Abstract
Purpose
This study compares perioperative and 1-year outcomes of lateral decubitus single position circumferential fusion (L-SPS) versus minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) for degenerative pathologies.
Methods
Multicenter retrospective chart review of patients undergoing AP fusion with L-SPS or MIS TLIF. Demographics and clinical and radiographic outcomes were compared using independent samples t tests and chi-squared analyses with significance set at p < 0.05.
Results
A total of 445 patients were included: 353 L-SPS, 92 MIS TLIF. The L-SPS cohort was significantly older with fewer diabetics and more levels fused. The L-SPS cohort had significantly shorter operative time, blood loss, radiation dosage, and length of stay compared to MIS TLIF. 1-year follow-up showed that the L-SPS cohort had higher rates of fusion (97.87% vs. 81.11%; p = 0.006) and lower rates of subsidence (6.38% vs. 38.46%; p < 0.001) compared with MIS TLIF. There were significantly fewer returns to the OR within 1 year for early mechanical failures with L-SPS (0.0% vs. 5.4%; p < 0.001). 1-year radiographic outcomes revealed that the L-SPS cohort had a greater LL (56.6 ± 12.5 vs. 51.1 ± 15.9; p = 0.004), smaller PI-LL mismatch (0.2 ± 13.0 vs. 5.5 ± 10.5; p = 0.004). There were no significant differences in amount of change in VAS scores between cohorts.
Similar results were seen after propensity-matched analysis and sub-analysis of cases including L5-S1.
Conclusions
L-SPS improves perioperative outcomes and does not compromise clinical or radiographic results at 1-year follow-up compared with MIS TLIF. There may be decreased rates of early mechanical failure with L-SPS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Single position circumferential (AP) fusion (L-SPS) has been shown to be safe and effective with shorter operative times (OpTime) and decreased estimated blood loss (EBL), length of stay (LOS), and rates of postoperative ileus compared with traditional AP fusion without other differences in complications or radiographic outcomes [1]. It is possible to achieve these improved outcomes while still maintaining the benefits of AP fusion including the ability to place large surface area grafts under the compression of the anterior column and improved biomechanical stability.
Minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) is another MIS technique without requiring repositioning. It allows a familiar, posterior approach, minimal muscle dissection and decreased OpTime, EBL, and LOS compared with open TLIF [2]. To date, L-SPS has not been directly compared to MIS TLIF. This study offers a comparison of L-SPS and MIS TLIF perioperative and 1-year outcomes.
Materials and methods
Data collection
This is a multicenter retrospective review comparing patients undergoing primary L-SPS with anterior (ALIF) or lateral lumbar interbody fusion (LLIF) with bilateral percutaneous pedicle screw placement (PPSP) to patients undergoing primary MIS TLIF with bilateral PPSP for degenerative pathologies at 5 institutions from 2013 to 2021. Patients were excluded for age younger than 18 years, previous fusion, unilateral pedicle screws, open decompression, or less than 1-year follow-up. Patient demographics, medical comorbidities, BMI, motor strength exam, procedural characteristics including numbers of levels fused, use of Bone Morphogenic Protein (BMP) or cellular bone matrix (CBM), operative time (OpTime), estimated blood loss (EBL), and radiation dosage (RadDose), and postoperative outcomes were obtained from the electronic medical record. Perioperative outcomes included post-op neurological deficits including hip flexor weakness, ileus, thromboembolic events (Pulmonary Embolus (PE)/Deep Vein Thrombosis (DVT)), surgical site infections (SSI), cardiac, or urinary complications, and returns to the operating room within 90 days. A perioperative complication was considered major if it was Grade III or higher on the Clavien-Dindo classification system [3]. 1-year outcomes included VAS scores, returns to OR for early mechanical failures (EMF), adjacent segment disease (ASD), instrumentation complications, or for neurological deficits. Radiographic analysis included preoperative, postoperative, lumbar lordosis (LL) and pelvic incidence (PI) as well as evidence of fusion or subsidence at 1 year.
Surgical technique
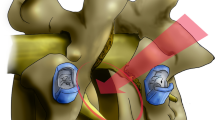
All cases were performed by experienced fellowship-trained orthopedic or neurosurgical spine surgeons. All ALIF cases utilized access surgeons. All L-SPS cases were performed according to previously published techniques [1]. The operating room was set up as depicted in Fig. 1, and patients were positioned as shown in Fig. 2. Briefly, LLIF procedures were performed using the standard lateral transpsoas approach with associated implants and instrumentation (XLIF®, NuVasive, Inc. San Diego, CA). Free-run and triggered EMG monitoring was performed during the approach to map the location of and prevent injury to the lumbar plexus during retractor placement. All ALIF procedures were carried out with a vascular access surgeon. An anterior retroperitoneal approach from the lateral decubitus position using a paramidline approach was utilized. Either a buttress plate or integrated locking screws were used to secure to the interbody cage. In all cases, cage dimensions and composition (PEEK vs. Titanium) were chosen per the senior operating surgeon’s preference.
PPSF was achieved with the patient maintained in the lateral decubitus position and using either fluoroscopic guidance or computer assisted/robot assistance. Standard technique was utilized for percutaneous pedicle screw placement. Jamshidi needles were placed using a starting point on the junction of the transverse process and lateral facet and advancing with a medialized trajectory to a depth of 25 mm with confirmation that there was no medial pedicle breach. Screw position was confirmed under fluoroscopy, and stimulation with EMG was performed to assess pedicle wall violations.
Statistical analysis
All measures were compared using independent samples t tests and chi-squared analyses as appropriate (p < 0.05.) Propensity matching (PSM) was utilized to account for demographic and procedural differences. Analysis was conducted using IBM SPSS Statistics Software (version 21.0, Armonk, NY, USA).
Results
A total of 445 patients were included, 353 undergoing L-SPS and 92 MIS TLIF. The total cohort had an average age of 61.5 ± 11.7 years, were 56.8% female and 43.2% male, and had an average BMI of 30.2 ± 5.9. 17.53% of patients were diabetic, and 8.8% had a history of smoking. The average number of levels fused was 1.4 ± 0.7, 18.4% utilized Bone Morphogenic Protein (BMP), and 53.5% used cellular bone matrix (CBM).
Analysis prior to PSM
A total of 353 patients were included in the L-SPS cohort and 92 patients were included in the MIS TLIF group. The L-SPS versus MIS TLIF cohort had an average age of 62.48 ± 11.5 vs. 57.8 ± 12.1 years, BMI of 29.9 ± 5.5 vs. 30.9 ± 7.1, were 57.5% vs. 64.1% female, 13.9% vs. 31.5% diabetic, and 7.4% vs. 14.1% smokers. Mean number of levels fused in the L-SPS cohort was 1.5 ± 0.7 and 1.2 ± 0.5 in the MIS TLIF cohort. In the L-SPS cohort, 7.9% used BMP and 61.8% used CBM, while the MIS TLIF cohort 58.7% used BMP and 21.7% used CBM. The cohorts showed significant differences in age (p = 0.001), diabetes (p = 0.001), smoking (p = 0.041), number of levels fused (p < 0.001), use of BMP (p < 0.001), and use of CBM (p < 0.001). There were no significant differences in gender or BMI (Table 1).
The L-SPS cohort had significantly shorter OpTime (97.8 ± 53.6 vs. 239.2 ± 76.9 min; p < 0.001), lower EBL (88.7 ± 165.2 vs. 214.7 ± 174.3 mL; p < 0.001), decreased RadDose (36.5 ± 35.0 vs. 59.0 ± 55.0 mGy; p = 0.001), and shorter LOS (1.9 ± 1.7 vs. 3.13 ± 2.1 days; p < 0.001) (Table 2).
Analysis of 90-day complications revealed fewer perioperative complications in the L-SPS compared to MIS TLIF group (19.0% vs. 32.6%; p = 0.005). L-SPS showed fewer minor complications (9.6% vs. 27.2%; p < 0.001), ileus (0.0% vs. 1.1%; p = 0.050), and SSI (1.4% vs. 5.4%; p = 0.021). There were no differences between the cohorts in major complications (7.7% vs. 5.4%; p = 0.464), DVT/PE (1.1% vs. 0.00%; p = 0.305), motor deficit (0.4% vs. 1.1%; p = 0.480), neuropraxia (8.2% vs. 8.7%; p = 0.882), or sensory deficits (9.6% vs. 12.0%; p = 0.510). There were no significant differences in returns to OR within 90 days for any reason (6.8% vs. 4.4%; p = 0.389), including for hematoma evacuation (0.9% vs. 1.1%; p = 0.830), irrigation and debridement (0.6% vs. 0.0%; p = 0.469), decompression (1.4% vs. 0.0%; p = 0.251), foraminal stenosis (1.4% vs. 1.1%; p = 0.807), neurological deficit (1.1% vs. 0.0%; p = 0.305), instrumentation revision (3.4% vs. 2.2%; p = 0.549), or other reason (0.9% vs. 0.0%; p = 0.375) (Table 2).
At 1 year, there were no significant differences in change in VAS scores between the 2 cohorts (− 3.1 ± 2.8 vs − 2.7 ± 3.7; p = 0.483). There were significantly fewer returns to OR within 1 year for EMF (0.0% vs. 5.4%; p < 0.001) with L-SPS. There were no other differences in overall returns to OR within 1 year for any reason (8.7% vs. 12.0%; p = 0.332) or for other reasons including returns for ASD (1.1% vs. 3.3%; p = 0.144), central (0.9% vs. 0.0%; p = 0.375) or foraminal (2.8% vs. 4.4%; p = 0.458) stenosis at the operative levels, neurological deficit (0.6% vs. 1.1%; p = 0.587), instrumentation revision (3.4% vs. 6.5%; p = 0.176), or for other reason including postoperative compressive collection or infection (1.7% vs. 2.2%; p = 0.760) (Table 3).
Radiographic analysis revealed that at 1-year follow-up, the L-SPS cohort showed higher rates of fusion compared with the MIS TLIF cohort (97.87% vs. 81.11%; p = 0.006). There were significantly higher rates of subsidence (6.38% vs. 38.46%; p < 0.001) in the MIS TLIF cohort compared to L-SPS, as illustrated in Fig. 3. There were no significant differences in baseline alignment between L-SPS and MIS TLIF cohorts including PI (56.7 ± 10.5 vs. 58.1 ± 11.3; p = 0.314), baseline LL (52.6 ± 11.3 vs. 54.0 ± 12.1; p = 0.408), and PI-LL mismatch (4.1 ± 10.1 vs. 5.4 ± 12.0; p = 0.430). 90-day radiographic outcomes revealed that the L-SPS cohort had a greater post-op LL (56.3 ± 11.18 vs. 52.0 ± 10.8; p = 0.002) and smaller post-op PI-LL mismatch (0.5 ± 9.9 vs. 5.8 ± 10.8; p < 0.001). 1-year radiographic outcomes revealed that the L-SPS cohort had a greater LL (56.6 ± 12.5 vs. 51.1 ± 15.9; p = 0.004), smaller PI-LL mismatch (0.2 ± 13.0 vs. 5.5 ± 10.5; p = 0.004). The L-SPS cohort also exhibited greater improvement in LL from baseline to 1 year (3.2 ± 8.8 vs. − 3.4 ± 13.5; p < 0.001) and in PI-LL (− 3.1 ± 10.7 vs. 1.3 ± 8.0; p = 0.006), as illustrated in Fig. 4. There were no significant differences in change in LL from post-op to 1 year − 0.2 ± 9.3 vs. − 1.6 ± 13.3; p = 0.343) or in change in PI-LL mismatch from post-op to 1 year (0.7 ± 8.6 vs. 0.1 ± 5.0; p = 0.547) (Table 4).
Example cases comparing change in alignment in two-level SPS versus MIS TLIF. Top images: Postoperative (left) compared to preoperative (right) sagittal XRs of patient undergoing two-level single position circumferential fusion (L-SPS) with anterior lumber interbody fusion with 17.3 degree increases in lumbar lordosis. Bottom Images: Postoperative (left) compared to preoperative (right) sagittal XRs of patient undergoing two-level minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) with 2.4 degree increases in lumbar lordosis
Analysis following PSM
Following PSM for age, diabetes, smoking, and number of levels fused, 184 patients remained (92 L-SPS and 92 MIS TLIF). The total cohort had an average age of 57.6 ± 12.2 years, was 59.2% female, and had an average BMI of 30.9 ± 6.5. 28.3% were diabetic and 12.0% were smokers. The average number of levels fused was 1.2 ± 0.5, 36.4% used BMP, and 36.4% used CBM. Following propensity matching there were no significant differences in demographics. There was significantly greater usage of BMP in the MIS TLIF cohort (14.1% vs. 58.7%; p < 0.001) and significantly more live cell usage in the L-SPS cohort (51.1% vs. 21.7%; p < 0.001) (Table 1). The findings after PSM continued to show shorter OpTime and decreased perioperative EBL, LOS, RadDose, and overall complication rates (Table 5). Additionally, a difference in returns to OR within 1 year for mechanical failures (0.0% vs. 5.4%; p = 0.023) was still observed. There were no significant differences in VAS scores or overall returns to OR within 1 year for any other reason (Table 6). Radiographic analysis revealed no differences in baseline alignment between the cohorts but the L-SPS had a greater post-op LL and smaller PI-LL mismatch at 90 days and at 1 year. There were no significant differences between L-SPS and MIS TLIF in change in LL or in PI-LL mismatch from post-op to 1 year (Table 7).
Sub-analysis of L5-S1 surgeries
L5-S1 surgeries were analyzed separately, which included 136 L-SPS and 41 MIS TLIF cases. The L-SPS group was older (59.0 ± 12.7 vs. 53.5 ± 12.1, p = 0.016), had more levels fused (1.7 ± 0.8 vs. 1.3 ± 0.5, p < 0.001), and lower use of BMP (8.8% vs. 68.3%, p < 0.001) than the MIS TLIF cohort. L5-S1 L-SPS showed shorter OpTime (235.9 ± 76.1 vs. 125.3 ± 53.0 min, p < 0.001), and decreased EBL (200.4 ± 160.1 vs. 136.9 ± 248.0 mL, p < 0.001), LOS (3.1 ± 2.2 vs. 2.1 ± 1.3 days, p = 0.007), rates of durotomy (0.0% vs. 4.9%; p = 0.010), and rate of minor postoperative complications (14.7% vs. 31.7%, p = 0.014) compared to the MIS TLIF cohort. The L-SPS cohort had a 4.8% rate of sensory deficit compared to 14.6% in the MIS TLIF cohort (p = 0.056) (Table 8).
There was a significantly higher fusion rate (100.0% vs. 76.9%; p < 0.001), lower subsidence rate (9.5% vs. 29.3%; 0.008), and lower EMF rate (0.0% vs. 4.9%, p = 0.010) in L-SPS patients. Improvement in LL (+ 5.0 ± 8.1 vs. − 2.5 ± 5.3; p < 0.001) and in PI-LL mismatch (− 4.5 ± 8.5 vs. + 1.2 ± 5.5; p = 0.020) at 1 year compared to baseline was greater in the L-SPS compared to MIS TLIF cohort (Table 9).
Discussion
L-SPS is a novel MIS technique for circumferential fusion with improved perioperative and 1-year outcomes compared with AP fusion with patient repositioning. Both L-SPS and MIS TLIF are muscle-sparing interbody techniques that do not require repositioning the patient. Traditionally, surgeons may opt to use MIS TLIF techniques due to OpTime, EBL, LOS, and complication profile of AP fusion [4]. However, this study found equivalent or improved perioperative outcomes with L-SPS compared to MIS TLIF. After PSM for demographic and procedural characteristics, L-SPS continued to demonstrate improved OpTime, EBL, RadDose, and LOS.
The OpTime, EBL, RadDose, and LOS demonstrated in prior MIS TLIF studies were similar [5,6,7,8,9,10]. Additionally, the current study found fewer postoperative complications in the L-SPS cohort compared to MIS TLIF. This was largely driven by minor complications, as there were no significant differences in major complications. There were also fewer sensory deficits following L-SPS compared with MIS TLIF. Numerous studies have demonstrated increased OpTime, EBL, LOS, and complications with AP fusion compared with TLIF [11,12,13,14]. A prior comparison of MIS TLIF and AP fusion showed that AP fusion was associated with a twofold higher complication rate, EBL, OpTime and LOS [11]. In a comparison of open or MIS TLIF versus ALIF utilizing the National Surgical Quality Improvement Project (NSQIP) Database, Upadhyayula et al. found that ALIF cohorts had increased pulmonary complications and hospital stays [12]. Phan et al.’s meta-analysis of TLIF versus ALIF also found that ALIF was associated with longer hospitalization with similar complication rates [15]. This first direct comparison of L-SPS with ALIF and/or LLIF versus MIS TLIF reveals that circumferential fusion can be accomplished more efficiently than MIS TLIF with less radiation and fewer complications.
Of note, MIS TLIF showed lower rates of fusion and more returns to OR for EMF at 1-year follow-up compared to L-SPS. While there is limited literature comparing EMF and pseudoarthrosis between AP fusion and MIS TLIF, the rates are comparable to those seen in prior studies. Analyses of 1- and 2-level MIS TLIFs with a minimum of 1-year follow-up have shown fusion rates of 81–92% [16,17,18]. In a prospective randomized trial, Serban et al. found a fusion rate of 90% among an MIS TLIF cohort at 1-year follow-up [19]. Studies of short segment fusion with ALIF have consistently shown rates of 93.5–100% [20, 21]. In a study of AP fusion with LLIF, Strom et al. found a fusion rate of 94% with percutaneous pedicle screw placement [22]. Therefore, the finding of higher rates of fusion among the L-SPS cohort is consistent with previous literature on MIS TLIF and traditional AP fusion. Additionally, while BMP has been associated with higher rates of fusion, the L-SPS cohort had higher rates of fusion than the MIS TLIF despite lower usage of BMP [23].
MIS TLIF was demonstrated to have significantly higher rates of subsidence when compared to L-SPS at 1 year. These rates of subsidence are similar to those previously reported in literature on MIS TLIF, ALIF, and LLIF. The Yao et al. study of 126 MIS TLIFs with 2-year follow-up found a similar rate of subsidence of 34.1% [24]. In Pisano et al.’s analysis of 89 patients with a minimum of 1-year follow-up, a subsidence rate of 50.6% [25]. In contrast to TLIF, prior studies have shown that subsidence rates in ALIF and XLIF are lower than reported rates in MIS TLIF. In a comparison of open TLIF and ALIF, cage subsidence rates at 1-year were found to be 7.7% in the ALIF cohort and 33.3% in the TLIF cohort [26]. In Rao et al.’s study of 147 patients with 18-month follow-up, the authors found a 10.2% subsidence rate. Tempel et al.’s analysis of 297 patients undergoing LLIF found a similar rate of 11.4% [27]. Therefore, it is not surprising that in the current study, L-SPS with ALIF and/or XLIF demonstrated lower rates of subsidence [26].
Furthermore, superior radiographic outcomes were observed in the L-SPS group. The postoperative LL was greater in the L-SPS cohort compared to MIS TLIF. In prior radiographic comparisons of ALIF/LLIF versus TLIF, Ahlquist et al. found that ALIF and LLIF produced greater improvements in radiographic measurements postoperatively compared with TLIF, with ALIF showing a change in LL of 5.5 degrees, LLIF of 7.7 degrees, and TLIF 2.7 degrees (p < 0.050) [28]. These results proved to be durable over time, as the change in LL from pre-op to 1 year greater in L-SPS group compared with the MIS TLIF cohort (3.73 ± 8.33 vs. − 3.41 ± 13.50; p = 0.001) and particularly notable in the L5-S1 sub-analysis which showed a change in LL to be 5.0 ± 8.1 vs. − 2.5 ± 5.3; p < 0.001. While circumferential fusion with L-SPS technique increased LL at 1 year, the MIS TLIF group experienced kyphosis. This is consistent with past literature showing that AP fusion with ALIF or LLIF serves to provide more powerful lordosis than TLIF procedures [29,30,31].
As a retrospective study, it is open to selection bias. PSM was undertaken to account for differences in demographics and procedural characteristics. Additionally, as a multicenter study, it is not possible to account for small differences in patient selection and surgical technique between institutions. However, all surgeons contributing cases are experienced, MIS surgeons, and therefore, there are unlikely to be clinically significant differences in outcomes.
The study is also limited by lack of longer-term follow-up to evaluation for pseudoarthrosis, other mechanical failures, and the differences in spinopelvic mismatch. However, it is important to recognize that there are not early failures with this novel technique. Additionally, positive 1-year clinical outcomes in lumbar spine surgery have been shown to have predictive value of longer-term outcomes [32].
Conclusion
Circumferential fusion with ALIF and/or LLIF and PPSF has clear advantages over MIS TLIF: high rates of fusion, less subsidence, and improved postoperative sagittal alignment. In the past, AP fusion required long surgeries with repositioning, high blood loss, and a unique complication profile including greater rates of postoperative ileus than in posterior fusion. This study shows that L-SPS improves operative efficiency and outcomes and low rates of complications, while still maintaining the benefits of traditional AP fusion over MIS TLIF both perioperatively and at 1 year. This makes L-SPS an attractive alternative to MIS TLIF for the treatment of degenerative pathologies.
Availability of data and material
Available.
References
Buckland AJ, Ashayeri K, Leon C, Manning J, Eisen L, Medley M, Protopsaltis TS, Thomas JA (2021) Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. Spine J 21:810–820. https://doi.org/10.1016/j.spinee.2020.11.002
Kim CH, Easley K, Lee JS, Hong JY, Virk M, Hsieh PC, Yoon ST (2020) Comparison of minimally invasive versus open transforaminal interbody lumbar fusion. Glob Spine J 10:143s–150s. https://doi.org/10.1177/2192568219882344
Klineberg EO, Passias PG, Poorman GW, Jalai CM, Atanda A, Worley N, Horn S, Sciubba DM, Hamilton DK, Burton DC, Gupta MC, Smith JS, Soroceanu A, Hart RA, Neuman B, Ames CP, Schwab FJ, Lafage V (2020) Classifying complications: assessing adult spinal deformity 2-year surgical outcomes. Glob Spine J 10:896–907. https://doi.org/10.1177/2192568220937473
Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U (2005) Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to 5 year results. Eur Spine J 14:551–558. https://doi.org/10.1007/s00586-004-0830-1
Lee MJ, Mok J, Patel P (2018) Transforaminal lumbar interbody fusion: traditional open versus minimally invasive techniques. J Am Acad Orthop Surg 26:124–131. https://doi.org/10.5435/jaaos-d-15-00756
Cheng JS, Park P, Le H, Reisner L, Chou D, Mummaneni PV (2013) Short-term and long-term outcomes of minimally invasive and open transforaminal lumbar interbody fusions: Is there a difference? Neurosurg Focus 35:E6. https://doi.org/10.3171/2013.5.Focus1377
Hey HW, Hee HT (2015) Open and minimally invasive transforaminal lumbar interbody fusion: comparison of intermediate results and complications. Asian Spine J 9:185–193. https://doi.org/10.4184/asj.2015.9.2.185
Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, McGirt MJ (2014) Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg 82:230–238. https://doi.org/10.1016/j.wneu.2013.01.041
Safaee MM, Oh T, Pekmezci M, Clark AJ (2018) Radiation exposure with hybrid image-guidance-based minimally invasive transforaminal lumbar interbody fusion. J Clin Neurosci 48:122–127. https://doi.org/10.1016/j.jocn.2017.09.026
Bindal RK, Glaze S, Ognoskie M, Tunner V, Malone R, Ghosh S (2008) Surgeon and patient radiation exposure in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine 9:570–573. https://doi.org/10.3171/spi.2008.4.08182
Villavicencio AT, Burneikiene S, Bulsara KR, Thramann JJ (2006) Perioperative complications in transforaminal lumbar interbody fusion versus anterior-posterior reconstruction for lumbar disc degeneration and instability. J Spinal Disord Tech 19:92–97. https://doi.org/10.1097/01.bsd.0000185277.14484.4e
Upadhyayula PS, Curtis EI, Yue JK, Sidhu N, Ciacci JD (2018) Anterior versus transforaminal lumbar interbody fusion: perioperative risk factors and 30-day outcomes. Int J Spine Surg 12:533–542. https://doi.org/10.14444/5065
Phan K, Xu J, Scherman DB, Rao PJ, Mobbs RJ (2017) Anterior Lumbar Interbody fusion with and without an “access surgeon”: a systematic review and meta-analysis. Spine 42:E592-e601. https://doi.org/10.1097/brs.0000000000001905 (Phila Pa 1976)
Hee HT, Castro FP Jr, Majd ME, Holt RT, Myers L (2001) Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord 14:533–540. https://doi.org/10.1097/00002517-200112000-00013
Phan K, Thayaparan GK, Mobbs RJ (2015) Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion–systematic review and meta-analysis. Br J Neurosurg 29:705–711. https://doi.org/10.3109/02688697.2015.1036838
Kaye ID, Fang T, Wagner SC, Butler JS, Sebastian A, Morrissey PB, Levine MJ, Vaccaro AR, Hilibrand AS (2020) A comparison of revision rates and patient-reported outcomes for a 2-level posterolateral fusion augmented with single versus 2-level transforaminal lumbar interbody Fusion. Glob Spine J 10:958–963. https://doi.org/10.1177/2192568219889360
Lin GX, Sharma S, Rui G, Song MS, Kim JS (2020) Minimally invasive transforaminal lumbar interbody fusion with intraoperative fluoroscopy for disc space preparation: analysis of fusion rate and clinical results. Oper Neurosurg 19:557–566. https://doi.org/10.1093/ons/opaa178 (Hagerstown)
Emami A, Faloon M, Sahai N, Dunn CJ, Issa K, Thibaudeau D, Sinha K, Hwang KS (2018) Risk factors for pseudarthrosis in minimally-invasive transforaminal lumbar interbody fusion. Asian Spine J 12:830–838. https://doi.org/10.31616/asj.2018.12.5.830
Serban D, Calina N, Tender G (2017) Standard versus minimally invasive transforaminal lumbar interbody fusion: a prospective randomized study. Biomed Res Int 2017:7236970. https://doi.org/10.1155/2017/7236970
Kleimeyer JP, Cheng I, Alamin TF, Hu SS, Cha T, Yanamadala V, Wood KB (2018) Selective anterior lumbar interbody fusion for low back pain associated with degenerative disc disease versus nonsurgical management. Spine 43:1372–1380. https://doi.org/10.1097/brs.0000000000002630 (Phila Pa 1976)
Rao PJ, Loganathan A, Yeung V, Mobbs RJ (2015) Outcomes of anterior lumbar interbody fusion surgery based on indication: a prospective study. Neurosurgery 76:7–24. https://doi.org/10.1227/neu.0000000000000561
Strom RG, Bae J, Mizutani J, Valone F 3rd, Ames CP, Deviren V (2016) Lateral interbody fusion combined with open posterior surgery for adult spinal deformity. J Neurosurg Spine 25:697–705. https://doi.org/10.3171/2016.4.Spine16157
Dawson E, Bae HW, Burkus JK, Stambough JL, Glassman SD (2009) Recombinant human bone morphogenetic protein-2 on an absorbable collagen sponge with an osteoconductive bulking agent in posterolateral arthrodesis with instrumentation. a prospective randomized trial. J Bone Joint Surg Am 91:1604–1613. https://doi.org/10.2106/jbjs.G.01157
Yao YC, Chou PH, Lin HH, Wang ST, Liu CL, Chang MC (2020) Risk factors of cage subsidence in patients received minimally invasive transforaminal lumbar interbody fusion. Spine 45:E1279-e1285. https://doi.org/10.1097/brs.0000000000003557 (Phila Pa 1976)
Pisano AJ, Fredericks DR, Steelman T, Riccio C, Helgeson MD, Wagner SC (2020) Lumbar disc height and vertebral Hounsfield units: association with interbody cage subsidence. Neurosurg Focus 49:E9. https://doi.org/10.3171/2020.4.Focus20286
Lee N, Kim KN, Yi S, Ha Y, Shin DA, Yoon DH, Kim KS (2017) Comparison of outcomes of anterior, posterior, and transforaminal lumbar interbody fusion surgery at a single lumbar level with degenerative spinal disease. World Neurosurg 101:216–226. https://doi.org/10.1016/j.wneu.2017.01.114
Tempel ZJ, McDowell MM, Panczykowski DM, Gandhoke GS, Hamilton DK, Okonkwo DO, Kanter AS (2018) Graft subsidence as a predictor of revision surgery following stand-alone lateral lumbar interbody fusion. J Neurosurg Spine 28:50–56. https://doi.org/10.3171/2017.5.Spine16427
Ahlquist S, Park HY, Gatto J, Shamie AN, Park DY (2018) Does approach matter? A comparative radiographic analysis of spinopelvic parameters in single-level lumbar fusion. Spine J 18:1999–2008. https://doi.org/10.1016/j.spinee.2018.03.014
Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7:379–386. https://doi.org/10.3171/spi-07/10/379
Kim JS, Kang BU, Lee SH, Jung B, Choi YG, Jeon SH, Lee HY (2009) Mini-transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion augmented by percutaneous pedicle screw fixation: a comparison of surgical outcomes in adult low-grade isthmic spondylolisthesis. J Spinal Disord Tech 22:114–121. https://doi.org/10.1097/BSD.0b013e318169bff5
Sembrano JN, Yson SC, Horazdovsky RD, Santos ER, Polly DW Jr (2015) Radiographic comparison of lateral lumbar interbody fusion versus traditional fusion approaches: analysis of sagittal contour change. Int J Spine Surg 9:16. https://doi.org/10.14444/2016
Adogwa O, Buchowski JM, Lenke LG, Shlykov MA, El Dafrawy M, Lertudomphonwanit T, Obey MR, Koscso J, Gupta MC, Bridwell KH (2019) Comparison of rod fracture rates in long spinal deformity constructs after transforaminal versus anterior lumbar interbody fusions: a single-institution analysis. J Neurosurg Spine 32(1):42–49. https://doi.org/10.3171/2019.7.Spine19630
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
J. Alex Thomas is a consultant for Nuvasive. Brett Braly is a consultant for Stryker and Nuvasive. Ivan Cheng is a consultant for Nuvasive and Globus Medical. Brian Kwon is a consultant for Nuvasive. Themistocles S. Protopsaltis is a consultant for Altus Partners, Globus Medical, Nuvasive, and Zimmer Biomet. Aaron J. Buckland is a consultant for Nuvasive, Biedermann Motech, Medtronic, Evolution Spine, Altus Partners, and Zimmer Biomet.
Ethical approval
IRB exempt.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ashayeri, K., Alex Thomas, J., Braly, B. et al. Lateral decubitus single position anterior–posterior (AP) fusion shows equivalent results to minimally invasive transforaminal lumbar interbody fusion at one-year follow-up. Eur Spine J 31, 2227–2238 (2022). https://doi.org/10.1007/s00586-022-07226-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07226-7