficient data. All studies had a mean follow-up time of about 4–5 years, and thus, long-term effects of UKA and TKA are still in question.
The quality of evidence was also assessed for each outcome following suggestion (Guyatt et al. 2008) [10] (Table 5). The quality of evidence was intermediate strength for all outcomes.
Conclusion
In short-term outcomes (5 years or less, with follow-up of 0–5 years), TKA had higher early postoperative complications than UKA, but had lower surgical revision rates. There was only one study that reported long-term survivorship (more than 5 years, with follow-up of 5–15 years). Further research that assesses long-term survivorship is necessary to further evaluate UKA and TKA in the treatment of unicompartmental knee OA.
References
Aglietti P, Buzzi R, De Felice R, Giron F (1999) The insall-burstein total knee replacement in osteoarthritis: a 10-year minimum follow-up. J Arthroplasty 14(5):560–565
Amin AK, Patton JT, Cook RE, Gaston M, Brenkel IJ (2006) Unicompartmental or total knee arthroplasty?: results from a matched study. Clin Orthop Relat Res 451:101–106
Banks SA, Fregly BJ, Boniforti F, Reinschmidt C, Romagnoli S (2005) Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg, Sports Traumatol, Arthrosc 13(7):551–556
Colizza WA, Insall JN, Scuderi GR (1995) The posterior stabilized total knee prosthesis. Assessment of polyethylene damage and osteolysis after a ten-year-minimum follow-up. J Bone Joint Surg Am 11:1713–1720
Costa CR, Johnson AJ, Mont MA, Bonutti PM (2011) Unicompartmental and total knee arthroplasty in the same patient. J Knee Surg 24(4):273–278
Dalury DF, Fisher DA, Adams MJ, Gonzales RA (2009) Unicompartmental knee arthroplasty compares favorably to total knee arthroplasty in the same patient. Orthopedics 32 (4)
Diduch DR, Insall JN, Scott WN, Scuderi GR, Font-Rodriguez D (1997) Total knee replacement in young, active patients. Long-term follow-up and functional outcome. J Bone Joint Surg Am 79(4):575–582
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634
Fetzer GB, Callaghan JJ, Templeton JE, Goetz DD, Sullivan PM, Kelley SS (2002) Posterior cruciate-retaining modular total knee arthroplasty: a 9- to 12-year follow-up investigation. J Arthroplasty 17(8):961–966
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ, Group GW (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336(7650):924–926
Hollinghurst D, Stoney J, Ward T, Gill HS, Newman JH, Murray DW, Beard DJ (2006) No deterioration of kinematics and cruciate function 10 years after medial unicompartmental arthroplasty. Knee 13(6):440–444
Laurencin CT, Zelicof SB, Scott RD, Ewald FC (1991) Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res 273:151–156
Li MG, Yao F, Joss B, Ioppolo J, Nivbrant B, Wood D (2006) Mobile versus fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee 13(5):365–370
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):e1000100
Lombardi AV Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA (2009) Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res 467(6):1450–1457
Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW (2012) Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res 470(1):84–90
Manzotti A, Confalonieri N, Pullen C (2007) Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: a matched paired study. Int Orthop 31(3):315–319
Mont MA, Stuchin SA, Paley D, Sharkey PF, Parvisi J, Tria AJ Jr, Bonutti PM, Etienne G (2004) Different surgical options for monocompartmental osteoarthritis of the knee: high tibial osteotomy versus unicompartmental knee arthroplasty versus total knee arthroplasty: indications, techniques, results, and controversies. Instr Course Lect 53:265–283
Newman J, Pydisetty RV, Ackroyd C (2009) Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br 91(1):52–57. doi:10.1302/0301-620X.91B1.20899
Newman JH, Ackroyd CE, Shah NA (1998) Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br 80(5):862–865
Palmer TM, Peters JL, Sutton AJ, Moreno SG (2008) Contour-enhanced funnel plots for meta-analysis. The STATA J 8(2):242–254
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2008) Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 61(10):991–996
Sun PF, Jia YH (2012) Mobile bearing UKA compared to fixed bearing TKA: a randomized prospective study. Knee 19(2):103–106
Sweeney K, Grubisic M, Marra CA, Kendall R, Li LC, Lynd LD (2013) Comparison of HRQL between unicompartmental knee arthroplasty and total knee arthroplasty for the treatment of osteoarthritis. J Arthroplasty 28(9 Suppl):187–190
Weale AE, Murray DW, Newman JH, Ackroyd CE (1999) The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br 81(5):790–795
Wiik AV, Manning V, Strachan RK, Amis AA, Cobb JP (2013) Unicompartmental knee arthroplasty enables near normal gait at higher speeds, unlike total knee arthroplasty. J Arthroplasty 28(9 Suppl):176–178
Yang KY, Wang MC, Yeo SJ, Lo NN (2003) Minimally invasive unicondylar versus total condylar knee arthroplasty–early results of a matched-pair comparison. Singapore Med J 44(11):559–562
Zhang Q, Guo W, Zhang Q, Sun R, Liu Z, Cheng L, Xia Y, Chen G, Ding R, Zhu D, Li Z (2010) Comparison of unicompartmental knee arthroplasty and total knee arthroplasty in the treatment of unicompartmental osteoarthritis: a meta-analysis. Curr Orthop Pract 21(5):497–503
Acknowledgments
All authors declare no funding source or sponsor involvement in the study design, collection, analysis and interpretation of the data, in writing the manuscript and in submission of the manuscript for publication.
Conflict of interest
All authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arirachakaran, A., Choowit, P., Putananon, C. et al. Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol 25, 799–806 (2015). https://doi.org/10.1007/s00590-015-1610-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1610-9