Abstract
Purpose
Recent studies suggest that cervical lordosis is influenced by thoracic kyphosis and that T1 slope is a key factor determining cervical sagittal alignment. However, no previous study has investigated the influence of cervical kyphosis correction on the remaining spinopelvic balance. The purpose of this study is to assess the effect of surgical correction of cervical kyphosis on thoraco-lumbo-pelvic alignment.
Methods
Fifty-five patients who underwent ≥2 level cervical fusions for cervical radiculopathy or myelopathy were included. All patients had regional or global cervical kyphosis, which was surgically corrected into lordosis. Radiographic measurements were made using whole spine standing lateral radigraphs pre- and postoperatively to analyze various sagittal parameters. The visual analogue scale (VAS) for neck pain and the neck disability index (NDI) were calculated. The paired t test was used to compare pre- and post-operative radiographic measures and functional scores. Correlations between changes in cervical sagittal parameters and those of other sagittal parameters were analyzed by Pearson’s correlation method.
Results
Preoperative kyphosis (11.4° ± 8.3°) was corrected into lordosis (−9.3° ± 8.1°). The average fusion levels were 3.3 ± 1.0. With increasing C2–C7 lordosis after surgery (from −3.4° ± 10.0° to −15° ± 7.9°), C0–C2 lordosis decreased significantly (from −34.6° ± 8.2° to −27.7° ± 8.0°) (P < 0.001). Thoracic kyphosis (from 24.8 ± 13.9° to 33.5 ± 11.9°) and T1 slope (from 12.8° ± 7.9° to 20.4° ± 5.2°) significantly increased after surgery (P < 0.001). However, other parameters did not significantly change (P > 0.05). Neck pain VAS and NDI scores (31.8 ± 16.2) significantly improved (P < 0.001). The degree of increasing C2–C7 lordosis by surgical correction was negatively correlated with changes in both thoracic kyphosis and T1 slope (P < 0.01).
Conclusions
Surgical correction of cervical kyphosis affects T1 slope and thoracic kyphosis, but not lumbo-pelvic alignment. These results indicate that the compensatory mechanisms to minimize positive sagittal malalignment of the head may occur mainly in the thoracic, and not in the lumbosacral spine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent studies have shown the importance of cervical sagittal balance, which serves to maintain horizontal gaze and global sagittal balance [1]. Cervical sagittal balance is also important because neck pain and functional disability are closely related to loss of cervical lordosis [2]. For this reason, it may be helpful to restore cervical lordosis in patients with cervical kyphosis who undergo cervical surgery. Cervical sagittal parameters such as C2–C7 lordosis, C0–C2 lordosis, and sagittal vertical axis have been shown to be closely correlated to thoraco-lumbar sagittal parameters through T1 slope and thoracic inlet angle [3]. If the T1 slope decreases, then cervical lordosis also decreases and vice versa. In addition, the T1 slope is reported to be influenced by thoracic kyphosis [4]. In a previous study, lowering of the T1 slope followed by surgical correction of thoracolumbar kyphosis resulted in decreased cervical lordosis [5, 6]. This means that surgical correction of thoracolumbar sagittal parameters, which include the middle to lower parts of spinal column, impacts cervical sagittal balance.
However, no studies have focused on the effect of surgical correction of cervical sagittal balance on the middle to lower parts of the spinal column, including on thoracic kyphosis, lumbar lordosis, or pelvic sagittal parameters. Because whole spine sagittal balance is important for the performance of the thoracolumbar spine, it is critical to evaluate the effect of surgical correction of cervical kyphosis on thoraco-lumbo-pelvic sagittal parameters [7]. The purpose of our present study was to evaluate the changes in sagittal parameters in thoracic, lumbosacral, and pelvic levels following surgical correction of cervical kyphosis.
Materials and methods
This was a retrospective analysis of prospectively collected data from 55 consecutive patients with cervical myelopathy or radiculopathy who underwent two-level or more cervical fusion surgeries between March 2009 and February 2011. All patients had regional or global cervical kyphosis. Patients with previous spine surgeries were excluded and patients who were followed up for less than 24 months were also excluded. Cases of tumor, trauma, or infection were also excluded. Demographic data, including age, sex, symptoms, operation level, and follow-up periods, were retrospectively collected from electronic medical records (EMR). Clinical data were prospectively collected by one clinical researcher during the preoperative period and at each patient visit. Neck pain and arm pain were measured using the visual analog scales (VAS). The neck disability index (NDI) was also used to assess pain. The study protocol was approved by the Institutional Review Board (IRB) of our institution, which waived the requirement for informed consent due to the retrospective nature of this study.
Radiological measurements
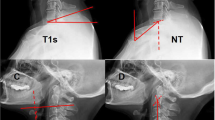
Radiological data were measured using a picture archiving communication system (PACS). Whole spine standing lateral radiographs were obtained from patients in a standardized position with arms straightforward and folded. On the radiographs, we measured radiological parameters as follows: (1) kyphosis angle (2) C0–C2 lordosis (3) C2–C7 lordosis (4) C2–C7 sagittal vertical axis (SVA) (5) T1 slope, (6) thoracic kyphosis (TK), (7) lumbar lordosis (LL), (8) sacral slope (SS), and (9) C7–S1 sagittal vertical axis (SVA). The kyphosis angle was measured as the Cobb’s angle generated by the involved kyphotic segments. The C0–C2 lordosis was measured as the angle between the line from the anterosuperior border of the atlas to the inferior end of the occiput and lower endplates of C2. The C2–C7 lordosis was defined by the Cobb’s angle between the lower endplates of C2 and C7. The C2–C7 SVA was defined as the distance from the posterosuperior corner of C7 and the vertical line from the center of the C2 body. The T1 slope was measured as the angle between the upper endplate of T1 and the horizontal line. Thoracic kyphosis was measured by Cobb’s angle between the upper endplate of T1 and the lower endplate of T12. Lumbar lordosis was defined by the Cobb’s angle between both upper endplates of L1 and S1. The sacral slope was defined by the angle between the upper endplates of the sacrum and the horizontal line. The C7–S1 SVA was defined as the distance from the posterosuperior corner of S1 and the vertical line from the center of the C7 body. The methods of measurement are summarized in Fig. 1.
Measurements of radiological parameters, including a C0–C2 lordosis, C2–C7 lordosis, C2–C7 sagittal vertical axis (SVA) (asterisk), and T1 slope (arrow) in magnified view of the cervical spine, and b thoracic kyphosis, lumbar lordosis, sacral slope, and C7–S1 sagittal vertical axis (asterisk) in whole-spine standing lateral radiographs
Operation methods
Three types of operations were performed: (1) anterior cervical discectomy and fusion (ACDF), (2) posterior laminectomy and fusion, and (3) combined ACDF and posterior laminectomy and fusion. Fibular allograft was used for disc height elevation to generate cervical lordosis in ACDF procedures. Slightly more lordotic rod bending was performed to produce a cervical lordotic angle in posterior surgeries. Level selection of surgeries depended on patient symptoms and the degree of cord or root compression on magnetic resonance imaging (MRI). Patients were regularly followed up at 1, 3, 6, and 12 months after surgery and yearly thereafter.
Statistical analysis
Changes in clinical and radiological parameters from preoperative to postoperative 2-year period were compared by paired t tests. Correlation analysis was performed between changes in C2–C7 lordosis with other thoraco-lumbo-pelvic parameters by Pearson’s correlation method. All statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS, version 21.0, Inc, Chicago, IL, USA), with P values less than 0.05 considered to be statistically significant.
Results
Of the 55 patients in our study series, 25 (45.5 %) were men, and the mean age was 59.0 ± 12.3 years. The mean kyphotic segments were 3.3 ± 1.0 (range 2–5 segments) and operation levels were 3.1 ± 1.3 (range 2–6 levels). Etiologies of the diseases and symptoms of the patients were shown in Table 1. Surgery consisted of ACDF in 40 patients (72.7 %), posterior laminectomy and fusion in six patients (10.9 %), and combined anterior and posterior procedures in nine patients (16.4 %). The patients were followed up for 30.3 ± 5.1 months. A representative case is illustrated in Fig. 2.
Case illustration of a 63-year-old male patient who underwent 2 level anterior cervical discectomy and fusion (ACDF, C5–6–7) for cervical myeloradiculopathy a MRI showing high signal intensity in the cord at the C5–6 level and cord compression at the C6–7 level. b Radiological parameters measured in the preoperative period. c Radiological parameters measured at postoperative 2 years
Postoperative changes in clinical and radiological parameters
An overall improvement in clinical parameters was seen after surgery. Neck pain VAS improved from 3.6 ± 2.9 to 1.6 ± 2.2 (P < 0.001). NDI also improved after surgery (from 14.1 ± 9.8 to 8.9 ± 8.3, P < 0.001).
In terms of radiological parameters, positive changes in cervical sagittal balance were noted after surgery. The preoperative kyphotic angle of involved segments changed into a lordotic angle following surgeries (from 11.4° to −9.3°, P < 0.001). In addition, C2–C7 lordosis increased (from −3.4° to −15.6°, P < 0.001) and C0–C2 lordosis decreased (from −34.6° to −27.7°, P < 0.001). The T1 slope increased from 12.8° to 20.4° (P < 0.001), while thoracic kyphosis increased from 24.8° to 32.5° (P < 0.001) after surgery. However, other lumbosacral and pelvic sagittal parameters did not significantly change after surgery. Overall changes in radiological parameters are described in Table 2.
Correlation between changes in radiological parameters
The degree of correction positively correlated with changes in C2–C7 lordosis (R = 0.588). However, reduction of kyphosis angle correlated with the increase of T1 slope and TK (R = −0.559 and −0.373, respectively). The degree of C2–C7 lordosis restoration also negatively correlated with changes in T1 slope and TK (R = −0.417 and −0.310, respectively). In addition, there was a strongly positive relationship between the change in T1 slope and the change in TK (R = 0.558). Although C0–C2 lordosis decreased after surgery, this change did not correlate with other sagittal parameters. In addition, changes in both kyphosis angle and C2–C7 lordosis did not show any correlation with changes in lumbo-pelvic parameters such as lumbar lordosis or sacral slope. Overall data are summarized in Table 3. Scatter plots showing the relationship between changes in cervical sagittal parameters and changes in thoraco-lumbo-pelvic parameters are illustrated in Fig. 3.
Scatter plots showing the relationship between changes in cervical sagittal parameters and T1 slope/thoracic kyphosis (TK). a, b Evidence of a strong negative correlation between changes in kyphosis angle and T1 slope (R = −0.559)/TK (R = −0.373). c, d A negative correlation was found between changes in C2–C7 lordosis and T1 slope (R = −0.417)/thoracic kyphosis (R = −0.310)
Discussion
The results of our present study indicate that surgical correction of cervical kyphosis affects thoracic kyphosis. Furthermore, symptoms including neck pain VAS and NDI were also improved. However, improvement of symptoms are thought to be attributed to the treatment of the underlying disease as well as surgical correction of kyphosis. Radiological improvements are thought to occur through increased T1 slope, which was previously reported to be a mediator of the change from thoracic to cervical sagittal alignment [4]. However, surgery had no effect on lumbo-pelvic sagittal balance in the current study.
Although it is thought that improvements of symptoms are mainly attributed to the treatment of the disease, cervical sagittal malalignment has been reported to be related to neck pain, functional disability, and deteriorated general health [2]. In patients undergoing posterior cervical fusion for cervical myelopathy, maintenance of cervical sagittal balance is reported to help improve symptoms and general health-related quality of life [2, 8, 9]. Positive sagittal malalignment such as increased C2–C7 SVA or decreased cervical lordosis is positively correlated with severity of disability and negatively correlated with health-related quality of life (e.g., SF-36 PCS) [2]. The mechanisms underlying these results have been partially explained in animal and cadaveric studies. In an animal model, cervical kyphotic deformity caused demyelination and neuronal loss in the spinal cords of animals [10]. In another cadaveric study, spinal cord intramedullary pressure increased when cervical kyphosis was >7.5° [11]. In addition, cervical sagittal alignment has been shown to be related to thoracic, lumbar, and pelvic sagittal alignment [4]. C2–C7 lordosis is correlated to thoracic inlet angle and T1 slope, which are also correlated to thoracic kyphosis [3, 12, 13]. For these reasons, correction of cervical kyphosis should be considered during cervical surgeries including cervical myelopathy.
In fact, correction of thoracolumbar deformity has been reported to influence cervical sagittal balance. Surgical correction of global sagittal imbalance by pedicle subtraction osteotomy results in improvement of abnormal hyperlordosis, which is a compensatory mechanism to maintain forward gaze [6]. Cervical reciprocal changes have been observed after corrective thoracolumbar deformity surgery [5]. Recently, it has been also suggested that lower cervical lordosis was modified by adult degenerative scoliosis surgery and lumbar pedicle subtraction osteotomy [14, 15]. Reliability of radiological measurements for sagittal balance including cervical spine was also proven in patients with scoliosis [16]. In addition, it was reported that adequate sagittal balance could be obtained by osteotomy in patients with proximal junctional kyphosis of the cervicothoracic spine [17]. However, to the best of our knowledge, no study has reported the effects of surgical correction of cervical sagittal malalignment on thoracolumbar or pelvic sagittal parameters. The aim of our current study was to show the direct cause and effect relationship by revealing that global sagittal malalignment can be influenced by surgical correction of cervical sagittal malalignment.
There were several noteworthy findings in our present investigation. The T1 slope was revealed as an important mediator between cervical and thoracic sagittal parameters, which is in agreement with the results of previous studies [4, 18]. The T1 slope is an important radiological parameter to maintain forward gaze via mediating cervical lordosis. As the T1 slope increases, C2–C7 lordosis also increases to maintain cervical sagittal balance, which explains why hyperlordosis of the cervical spine is frequently observed in patients with thoracolumbar kyphotic deformity. Hyperlordosis of the cervical spine can be corrected following corrective surgery of thoracolumbar kyphosis through changes in the T1 slope [6, 19]. In the same way, our present study showed that thoracic hypokyphosis can also be corrected by restoration of cervical sagittal balance through the effects on the T1 slope. In addition, preoperatively shown C0–C2 hyperlordosis tended to decrease (from 34.6° to 27.7°) after surgery. C0–C2 lordosis is known to be negatively correlated with C2–C7 lordosis [3]. This means that if C2–C7 lordosis decreases, a compensation mechanism is activated by increasing C0–C2 lordosis. This may be explained via a mechanism in which excessive stress on the high cervical spine by C0–C2 hyperlordosis is also mitigated by correction of subaxial cervical sagittal balance. However, interestingly, correction of cervical sagittal balance does not impact levels beyond the thoracic spine. Taken together, these results indicate that the compensation mechanism to maintain cervical sagittal balance may stem from an interaction between cervical lordosis, T1 slope, and thoracic kyphosis. This mechanism may also contribute to maintenance of similar C2–C7 SVA from the pre- to postoperative period (from 17.8 to 16.2 mm).
The dynamic reason of correlation between cervical pain and sagittal balance is thought to be as follows. In patients with cervical myelopathy or radiculopathy, cervical forward bending is usually observed because cervical diameter is normally increased by that position. In that condition, thoracic kyphosis usually decreases to maintain forward gazing. However, elimination of the cervical pain causes restoration of cervical lordosis because of no need for cervical forward bending, which leads to increase of thoracic kyphosis. So, the cervical shape itself is not considered to be the main reason of the thoracic sagittal imbalance.
Our present analyses had a few limitations of note, many of which are associated with the retrospective study design. First, surgical procedures were not uniform. Not only different approaches were used, but the level selection was also variable. Second, the original purpose of the surgeries was not correction of a deformity; most surgeries were performed to treat cervical myelopathy or radiculopathy. In particular, the symptom could be aggravated by extension position, which could have effect on posture preoperatively. This could be one of reasons of bias. In addition, the degree of surgical correction was small. Nonetheless, we identified a close relationship between cervical and thoracic sagittal parameters, which may be explained by the T1 slope. Furthermore, we believe that our current study reflects real clinical settings because cervical deformity surgery is not frequently performed. Third, the follow-up period was relatively short. Because cervical lordosis is reported to decrease with time, long-term outcomes may differ from those of the present study. However, our present analysis is valuable and unique in that it reports the direct effect of surgical correction of cervical kyphosis on thoraco-lumbo-pelvic sagittal alignment.
In summary, our findings suggest that surgical correction of cervical kyphosis can restore preoperatively decreased T1 slope and thoracic kyphosis. Considering that no significant changes were found in the lumbar and pelvic sagittal parameters postoperatively, the compensatory mechanisms to minimize positive sagittal malalignment of the head may occur mainly in the thoracic level. Correction of cervical sagittal imbalance did not impact lumbar or pelvic sagittal parameters. However, further studies are required to clarify the complex reciprocal relationships between cervical, thoracic, lumbar, and pelvic sagittal parameters.
References
Scheer JK, Tang JA, Smith JS, Acosta FL Jr, Protopsaltis TS, Blondel B, Bess S, Shaffrey CI, Deviren V, Lafage V, Schwab F, Ames CP (2013) Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 19:141–159. doi:10.3171/2013.4.spine12838
Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, Lafage V, Shaffrey CI, Schwab F, Ames CP, ISSG (2012) The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery 71:662–669. doi:10.1227/NEU.0b013e31826100c9
Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES (2012) The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech 25:E41–E47. doi:10.1097/BSD.0b013e3182396301
Lee SH, Son ES, Seo EM, Suk KS, Kim KT (2015) Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 15:705–712. doi:10.1016/j.spinee.2013.06.059
Ha Y, Schwab F, Lafage V, Mundis G, Shaffrey C, Smith J, Bess S, Ames C (2014) Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J 23:552–559. doi:10.1007/s00586-013-2953-8
Smith JS, Shaffrey CI, Lafage V, Blondel B, Schwab F, Hostin R, Hart R, O’Shaughnessy B, Bess S, Hu SS, Deviren V, Ames CP; International Spine Study Group (2012) Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine 17:300–307. doi:10.3171/2012.6.SPINE1250
Scheer JK, Tang JA, Smith JS, Acosta FL, Protopsaltis TS, Blondel B, Bess S, Shaffrey CI, Deviren V, Lafage V, Schwab F, Ames CP; International Spine Study Group (2013) Cervical spine alignment, sagittal deformity, and clinical implications: a review. J Neurosurg Spine 19:141–159. doi:10.3171/2013.4.SPINE12838
Roguski M, Benzel EC, Curran JN, Magge SN, Bisson EF, Krishnaney AA, Steinmetz MP, Butler WE, Heary RF, Ghogawala Z (2014) Postoperative cervical sagittal imbalance negatively affects outcomes following surgery for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 39:2070–2077. doi:10.1097/BRS.0000000000000641
Shamji MF, Ames CP, Smith JS, Rhee JM, Chapman JR, Fehlings MG (2013) Myelopathy and spinal deformity: relevance of spinal alignment in planning surgical intervention for degenerative cervical myelopathy. Spine (Phila Pa 1976) 38:S147–S148. doi:10.1097/BRS.0b013e3182a7f52
Shimizu K, Nakamura M, Nishikawa Y, Hijikata S, Chiba K, Toyama Y (2005) Spinal kyphosis causes demyelination and neuronal loss in the spinal cord: a new model of kyphotic deformity using juvenile Japanese small game fowls. Spine (Phila Pa 1976) 30:2388–2392
Chavanne A, Pettigrew DB, Holtz JR, Dollin N, Kuntz C 4th (2011) Spinal cord intramedullary pressure in cervical kyphotic deformity: a cadaveric study. Spine (Phila Pa 1976) 36:1619–1626. doi:10.1097/BRS.0b013e3181fc17b0
Lee SH, Son ES, Seo EM, Suk KS, Kim KT (2013) Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 15:705–712. doi:10.1016/j.spinee.2013.06.059
Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, Patel AA, Traynelis VC, Kim HJ, Shaffrey CI, Smith JS, Lafage V (2013) Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 38:S149–S160. doi:10.1097/BRS.0b013e3182a7f449
Boissière L, Bernard J, Vital JM, Pointillart V, Mariey R, Gille O, Obeid I (2015) Cervical spine balance: postoperative radiologic changes in adult scoliosis surgery. Eur Spine J 24:1356–1361. doi:10.1007/s00586-015-3854-9
Obeid I, Boniello A, Boissiere L, Bourghli A, Pointillart V, Gille O, Lafage V, Vital JM (2015) Cervical spine alignment following lumbar pedicle subtraction osteotomy for sagittal imbalance. Eur Spine J 24:1191–1198. doi:10.1007/s00586-014-3738-4
Vidal C, Ilharreborde B, Azoulay R, Sebag G, Mazda K (2013) Reliability of cervical lordosis and global sagittal spinal balance measurements in adolescent idiopathic scoliosis. Eur Spine J 22:1362–1367. doi:10.1007/s00586-013-2752-2
Cecchinato R, Berjano P, Bassani R, Lamartina C (2015) Osteotomies in proximal junctional kyphosis in the cerviothoracic area. Eur Spine J 24(Suppl 1):S31–S37. doi:10.1007/s00586-014-3654-7
Knott PT, Mardjetko SM, Techy F (2010) The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 10:994–998. doi:10.1016/j.spinee.2010.08.031
Lafage V, Ames C, Schwab F, Klineberg E, Akbarnia B, Smith J, Boachie-Adjei O, Burton D, Hart R, Hostin R, Shaffrey C, Wood K, Bess S; International Spine Study Group (2012) Changes in thoracic kyphosis negatively impact sagittal alignment after lumbar pedicle subtraction osteotomy: a comprehensive radiographic analysis. Spine (Phila Pa 1976) 37:E180–E187. doi:10.1097/BRS.0b013e318225b926
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Lee, DH., Ha, JK., Chung, JH. et al. A retrospective study to reveal the effect of surgical correction of cervical kyphosis on thoraco-lumbo-pelvic sagittal alignment. Eur Spine J 25, 2286–2293 (2016). https://doi.org/10.1007/s00586-016-4392-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4392-9