Abstract
Purpose
This study systematically analyzed and assessed the interrelationships among vertebral anomaly location, congenital scoliosis (CS) type and associated abnormality prevalence.
Methods
We retrospectively extracted medical records of 1289 CS inpatients surgically treated in our institute from January 2010–December 2019. All patients underwent spinal X-ray, CT, MRI, echocardiogram, urogenital ultrasound and systemic physical examination. We analyzed information on demographics, CS type, associated anomalies and vertebral anomaly location.
Results
Cervical, thoracic and lumbar vertebral anomalies were found in 5.7%, 78.1% and 33.6% of patients, respectively. 82.7% had one region involved. 59.5% with cervical malformations had mixed defects and 61.1% with lumbar malformations exhibited failure of formation. The musculoskeletal defect prevalence was 28.4%, 19.1% and 9.0% in patients with cervical, thoracic and lumbar anomalies. The intraspinal defect prevalence was 33.4% and 20.7% for thoracic and lumbar anomalies. 86.5% of patients with cervical anomalies had more than one region involved, while 78.1% and 62.2% with thoracic and lumbar anomalies, respectively, had only one region involved.
Conclusions
Cervical malformations had higher prevalence of mixed defects, musculoskeletal and intraspinal defects and multi-region involved. Thoracic malformations had higher prevalence of intraspinal and musculoskeletal defects and more involvement of only one vertebral region. Lumbar vertebral malformation patients had much lower prevalence of intraspinal and musculoskeletal defects and more involvement of only one vertebral region. Cervical malformation was a risk factor for more associated anomalies and more severe vertebral anomalies, which deserves more attention from surgeons in outpatient clinic.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital scoliosis (CS), previously usually referred to as congenital vertebral anomaly (CVA), is the 3D curvature of the spine resulting from vertebral deformities like failure of vertebral formation, segmentation, or mixed ones that develop between 4 and 6 weeks of gestation. CS was reported to occur in approximately 1 in every 1000 live births [1]. Congenital scoliosis is caused by abnormal vertebral development, and a multifactorial etiology of CS is universally accepted [2,3,4]. However, the specific etiology of most CS cases remains unclear.
It is widely observed in clinical practice that CS patients usually have other comorbid congenital abnormalities. Among all kinds of congenital defects, intraspinal, cardiovascular and genitourinary defects are the most common. Several previous studies have reported the prevalence of different congenital defects in CS patients [5,6,7,8,9,10,11,12,13,14,15,16]. However, very few studies have revealed the interrelationship between vertebral anomaly location and prevalence of associated anomalies, and contradictory findings have been suggested in different cohorts with no more than 300 CS patients.
Thus, this study retrospectively analyzed 1289 surgical CS patients in a single center and aimed to systemically analyze and assess the interrelationships among vertebral anomaly location, CS type and prevalence of associated abnormalities.
Materials and methods
We retrospectively searched the inpatient database using ICD-10 codes (Q67.501, Q67.502) for patients who were admitted for CS from January 2010 to December 2019 in our institute. In total, we consecutively included 1289 CS inpatients in our study.
The CS types, namely failure of formation (FF), failure of segmentation (FS) and mixed defects (MD), and vertebral anomaly location were diagnosed from the patients’ X-ray and spine CT [17, 18]. The vertebral anomaly location was classified as cervical (C1 to C7/T1 disc), thoracic (T1 to T12/L1 disc) or lumbar (L1 to L5/S1 disc). Echocardiogram, urogenital ultrasound, spine imaging including spine MRI, X-ray and CT and systemic physical examination were performed for all inpatients to screen and diagnose associated anomalies.
After automated extraction of patient information from the inpatient database, all patients’ medical records, including imaging reports, were reviewed and reevaluated case by case to minimize missing data.
Statistical analysis
Descriptive statistics are expressed as the mean ± standard deviation for continuous variables and percentage (%) for categorical variables. The chi-square test was used to evaluate the relationships between categorical variables. p value < 0.05 was considered to indicate a statistically significant result. Statistical analysis was performed using IBM SPSS Statistics 23 (SPSS Inc., Beijing, China). Statistical graphs were plotted using GraphPad Prism 7.
Results
In total, 1289 CS patients were included in our study. The mean patient age was 12.4 ± 8.1 years old, and 54.0% were female (Table 1). Among all 1289 CS patients, FF was seen in 633 patients (49.1%), FS in 251 patients (19.5%), and MD in 405 patients (31.4%) (Table 1). Regarding vertebral anomaly location, cervical, thoracic and lumbar vertebral anomalies were found in 74 patients (5.7%), 1008 patients (78.1%) and 434 patients (33.6%), respectively. Most patients (n = 1067, 82.7%) had only one region involved (C, T or L), whereas only 5 patients (0.4%) had all three regions involved (Table 1). Typical X-rays and spine CT 3D-reconstructions of three CS types and different vertebral anomaly regions were shown in Fig. 1.
Typical X-ray and CT 3D-reconstruction of three CS types. a X-ray and CT 3D-reconstruction of a patient with failure of formation (a hemivertebrae between L2 and L3), b X-ray and CT 3D-reconstruction of a patient with failure of segmentation (T6 to T8 segmentation defect), c X-ray and CT 3D-reconstruction of a patient with mixed defects (a hemivertebrae between L4 and L5, T8 to T11 segmentation defects)
The prevalence of cervical, thoracic and lumbar malformations was compared according to sex in Table 2. The prevalence of cervical and lumbar malformations was higher in male patients, while the prevalence of thoracic malformation was higher in female patients. However, none of the differences was statistically significant.
In the analysis of the interrelationship between CS type and malformation location, we found that in patients with cervical malformation, the prevalence of mixed defects was significantly higher than that in the total population, while the prevalence of failure of formation and failure of segmentation was lower (59.5% vs 31.4% for MD, 27.0% vs. 49.1% for FF, 13.5% vs 19.5% for FS, p < 0.001). Patients with thoracic malformations were found to have lower prevalence of FF, and higher prevalence of FS and MD (41.7% vs 49.1% for FF, 22.4% vs 19.5% for FS, 35.9% vs. 31.4% for MD, p < 0.001). However, in patients with lumbar malformations, most patients were found to have FF (61.1% vs. 49.1% for FF, 12.7% vs. 19.5 for FS, 26.3% vs. 31.4% for MD, p < 0.001) (Table 3).
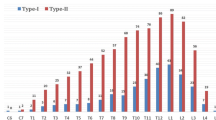
Regarding the interrelationship between different associated anomalies and vertebral malformation locations, we found that cardiac, urogenital and gastrointestinal defects were not related to any of the three spinal regions. However, musculoskeletal defects, including rib deformities, absent rib, fused rib, polydactyly, syndactyly, foot deformities and developmental dysplasia of hip, exhibited significantly higher prevalence in patients with cervical (28.4% vs 15.6%, p = 0.005) (Fig. 2a) and thoracic malformations (19.1% vs 6.4%, p < 0.001) (Fig. 2b), but lower prevalence in patients with lumbar malformations (9.0% vs. 20.1%, p < 0.001) (Fig. 2c). Similarly, intraspinal defects exhibited significantly higher prevalence in patients with thoracic malformations (33.4% vs. 14.9%, p < 0.001) (Fig. 2b) and significantly lower prevalence in patients with lumbar malformations (20.7% vs. 33.8%, p < 0.001) (Fig. 2c).
Interrelationship between different associated anomalies and vertebral malformation location. a Interrelationship between different associated anomalies and cervical malformation, b Interrelationship between different associated anomalies and thoracic malformation, c Interrelationship between different associated anomalies and lumbar malformation, *p < 0.05; **p < 0.01; ***p < 0.001
As intraspinal defects were greatly interrelated with thoracic and lumbar malformations, we further analyzed interrelationship between specific intraspinal defects, namely diastematomyelia, syringomyelia and tethered cord, and malformation location. We found that in patients with thoracic malformations, all three intraspinal defects had significantly higher prevalence (23.2% vs. 5.3% for diastematomyelia, 15.2% vs. 6.0% for syringomyelia and 10.5% vs. 3.9% for tethered cord, p < 0.001) than in patients without thoracic malformations (Fig. 3a). However, in patients with lumbar malformations, the prevalence was significantly lower (20.7% vs. 33.8% for diastematomyelia and 11.5% vs. 23.3% for syringomyelia, p < 0.001) than in patients without lumbar malformations (Fig. 3b).
Interrelationship between specific intraspinal anomalies and vertebral malformation location. a Interrelationship between different associated anomalies and thoracic vertebral malformation, b Interrelationship between different associated anomalies and lumbar vertebral malformation, *p < 0.05; **p < 0.01; ***p < 0.001
After analyzing the interrelationship between involved region number and vertebral malformation location, we also found that 86.5% of patients with cervical malformations had more than one region involved (p < 0.001), whereas most patients with thoracic (78.1%, p < 0.001) and lumbar malformations (62.2%, p < 0.001) had only one region involved (Table 4). A recommended diagnostic algorithm was summarized in Fig. 4.
Discussion
Very few independent studies covering different ethnic populations analyzing vertebral anomaly locations in CS patients have been published. However, most of these studies did not analyze the interrelationships among vertebral anomaly location, all common associated anomalies and types of CS. Therefore, we conducted this study to systemically analyze and fully describe the distribution of vertebral anomaly locations and the interrelationships among location, associated anomalies and CS type. To the best of our knowledge, this is the largest CS series and the first systemic analysis of all common associated anomalies and all CS types so far. In our study, a total of 1289 CS patients were included and all their medical records, including imaging examination reports, were reviewed and reevaluated.
In the study of Eliane et al. [13], cervical, thoracic and lumbar malformations were found in 18.9%, 67.8% and 38.8% of patients, respectively. In our CS cohort, a large percentage of patients were found to have thoracic and lumbar malformations, but very few patients presented with cervical malformations. This result is similar to previous findings, although the prevalence of cervical malformation in a previous study was much higher. This finding indicates that thoracic vertebrae are the most commonly affected, while cervical vertebrae are the least commonly affected in the natural CS population. 17.2% of patients in our cohort had anomalies affecting multiple spinal regions; this value is slightly lower than the 29.7% identified in the study of Eliane et al. [13].
Regarding the analysis of malformation location and sex, we found no statistically significant differences according to sex, although males had slightly higher prevalence of cervical and lumbar malformation, while females had slightly higher prevalence of thoracic malformation. This result is similar to the findings in the study of Ghandhari et al. [10], but the correlation was more significant in their study. This difference might result from the much larger patient population in our study (1289 vs. 202) or the different ethnicities included (Chinese vs Caucasian).
In this study, we first analyzed the interrelationship between CS type and vertebral malformation location. In short, we found that patients with cervical malformations had significantly higher prevalence of MD, whereas patients with lumbar malformations had significantly higher prevalence of FF. This result is in accordance with our experience in clinical practice. Most patients with cervical defects treated in our hospital had quite complex anomalies, whereas most patients with lumbar defects had only simple hemivertebrae. During embryonic development, the paraxial mesoderm develops into 42 pairs of somites, and each somite then differentiates into a dermomyotome and a sclerotome which further become the skeleton of the vertebral column in a craniocaudal direction [19]. Therefore, cervical vertebrae develop earlier than lumbar vertebrae. In addition, in the early stage of development, embryos are more vulnerable to teratogenic factors. Thus, abnormalities in cervical vertebral development might affect the development of subsequent vertebrae and other systems, leading to complex defects and MD in patients with cervical defects.
Regarding associated anomalies, some previous studies suggested an association between spine level and concomitant anomalies, while other studies did not. Several previous studies have revealed that cardiac, gastrointestinal and urogenital defects are not correlated with the location of vertebral anomalies [5, 6]. However, Bollini et al. [20] found that there was higher prevalence of cardiac defects in patients with thoracic malformations but urogenital defects are not associated with the location of vertebral anomalies. However, all the sample sizes of these studies were small, and the largest study included no more than 300 cases. In our cohort, we analyzed a much larger cohort of 1289 CS patients and found that gastrointestinal and urogenital defects showed no interrelationship with vertebral anomaly levels. Cardiac defects were slightly more frequent in patients with thoracic malformations, but the difference was not significant (p = 0.054).
Ghandhari et al. [10] showed that patients with rib defects had higher prevalence of thoracic malformation and lower prevalence of lumbar malformation. In this study, musculoskeletal defects were found in 16.4% of the total population. Patients with cervical and thoracic malformations had significantly higher prevalence of musculoskeletal anomalies, while patients with lumbar malformations had lower prevalence. As most musculoskeletal defects in our cohort were rib defects, this finding is consistent with the result of the study of Ghandhari et al. Based on our clinical practice, CS individuals with rib defects tend to have more severe and progressive curves as rib defects lead to additional forces that accelerate the promotion of spinal deformities.
In the analysis of intraspinal defects, Beals et al. [5] showed that hemivertebrae located higher up in the spine (cervical or thoracic) had a higher risk of intraspinal abnormalities. Similarly, Basu et al. [6] revealed that in patients with lumbar hemivertebrae, only 20% of patients had abnormal spinal MRI findings; this percentage is significantly lower than the prevalence of intraspinal defects. They also found that intraspinal defects were more frequent in patients with cervical and thoracic malformations. However, Bollini et al. [20] found that intraspinal defects are more common in patients with lumbosacral anomalies and less common in patients with thoracic anomalies. In our CS series, we also found that the prevalence of intraspinal defects was higher in patients with cervical and thoracic malformations but lower in patients with lumbar malformations. After further analyzing specific intraspinal defects, we found higher prevalence of diastematomyelia, syringomyelia and tethered cord in patients with thoracic malformations and lower prevalence in patients with lumbar malformations. As the spinal cord ends at approximately the L1 level 2 months after birth, we assumed that vertebral defects at the cervical and thoracic regions might affect the normal development of the spinal cord. However, this concept still needs further clarification.
Finally, by analyzing the interrelation between vertebral anomaly location and the number of involved regions, we found that in patients with cervical malformations, 86.5% had more than one region involved, while in patients with thoracic and lumbar malformations, the majority had only one region affected.
Generally, we found that patients with cervical vertebral malformations were more severe and complex. For example, Fig. 5 showed a typical patient with cervical vertebral malformation. The patient has mixed defects of vertebral malformations located in cervical and upper thoracic spine. CT 3D-reconstruction also showed fused ribs and spinal MRI showed syringomyelia. This case demonstrated our results that patients with cervical malformations had higher prevalence of mixed defects, musculoskeletal and intraspinal defects and multi-region involved.
A typical patient with cervical vertebral malformation. a Spine antero-posterior and lateral X-ray showed that the patient had severe mixed defects of vertebral malformations located in cervical and upper thoracic region, b left and right bending X-ray showed that the scoliosis had poor flexibility, c CT 3D-reconstruction showed that the patient had C6 to T2 and T4 to T5 segmentation defects, T1, T3, T6 hemivertebrae, T5 butterfly vertebra, right 1 to 2 and 3 to 6 ribs fused, d sagittal plane of Spine MRI showed longitudinal low T1 and high T2 signal indicating that the patient had syringomyelia, e cross-sectional plane of Spine MRI showed circular high T2 signal in spinal cord indicating syringomyelia
The results found in our study have significant instructions for surgeons, especially in the outpatient clinic. In the setting of outpatient clinic, only spinal imaging, instead of multi-system examinations, will be prescribed by surgeons in most time in our institute. In addition, from the perspective of economic burden, it is helpful for both patients and the government that only CS patients with risk factors of more comorbidities and associated anomalies, which were defined as cervical and thoracic vertebral deformities in this study, are prescribed with thorough examinations. Based on our findings, we recommended that patients with risk factors for more associated intraspinal defects should be prescribed with spinal MRI in the setting of outpatient clinic.
In summary, our study has two major strengths. First, to our knowledge, CS series in previous studies included no more than 300 patients, thus this is one of the largest CS cohorts. Second, we are the first to comprehensively analyze the interrelationships among sex, CS type, all common associated anomalies and vertebral malformation location in a single CS cohort. However, as this is a retrospective study of extracted medical records, the quality and reliability of this study were largely influenced by the recorders, imaging interpreters and medical record quality.
Conclusions
As described above, our study revealed that cardiac, urogenital and gastrointestinal defects were not correlated with vertebral anomaly location. We also found that patients with cervical vertebral malformations had higher prevalence of MD, musculoskeletal and intraspinal defects, and involvement of more than one region. Thoracic vertebral malformation patients had higher prevalence of intraspinal and musculoskeletal defects and more involvement of only one vertebral region. Patients with lumbar vertebral malformations had much higher prevalence of FF and lower prevalence of intraspinal and musculoskeletal defects. This finding is consistent with our clinical experience that patients with cervical anomalies had more associated anomalies and more complex vertebral abnormalities, while patients with lumbar anomalies usually had simple hemivertebrae with less associated anomalies. Thus, we suggest that cervical malformation could be considered as a risk factor for more associated anomalies and more severe vertebral anomalies in CS patients, which deserves more attention from surgeons in the setting of outpatient clinic. Based on such findings, we have originally proposed a recommended diagnostic algorithm in Fig. 4 for developing regions to help reduce economic burden and examination accessibility.
IRB Approval Statement: This study has been approved from the Institutional Review Board.
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Giampietro PF, Blank RD, Raggio CL, Merchant S, Jacobsen FS, Faciszewski T, Shukla SK, Greenlee AR, Reynolds C, Schowalter DB (2003) Congenital and idiopathic scoliosis: clinical and genetic aspects. Clin Med Res 1(2):125–136. https://doi.org/10.3121/cmr.1.2.125
Batra S, Ahuja S (2008) Congenital scoliosis: management and future directions. Acta Orthop Belg 74(2):147–160
Giampietro PF, Raggio CL, Blank RD, McCarty C, Broeckel U, Pickart MA (2013) Clinical, genetic and environmental factors associated with congenital vertebral malformations. Mol Syndromol 4(1–2):94–105. https://doi.org/10.1159/000345329
Li Z, Yu X, Shen J (2015) Environmental aspects of congenital scoliosis. Environ Sci Pollut Res Int 22(8):5751–5755. https://doi.org/10.1007/s11356-015-4144-0
Beals RK, Robbins JR, Rolfe B (1993) Anomalies associated with vertebral malformations. Spine (Phila Pa 1976) 18(10):1329–1332. https://doi.org/10.1097/00007632-199308000-00012
Basu PS, Elsebaie H, Noordeen MH (2002) Congenital spinal deformity: a comprehensive assessment at presentation. Spine (Phila Pa 1976) 27(20):2255–2259. https://doi.org/10.1097/00007632-200210150-00014
Rai AS, Taylor TK, Smith GH, Cumming RG, Plunkett-Cole M (2002) Congenital abnormalities of the urogenital tract in association with congenital vertebral malformations. J Bone Joint Surg Br 84(6):891–895. https://doi.org/10.1302/0301-620x.84b6.11814
Liu YT, Guo LL, Tian Z, Zhu WL, Yu B, Zhang SY, Qiu GX (2011) A retrospective study of congenital scoliosis and associated cardiac and intraspinal abnormities in a Chinese population. Eur Spine J 20(12):2111–2114. https://doi.org/10.1007/s00586-011-1818-2
Shen J, Wang Z, Liu J, Xue X, Qiu G (2013) Abnormalities associated with congenital scoliosis: a retrospective study of 226 Chinese surgical cases. Spine (Phila Pa 1976) 38(10):814–818. https://doi.org/10.1097/BRS.0b013e31827ed125
Ghandhari H, Tari HV, Ameri E, Safari MB, Fouladi DF (2015) Vertebral, rib, and intraspinal anomalies in congenital scoliosis: a study on 202 Caucasians. Eur Spine J 24(7):1510–1521. https://doi.org/10.1007/s00586-015-3833-1
Bozcali E, Ucpunar H, Sevencan A, Balioglu MB, Albayrak A, Polat V (2016) A retrospective study of congenital cardiac abnormality associated with scoliosis. Asian Spine J 10(2):226–230. https://doi.org/10.4184/asj.2016.10.2.226
Gupta N, S R, G B, Shetty A, (2016) Vertebral and intraspinal anomalies in Indian population with congenital scoliosis: a study of 119 consecutive patients. Asian Spine J 10(2):276–281. https://doi.org/10.4184/asj.2016.10.2.276
Beauregard-Lacroix E, Tardif J, Camurri MV, Lemyre E, Barchi S, Parent S, Campeau PM (2017) Retrospective analysis of congenital scoliosis: associated anomalies and genetic diagnoses. Spine (Phila Pa 1976) 42(14):E841–E847. https://doi.org/10.1097/BRS.0000000000001983
Sevencan A, Misir A, Ucpunar H, Balioglu MB, Gur V, Akinci S (2019) The prevalence and interrelationship of concomitant anomalies in congenital scoliosis. Turk Neurosurg 29(3):404–408. https://doi.org/10.5137/1019-5149.JTN.24429-18.2
Mohanty SP, Pai Kanhangad M, Narayana Kurup JK, Saiffudeen S (2020) Vertebral, intraspinal and other organ anomalies in congenital scoliosis. Eur Spine J 29(10):2449–2456. https://doi.org/10.1007/s00586-020-06450-3
MacEwen GD, Winter RB, Hardy JH (1972) Evaluation of kidney anomalies in congenital scoliosis. J Bone Joint Surg Am 54(7):1451–1454
McMaster MJOK (1982) The natural history of congenital scoliosis. A study of two hundred and fifty-one patients. J Bone Joint Surg Am 64(8):1128–1147
Winter RBMJ, Wang JF (1973) Congenital kyphosis. Its natural history and treatment as observed in a study of one hundred and thirty patients. J Bone Joint Surg Am 55(2):223–256
Kaplan KM, Spivak JM, Bendo JA (2005) Embryology of the spine and associated congenital abnormalities. Spine J 5(5):564–576. https://doi.org/10.1016/j.spinee.2004.10.044
Bollini G, Launay F, Docquier PL, Viehweger E, Jouve JL (2010) Congenital abnormalities associated with hemivertebrae in relation to hemivertebrae location. J Pediatr Orthop B 19(1):90–94. https://doi.org/10.1097/BPB.0b013e3283327f57
Funding
The study was supported by grants from National Natural Science Foundation of China (Nos. 81972037, 81902178), National Key Research & Development Program of China (No. 2017YFC1104902), Beijing Natural Science Foundation (No. L192015), Fundamental Research Funds for the Central Universities (No. 3332019021), China Postdoctoral Science Foundation (No. 2020M670008ZX).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no conflict of interest statement.
Ethics approval
This study has been approved from the Institutional Review Board.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lin, G., Chai, X., Wang, S. et al. Cross-sectional analysis of associated anomalies and vertebral anomaly location in 1289 surgical congenital scoliosis. Eur Spine J 30, 3577–3584 (2021). https://doi.org/10.1007/s00586-021-06898-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06898-x