Abstract
Purpose
To investigate the anatomical and biomechanical feasibility of the unilateral C1 double screw [pedicle screw (PS) + lateral mass screw (LMS)] and ipsilateral C2 PS combined with contralateral C2 laminar screw (LS)-rod fixation for atlantoaxial instability by comparison with traditional posterior fixation methods.
Methods
Fifteen sets of complete dry bony specimens of atlas were used for morphometric analysis. The working length, width and thickness of the C1 PSs and LMSs were manually measured. Ten fresh-frozen cervical spines (C0–C7) were used to complete the range of motion (ROM) testing in their intact condition, under destabilization and after stabilization by the following procedures: unilateral C1–C2 PS rod fixation (Group A), bilateral C1–C2 PS rod fixation (Group B), and unilateral C1 double screw and ipsilateral C2 PS combined with contralateral C2 LS rod fixation (Group C).
Results
The working thickness of the C1 PS was ≤ 3.5 mm in only one (1/15 = 6.7%) specimen. The other parameters were > 3.5 mm in all specimens. In the ROM test, all fixation groups showed significantly reduced flexibility in all directions compared with both the intact and destabilization groups. Further, Groups B and C showed better stability in all directions than Group A. However, no significant differences were observed between Groups B and C.
Conclusion
The C1 unilateral lateral mass could mostly contain two screws(PS + LMS) with diameters ≤ 3.5 mm. The novel technique of unilateral C1 double screw and ipsilateral C2 PS combined with contralateral C2 LS rod fixation provided better stability than unilateral PS rod fixation and similar as bilateral PS rod fixation. Therefore, it is a feasible salvage method that provides a new insight into atlantoaxial instability.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, the C1–C2 pedicle screws (PSs) or lateral mass screws (LMSs) with additional rods have been widely used as a surgical technique for stabilizing atlantoaxial instability. Goel and Laheri [1] initially introduced the technique of C1 LMS and C2 PS fixation, which was then popularized by Harms and Melcher [2]. Resnick et al. [3] modified the technique by placing the screw through the posterior arch into the lateral mass without penetrating the anterior cortex to overcome the deficiencies of the Harms technique, which is now most commonly referred to as the C1 PS technique. These two techniques of C1 placement have been proven to result in excellent biomechanical properties and have been widely clinically applied [4,5,6,7]. However, they still carry potential risks of injuring the surrounding neurovascular tissue, especially vertebral artery injury (VAI). Furthermore, in the inevitable situation of VAI or in the case of unfavorable bone structures, C1 LMS–C2 PS fixation cannot be performed using the bilateral method [8]. Then, unilateral fixation is generally acceptable, but the patient requires an external orthosis until fusion or bone union is achieved [9]. Therefore, a secure and feasible salvage fixation method with satisfactory biomechanical stability is needed.
Materials and methods
Anatomical measurements
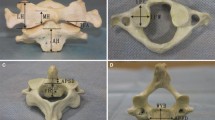
This study was approved by the medical ethics committee. Fifteen sets of complete dry bony specimens of adult atlas vertebrae were used for morphometric measurement using electronic vernier calipers (precision 0.01 mm, YATO, Tokyo, Japan). According to the previous reports of C1 screw insertion techniques, we proposed our modified strategy of the ideal screw path, entry point and end point via simulating the placement of two screws in the unilateral C1 lateral mass with Mimics software 17.0 (Materialise, Leuven, Belgium) (Fig. 1).
For the C1 PS, we took the medial third of the posterior arch at the midpoint of the thinnest part of the VA groove as the screw entry point (A) [10]. The PS was placed through the posterior arch aiming at the medial and superior thirds of the lateral mass (B) with an approximately cephalad angulation of 10° and a medial angulation of 5°, without penetrating the superior rim of the posterior arch.
For the C1 LMS, we chose the point approximately 1 mm lateral and inferior to the midpoint of the posterior surface of the lateral mass, below the dorsal arch, as the screw entry point (C). The LMS directly entered the lateral mass aiming at the junction of the anterior arch and lateral mass (D) with a cephalad angulation of approximately 10°–15° and a medial angulation of 20°.
Then, the working length, width and thickness of the C1 PS and LMS were manually measured on two sides. All measurements were taken twice, and the mean was calculated. The measured parameters were listed below (Fig. 2):
-
1.
PS working length (L1) AB.
-
2.
PS working width (W1) Minimum distance from the medial intersection of the posterior arch and lateral mass (E) to the medial rim of the VA foramen (F).
-
3.
PS working thickness (T1) Thickness of the thinnest part of the VA groove.
-
4.
LMS working length (L2) CD.
-
5.
LMS working width (W2) The width at entry point C in the horizontal direction.
-
6.
LMS working thickness (T2) The height between the intersection of the posterior arch and inferior articular process within a vertical line crossing point C.
Specimens
Ten fresh-frozen cadaveric cervical spines (C0 [basilar part of occipital bone]–C7) were verified via computed tomography (CT) to exclude bony abnormalities. All qualified specimens were individually preserved with double-bagged and frozen at − 20 °C. Before testing, the specimens were thawed at 4 °C for at least 12 h and carefully stripped of surrounding soft tissues while the intervertebral disks, ligaments and joint capsules were completely preserved. To keep the specimens moist, saline was sprayed throughout the entire experimental process. The C0 and C7 vertebrae were then embedded as fixed parts with polymethylmethacrylate bone cement.
Surgical techniques
For C1 PS and LMS placement, we utilized the screw placement strategy described above. The C1 LMS was inserted bicortically, and the C1 PS was inserted unicortically. For C2 PS placement, the entry point was in the cranial and medial quadrant of the C2 lateral mass surface. Screws were inserted unicortically, 20° to 30° in a medial and cephalad direction, guided by the superior and medial surface of the C2 isthmus [6]. For C2 LS placement, the entry point was identified at the junction point of spinous process and lamina, and the screw was then placed along the long axis of lamina [11]. After all the screws were inserted, the C1–C2 PSs were connected by a 3-mm-diameter rod. Meanwhile, the C1 LMS and C2 LS were connected by a rod crossing with the former. All screws were 3.6-mm-diameter multiaxial screws provided by the Medtronic-Kanghui medical company. The length of the screws was chosen such that unicortical screws were just short of the anterior cortex of C1 and bicortical screws penetrated the anterior cortex by two screw threads.
Flexibility test
The flexibility test was performed by measuring the range of motion (ROM) in all directions. The ROM was determined with the MTS 858 Mini Bionix II test system (MTS Systems Corp., Eden Prairie, Minnesota). A testing system consisting of cables and pulleys was applied to generate pure moments to induce three loading plane: extension–flexion, lateral bending and axial rotation. Each moment generated a maximum torque of 1.5 Nm at a rate of 0.1 Nm/s, and the peak torque was held constantly for 10 s to stabilize the mechanical response. Under the physiological movements, specimens could present a maximum ROM without causing structural injury. Before the formal test, each movement was preloaded three times to minimize the viscoelastic effect. After the third loading, the testing system was set to halt for 30 s to minimize creep movement in order to obtain stable results that were collected and stored automatically in a computer. Meanwhile, a 3D spine motion measurement system (Eagle System, Motion Analysis) was used for image processing to identify, locate and calculate markers of C1 and C2 positions in space and to reconstruct the 3D motion of the vertebral segments (Fig. 3).
Testing sequence
Each specimen was tested in the following sequence:
-
1.
Intact group.
-
2.
Destabilization group Atlantoaxial ligament dissection and odontoidectomy were performed to induce a destabilized condition in all specimens.
-
3.
After destabilization, each specimen was stabilized in the following sequence, and the screws were not repeatedly placed in order to avoid bone–screw interference.
-
4.
Group A Unilateral C1 PS + C2 PS rod fixation (Fig. 4a).
-
5.
Group B Bilateral C1 PS + C2 PS rod fixation (Fig. 4b).
-
6.
Group C Unilateral C1 double screw (PS + LMS) + ipsilateral C2 PS combined with contralateral C2 LS rod fixation (Fig. 4c, d).
Statistical analysis
The results are described as mean ± SD. Wilcoxon paired t tests was used to test differences between groups. A P value of 0.05 was used to determine statistical significance. Statistical evaluations were performed with the software package SPSS Statistics 19.0 (SPSS, Inc., Chicago, Illinois).
Results
The mean working length, width and thickness for the C1 PS were 27.90 ± 1.16 mm, 10.70 ± 0.65 mm and 4.15 ± 0.44 mm, respectively, and the same three parameters for the C1 LMS were 21.82 ± 1.13 mm, 7.91 ± 1.01 mm and 4.62 ± 0.49 mm, respectively. The working thickness of the C1 PS was ≤ 3.5 mm in only one (1/15 = 6.7%) specimen. The other parameters were > 3.5 mm in all specimens (Table 1).
The ROM under intact, destabilized and stabilized conditions after different fixation procedures is presented in Fig. 5 and Table 2. The biomechanical results showed that all fixation groups significantly reduced flexibility in all directions compared with both the intact and destabilization group. Further, comparisons among the three different fixation groups showed better stability in all directions in Groups B and C than in Group A. However, no significant differences were observed between Groups B and C.
Discussion
The atlantoaxial complex has the most ROM in the entire cervical spine. Consequently, rigid intervertebral fixation is required to minimize motion when traumatic injuries, rheumatological disorders, infection, tumors, or other conditions result in atlantoaxial instability. Different stabilization techniques have been introduced in previous studies and have been established for clinical use to avoid persistent instability and neurological complications [2, 7, 12, 13].
Vertebral artery injuries (VAI) are rare but serious complications of cervical spine surgery. VAI has a relatively high rate of occurrence in upper cervical posterior instrumentation surgery. The rate of VAI during C1 LMS placement has been reported up to 5.8% [14, 15]. When asymmetry or unilateral occlusion is present or in the inevitable situation of VAI or in the case of unfavorable bone structures in upper cervical surgery, C1 LMS-C2 PS fixation cannot be performed using the bilateral method even though it results in greater rigidity than the unilateral method [8]. Then, unilateral fixation may be acceptable, but the patient requires an external orthosis until a fusion or bone union achieved [9]. Therefore, a secure and feasible salvage fixation method with satisfactory biomechanical stability is needed.
In 2004, the lamina screw (LS) technique was initially used to avoid injury to the vertebral artery that might occur during transarticular or PS fixation in C2 [16]. Recent studies [11, 17] reported a secure and minimally invasive method, i.e., the placement of unilateral C1 posterior arch screws and a C2 LS combined with ipsilateral C1 + C2 PS fixation, for treating atlantoaxial instability. This method via one-side incision effectively decreased the surgical invasiveness and the risk of VA injury compared with traditional bilateral fixation. Inspired by this technique, we proposed an idea to simultaneously insert two screws (PS + LMS) in the C1 unilateral lateral mass as two anchoring sites for connecting the C2 LS and PS. To demonstrate its feasibility, we reviewed the literature on C1 PS and LMS placement techniques and then modified strategy of the ideal screw path and entry point using Mimics software 17.0 (Materialise, Leuven, Belgium) to simulate the process of placing two screws in a unilateral C1 lateral mass (Fig. 1).
C1 LMS placement is a common technique for C1 fixation. However, it is technically demanding, especially when the lateral mass is obscured by a thick posterior arch or anomalous VA. One study showed that bicortical C1 LMSs were significantly stronger than unicortical screws in terms of pullout strength [5]. Therefore, bicortical C1 LMS placement is needed when the bone quality is poor, especially in osteoporotic patients. In our study, to avoid collision when the screws simultaneously inserted into the C1 unilateral lateral mass, we set the entry point of the LMS slightly lateral and inferior to the previously reported entry points [4, 6, 18, 19]. Meanwhile, the cephalad angulation was relatively smaller, at approximately 10° to 15° with the tip of the screw directed toward the inferior rim of the anterior tubercle, almost parallel with the C1 PS. The medial angulation was approximately 15°, a relatively greater value (Fig. 1). Internal carotid artery (ICA) was more common in the lateral half when it was anterior to the lateral mass. So, it is safe when we used bicortical LMSs with a higher medial angulation. However, it is to be emphasized that an overmuch medial angulation may put the VA in the risk. Regarding the morphological measurements, the working width and thickness of the LMSs were > 3.5 mm in all specimens, indicating that this LMS insertion method is feasible. The working length was 21.82 ± 1.13 mm similar to previous studies [20, 21]. However, the most difficult aspect of inserting a screw into a C1 lateral mass is the bleeding that is encountered when the undersurface of the C1 posterior arch and the posterior surface of the lateral mass are dissected.
C1 PS placement is an alternative method to overcome the limitations of the LMS, which involves placement through the posterior arch into the lateral mass. One study showed that unicortical C1 PS fixation provided the same pullout strength and biomechanical stability as bicortical C1 LMS fixation [6]. However, an anatomical study reported that the pedicle height averaged 4.80 mm, and 7.5% of C1 pedicles were less than 3.5 mm, which means they were not suitable for PS placement with a 3.5-mm-diameter screw [18]. Other previous studies have reported that the working thickness of the PS, the maximal diameter of the PS via the posterior arch, ranged from 3.95 mm to 4.93 mm [10, 18,19,20,21,22]. Our study showed that the PS mean value of working thickness was 4.15 ± 0.44 mm, which is within a reasonable range. Nonetheless, 6.7% (1/15) of the specimens were ≤ 3.5 mm and were thus not suitable for undergoing fixation with 3.5-mm-diameter PSs. To overcome this limitation, Lee et al. proposed that LMSs be inserted partially through the posterior arch (notching technique) to make the small percentage of patients with pedicle heights lower than 3.5 mm suitable for 3.5-mm screw placement [23]. In our study, the ideal screw path we proposed showed some differences from those of previous studies [6, 22]. Our cephalad angulation was a relatively high value of approximately 10°, with the tip of the screw directed toward the superior rim of the anterior tubercle that was almost parallel with the C1 LMS, and our medial angulation was a relatively low value of approximately 5° (Fig. 1). Additionally, it should be emphasized that the usual location of the hypoglossal nerve is dorsal to the ICA, approximately 2 to 3 mm lateral to the middle of the anterior aspect of the C1 lateral mass [6]. Hence, unicortical C1 PS should be adopted to avoid injury to ventral neurovascular structures.
To the best of our knowledge, the technique of unilateral C1 double screw (PS + LMS) and C2 PS combined with contralateral C2 LS rod fixation has not been previously reported. Unilateral C1–C2 PS rod fixation (Group A) is commonly used as an alternative treatment for atlantoaxial instability because its biomechanical stability is limited. Bilateral C1–C2 PS rod fixation (Group B) exhibits excellent biomechanical stability due to its long effective fixed length [6, 17]. As we expected in our study, better stability was achieved by the novel technique used in Group C than that used in Group A and provided stability similar to that in Group B under 1.5 Nm of torque. These positive biomechanical results indicate its potential application in treating atlantoaxial instability.
Compared to the traditional bilateral fixation, this novel method actually effectively prevented contralateral VAI and reduced the disruption of the contralateral soft tissue, potentially mitigating postoperative muscular dysfunction, pain and disability. However, it also has several disadvantages. First, unilateral C1 double screw actually increases the risk of ipsilateral VAI while simultaneously inserting two screws in a lateral mass. This is a drawback of the technique that needs to be emphasized. Second, the risk of VAI is increased in individuals with the presence of a posterior ponticulus when the C1 PS is inserted [24]. Third, this method will be difficult in cases where the height of the lateral mass is below 7 mm with unilateral insertion of a C1 double screw with 3.5-mm diameter. Therefore, the novel technique presented here is a salvage alternative method that is restricted by specific anatomical features. Additionally, the fusion and bone union rates in atlantoaxial instability require further clinical observation. It is important that CT scans should be performed before surgery to facilitate selection of the ideal entry point, optimal screw length and desired medial angulation. Furthermore, posterior ponticulus and VA variation should be assessed by preoperative CT angiography to minimize the risk of complications.
Conclusion
The C1 unilateral lateral mass could mostly contain two screws (PS + LMS) with diameters ≤ 3.5 mm. The novel technique of C1 double screw and ipsilateral C2 PS combined with contralateral C2 LS rod fixation provided better stability than unilateral PS rod fixation and similar as bilateral PS rod fixation. Therefore, it is a feasible salvage method that provides a new insight into atlantoaxial instability.
References
Goel A, Laheri V (1994) Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir 129(1–2):47–53
Harms J, Melcher RP (2001) Posterior C1–C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 23(22):2467–2471
Resnick DK, Benzel EC (2002) C1–C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery 50(2):426–428
Fensky F, Kueny RA, Sellenschloh K et al (2014) Biomechanical advantage of C1 pedicle screws over C1 lateral mass screws: a cadaveric study. Eur Spine J 23(4):724–731
Eck JC, Walker MP, Currier BL, Chen Q, Yaszemski MJ, An KN (2007) Biomechanical comparison of unicortical versus bicortical C1 lateral mass screw fixation. J Spin Disord Tech 20(7):505–508
Ma XY, Yin QS, Wu ZH et al (2009) C1 pedicle screws versus C1 lateral mass screws: comparisons of pullout strengths and biomechanical stabilities. Spine (Phila Pa 1976) 34(4):371–377
Richter M, Schmidt R, Claes L, Puhl W, Wilke HJ (2002) Posterior atlantoaxial fixation: biomechanical in vitro comparison of six different techniques. Spine (Phila Pa 1976) 27(16):1724–1732
Paik SC, Chun HJ, Bak KH, Ryu J, Choi KS (2015) Unilateral C1 Lateral Mass and C2 Pedicle Screw Fixation for Atlantoaxial Instability in Rheumatoid Arthritis Patients: Comparison with the Bilateral Method. J Korean Neurosurg Soc 57(6):460–464
Bhatia N, Rama A, Sievers B et al (2017) Biomechanical evaluation of unilateral versus bilateral C1 lateral mass-C2 intralaminar fixation. Global Spine J 7(3):239–245
Tan M, Wang H, Wang Y et al (2003) Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine (Phila Pa 1976) 28(9):888–895
Shen K, Deng Z, Yang J, Liu C, Zhang R (2017) Biomechanical study of novel unilateral C1 posterior arch screws and C2 laminar screws combined with an ipsilateral crossed C1–C2 pedicle screw-rod fixation for atlantoaxial instability. Arch Orthop Trauma Surg 137(10):1349–1355
Calisaneller T, Yilmaz C, Ozdemir O, Caner H (2008) Posterior atlantal lateral mass fixation technique with polyaxial screw and rod fixation system. Turkish Neurosurg 18(2):142–148
Chen JF, Wu CT, Lee SC, Lee ST (2005) Posterior atlantoaxial transpedicular screw and plate fixation. J Neurosurg Spine 2(3):386–392
Yoon KW, Ko JH, Cho CS, Lee SK, Kim YJ, Kim YJ (2013) Endovascular treatment of vertebral artery injury during cervical posterior fusion (C1 lateral mass screw). A case report. Interv Neuroradiol 19(3):370–376
Lall R, Patel NJ, Resnick DK (2010) A review of complications associated with craniocervical fusion surgery. Neurosurgery 67(5):1396–1403
Wright NM (2004) Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 17(2):158–162
Du S, Ni B, Lu X et al (2017) Application of unilateral C2 translaminar screw in the treatment for atlantoaxial instability as an alternative or salvage of pedicle screw fixation. World Neurosurg 97:86–92
Christensen DM, Eastlack RK, Lynch JJ, Yaszemski MJ, Currier BL (2007) C1 anatomy and dimensions relative to lateral mass screw placement. Spine (Phila Pa 1976) 32(8):844–848
Seal C, Zarro C, Gelb D, Ludwig S (2009) C1 lateral mass anatomy: Proper placement of lateral mass screws. J Spinal Disord Tech 22(7):516–523
Gupta T (2008) Cadaveric morphometric anatomy of C-1 vertebra in relation to lateral mass screw placement. Surg Radiol Anat 30(7):589–593
Simsek S, Yigitkanli K, Seçkin H et al (2009) Ideal screw entry point and projection angles for posterior lateral mass fixation of the atlas: an anatomical study. Eur Spine J 18(9):1321–1325
Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Zhong SZ (2007) Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine (Phila Pa 1976) 30(13):1519–1523
Lee MJ, Cassinelli E, Riew KD (2006) The feasibility of inserting atlas lateral mass screws via the posterior arch. Spine 31(24):2798–2801
Zhang XL, Huang DG, Wang XD et al (2017) The feasibility of inserting a C1 pedicle screw in patients with ponticulus posticus: a retrospective analysis of eleven patients. Eur Spine J 26(4):1058–1063
Funding
The study was supported by the national nature science foundation of China (No. 81301573), natural science foundation of Chongqing (No. cstc2013jcyjA10090), the special foundation for social safeguard and scientific innovation of Chongqing (No. cstc2016shms-ztzx10001-6), Science and technology foundation of Yuzhong district in Chongqing (No. 20160131), Chongqing research and innovation project of graduate students(No.YB17112).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have declared that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shi, L., Shen, K., Deng, R. et al. Novel unilateral C1 double screw and ipsilateral C2 pedicle screw placement combined with contralateral laminar screw–rod fixation for atlantoaxial instability. Eur Spine J 28, 362–369 (2019). https://doi.org/10.1007/s00586-018-5853-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5853-0