Abstract
Purpose
Given that the disc moves simultaneously with facet joints, there would be a relationship between Modic changes and facet joint degeneration in the cervical spine. However, there is no literature investigating the relationship. The purpose is to evaluate the relationship between Modic changes and facet joint degeneration in the cervical spine.
Methods
Ninety-eight patients underwent both computed tomography (CT) and magnetic resonance images (MRI) of the cervical spine. They consisted of fifty-one males and forty-eight females and their mean age was 60.1 years (ranged from 40 years to 81 years). We compared the degree of facet joint degeneration based on CTs with Modic changes based on MRIs from C2–C3 to C6–C7. The degree of facet joint degeneration was classified into four categories and Modic changes were classified into four types. Disc degeneration was determined with Miyazaki’s grading system.
Results
Facet joint degeneration was most common at C2–C3 and C4–C5 and rarest at C6–C7. Modic changes were most common at C2–C3 and rarest at C6–C7. However, there was no relationship between facet joint degeneration and any Modic changes at the same level. However, the presence of facet joint degeneration and the presence of Modic change are common in high grades of disc degeneration at the same level of the cervical spine.
Conclusion
Modic changes and facet joint degeneration are most common at C2–C3 in the cervical spine. However, there were no relationships between the presence of Modic changes and facet joint degeneration at the same level of the cervical spine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The Prevalence of Modic changes in the cervical spine has been reported in several studies [1–4]. Hayashi et al., found that cervical disc levels with Modic changes were significantly more likely to have disc degeneration and less angular motion, suggesting that Modic changes may correlate with loss of mobility [3]. As the disc degenerates, the endplates of the disc spaces develop spurs and other arthritic changes. Master et at., determined that such cervical endplate arthritic changes precede cervical facet arthrosis in a cadaveric study [5]. Given that the disc moves simultaneously with facet joints, we hypothesized that there would be a correlation between Modic changes on MRI images and facet joint arthrosis seen on CT scans. To our knowledge, there have been no investigations of such a hypothesis. Therefore, the objective of this study was to elucidate the relationship between Modic changes and facet joint degeneration in the cervical spine.
Materials and methods
This study was approved by the institutional review board at the institution of the corresponding author (IRB number: 2013-I131). We analyzed the collected clinical information and digitalized image documents retrospectively, but had received a generic agreement from every adult patient authorizing us to use the clinical information and image documents for clinical studies. We included all patients who underwent both CT and MRI of cervical spine at the same time because of symptomatic cervical spine issues, including neck pain, pain radiating to arm or walking difficulty from January 2003 to January 2012 at the first author’s academic institution. Both studies had to be retrievable on our computerized system and be of adequate quality to make readings. We do not routinely obtain CT scans on patients, but rather, only when we feel that the information adds to their clinical management. Indications for the CT included the following: evaluate for the possibility and severity of hard disc herniations in patients with cervical radiculopathy, ossification of posterior longitudinal ligament, facet arthrosis and facet auto-fusion. We excluded patients with trauma, tumor, infectious spondylitis, inflammatory spondylitis of gout, rheumatoid arthritis, ankylosing spondylitis, ossification of posterior longitudinal ligament (OPLL), Arnold Chiari malformation, Klippel–Feil syndrome. We included patients with symptoms of neck pain, radiculopathy or gait disturbance due to cervical spondylosis.
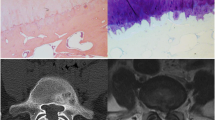
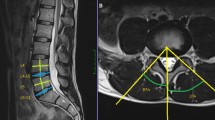
We compared the degree of facet joint degeneration based on CT with the Modic change based on MRI from C2–C3 to C6–C7. The degree of cervical facet degeneration was determined on a PACS viewer using the axial, sagittal or coronal images from C2 to C7 bilaterally [6]. The degree of degeneration was graded into 4 categories: grade I, normal; grade II, degenerative changes including joint space narrowing, cyst formation, small osteophytes without joint hypertrophy seen on axial or sagittal images; grade III, joint hypertrophy secondary to large osteophytes without fusion on axial or coronal images; grade IV, bony fusion of the joint seen on sagittal images [6]. Four types of Modic changes were described as follows; type 0: within normal limit, type 1: hypointense signal on T1-weighted sequences and hyperintense signal on T2-weighted sequences, type 2: hyperintense signal on T1 sequences and hyper- or isointense signal on T2 sequences, type 3: hypointense signal on T1 and T2 sequences. The disc degeneration was determined with MRI on a PACS viewer using the sagittal images from C2 to C7 with Miyazaki’s grading system (Table 1) [7].
All statistical analyses were performed with a SPSS version 13.0 for Windows (Chicago, IL, USA). Chi-square test was used for analysis of the nominal and ordinal variables. Power analysis was performed using G*Power version 3.1.5 (Germany). Power was 0.95 for Chi-Square test with the effect size of 0.5. The sample size in each group needed to be more than 80. Intra-observer and inter-observer reliabilities for cervical facet degeneration based on CT were good at 0.878 and 0.869, respectively, using ICC reliability statistics in the previous study [6]. Intra-observer and inter-observer reliabilities for Modic change in cervical spine were substantial at 0.62–0.74 and 0.64–0.78, respectively, using Kappa statistics in the previous studies [1, 3]. Intra-observer and inter-observer reliabilities for cervical disc degeneration by Miyazaki’s grading system were substantial at 0.907–0.950 and 0.730–0.826, respectively, using Kappa statistics in the previous study [7].
Results
We identified 98 patients who fit the inclusion criteria. They consist of fifty males and forty-eight females and their mean age was 60.0 years (ranged from 40 to 81 years). A total of four hundred and ninety cervical levels were evaluated in the ninety-eight patients. Cervical facet degeneration more than grade I was found in 68 cervical levels (13.9 %): 24 cervical levels of facet grade II (4.9 %), 41 cervical levels of facet grade III (8.4 %), and 3 cervical levels of facet grade IV (0.6 %). Modic changes were found in 83 cervical levels (16.9 %): 5 of type 1 (1.0 %), 65 of type 2 (13.3 %) and 13 of type 3 (2.6 %). Disc degeneration was found in 5 cervical levels of grade 1 (1.0 %), 97 of grade 2 (19.8 %), 286 of grade 3 (58.4 %), 72 of grade 4 (14.7 %) and 30 of grade 5 (6.1 %).
Facet joint degeneration was most common at C2–C3 and C4–C5 and rarest at C6–C7. There were 20 cases of facet joint degeneration (above facet grade I) at C2–C3 (29.4 %), 12 cases at C3–C4 (17.6 %), 21 cases at C4–C5 (30.9 %), 9 cases at C5–C6 (13.2 %) and 6 cases at C6–C7 (8.8 %), respectively (Tables 2, 3). Modic changes were most common at C2–C3 and rarest at C6–C7. There were 38 cases of Modic changes at C2–C3 (45.8 %), 16 cases at C3–C4 (19.3 %), 11 cases at C4–C5 (13.3 %), 11 cases at C5–C6 (13.3 %), and 7 cases at C6–C7 (8.4 %), respectively (Tables 2, 3).
There was no relationship between the presence of facet joint degeneration (above facet grade I) and any Modic changes at the same level of the cervical spine (p = 0.857, Table 4). In addition, there were no relationships between the presence of facet joint degeneration and the presence of subgroup types 1, 2 or 3 Modic changes at the same level of the cervical spine (p = 1.000, p = 0.902, p = 1.000, Table 4).
However, the presence of facet joint degeneration is common in high grades of disc degeneration by Miyazaki’s grading system at the same level of the cervical spine (p = 0.030, Table 5). The presence of Modic change is common in high grades of disc degeneration by Miyazaki’s grading system at the same level of the cervical spine (p = 0.000, Table 6).
Discussion
Signal intensity changes in the vertebral endplates and subchondral bone are often observed on MRIs of patients with spinal degenerative diseases. Most of the literatures on Modic marrow changes have focused on the lumbar spine. Modic changes have been linked with low back pain and are, therefore, clinically relevant findings seen on lumbar MRI scans [8, 9]. In addition, Modic changes and facet joint degeneration in the lumbar spine are most common at L4–L5 [10–12]. However, there was no report regarding the relationship between Modic changes and facet joint degeneration in the cervical spine. The objective of this study was to elucidate the relationship between Modic changes and facet joint degeneration in the cervical spine.
Facet joint degeneration was most common at C2–C3 and C4–C5 and rarest at C6–C7. Modic changes were most common at C2–C3 and rarest at C6–C7. However, there was no relationship between the presence of Modic changes and the presence of facet joint degeneration at the same level of the cervical spine. Also, there were no relationships between the presence of facet joint degeneration and the presence of subgroup types 1, 2 or 3 Modic changes at the same level of the cervical spine. However, the presence of facet joint degeneration and the presence of Modic change are common in high grades of disc degeneration at the same level of the cervical spine.
We could only identify a few studies that had reported strictly on the prevalence of Modic changes in the cervical spine (Table 7) [1–4]. In a prospective study with asymptomatic volunteers with a mean age of 49.8 years, Modic changes in the cervical spine were found in 10 out of 223 patients (4.5 %) with the C5–C6 cervical level being the most common (Table 7) [1]. Age (≥40 years), gender (male), and pre-existing disc degeneration were significantly associated with newly developed Modic changes [1]. In a clinical study of patients complaining of neck pain, Modic changes were observed in 19 out of 118 patients (16.1 %), with the C5–C6 cervical level being the most common (Table 7) [2]. Type 1 Modic changes were found to be the most common in the cervical spine (Table 7) [2]. Another clinical study of patients complaining of neck pain showed that Modic changes in the cervical spine were observed in 84 out of 437 patients (19.2 %) with the C5–C6 cervical level being the most commonly involved (Table 7) [3]. However, type 2 Modic changes were the most common (Table 7) [3]. In the study of an older population with a mean age of 61.7 years, the prevalence of Modic changes in the cervical spine was 40.4 % with type 2 predominating (Table 7). The C6–C7 cervical level was most commonly affected [4].
In the current study, type 2 Modic changes were most common, similar to a previous study in which the population was of a similar age [4]. In contrast, it is not concordant to two previous studies where type 1 changes were dominant [1, 2]. This is most likely explained by the fact that the mean age of the current study population was 60.1 years, much older than that of those studies (Table 7) [1, 2]. In addition, Modic type 1 changes are expected to further degenerate into type 2 over time [1, 13]. A prospective study with asymptomatic volunteers with a mean age of 49.8 years demonstrated that type 1 Modic changes were most common initially in the cervical spine. Over a ten-year period, type 2 Modic changes newly developed most frequently [1]. In another study in patients with neck pain, Modic changes in the cervical spine were a dynamic phenomenon, similar to the lumbar spine [13]. The conversion of Modic type 1 to 2 over time was a common pattern observed in patients [13].
Modic changes were most common at the C2–C3 level in the current study. This is discordant with previous studies [1–4] and might be explained by the fact that our study population was symptomatic with neck and/or radiating arm pain or walking difficulty. However, the study population in previous studies was either asymptomatic or had neck pain only [1, 4, 10, 11]. In addition, there has been controversy about the most common level with Modic change in the cervical spine, similar to the controversy about the most common level in the lumbar spine. Asymptomatic Modic changes are common at the upper lumbar levels (L1–L2–L3–L4) whereas those with lower back pain have them most commonly at L5–S1 [14]. The C5–C6 cervical level was most affected in some studies [1–3], while C6–C7 was most affected in another [4].
High grades of disc degeneration are associated with the presence of Modic change at the same level of the cervical spine, which is concordant with a previous study of cervical spine of symptomatic patients with neck pain [3]. Similarly, high grades of disc degeneration are associated with the presence of facet joint degeneration at the same level of the cervical spine. However, there was no concordance in the presence of Modic changes and facet joint degeneration at the same level of the cervical spine. This contradicts a previous study of 234 cadaveric cervical spines [5]. They found that concurrent cervical endplate arthrosis and facet arthrosis were present in 77 % of the study population [5]. This might be explained by the fact that the grading systems were different. The grading system in the current study is comprised cervical facet degeneration based on CTs and Modic changes based on MRI. Instead, the previous cadaveric study used simple visual inspection to grade the degree of arthrosis in the facet joint or endplate based on the extent of osteophytes in the joint [5]. Of note, no one has confirmed the concurrent presence of lumbar Modic changes and facet arthrosis, although Modic changes and facet joint degeneration in the lumbar spine are reported to be most common at L4–L5 [10–12].
As with any study, the present investigation has several limitations. First, it is a retrospective study. Our study could be improved with a prospective study of volunteers who undergo cervical CT and MRI. However, the relative advantages of a prospective study in a study such as ours are minimal. Second, our study could be improved by having a large number of subjects with a broad spectrum of ages ranging from the young to the elderly. Third, for the foreseeable future, there is relatively minor clinical relevance to our study, as it is more of a basic science study designed to determine the relationship between the degenerative changes seen in discs versus facet joints. Fourth, unfortunately, we did not compare the degree of facet joint degeneration based on CT and the Modic change based on MRI with clinical symptoms, since it is known that they are not completely accurate without confirmatory blocks. Degenerative changes seen on radiologic studies are often not symptomatic. One possible current clinical application is that when considering a patient for cervical arthroplasty, Modic changes on MRI will not be predictive of facet arthrosis, a contraindication for that procedure. The strength of our study is that, to the best of our knowledge, this represents the first set of data determining Modic changes and facet joint degeneration in the cervical spine.
In conclusion, we found that there is no relationship between the presence of Modic changes and the presence of facet joint degeneration at the same level in the cervical spine. Our results suggest that Modic changes and facet joint degeneration may appear independently of each other in the cervical spine and that one does not necessarily result in the other.
References
Matsumoto M, Okada E, Ichihara D, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Takahata T (2012) Modic changes in the cervical spine: prospective 10-year follow-up study in asymptomatic subjects. J Bone Joint Surg Br 94:678–683. doi:10.1302/0301-620X.94B5.28519
Peterson CK, Humphreys BK, Pringle TC (2007) Prevalence of modic degenerative marrow changes in the cervical spine. J Manipulative Physiol Ther 30:5–10. doi:10.1016/j.jmpt.2006.11.013
Hayashi T, Daubs MD, Suzuki A, Phan K, Shiba K, Wang JC (2014) Effect of Modic changes on spinal canal stenosis and segmental motion in cervical spine. Eur Spine J. doi:10.1007/s00586-014-3406-8
Mann E, Peterson CK, Hodler J (2011) Degenerative marrow (modic) changes on cervical spine magnetic resonance imaging scans: prevalence, inter- and intra-examiner reliability and link to disc herniation. Spine (Phila Pa 1976) 36:1081–1085. doi:10.1097/BRS.0b013e3181ef6a1e
Master DL, Toy JO, Eubanks JD, Ahn NU (2012) Cervical Endplate and Facet Arthrosis: An Anatomic Study of Cadaveric Specimens. J Spinal Disord Tech 25:379–382. doi:10.1097/BSD.0b013e318224a60f
Park MS, Moon SH, Lee HM, Kim TH, Oh JB, Riew KD (2014) Facet joint degeneration of the cervical spine: a computed tomographic analysis of 320 patients. Spine 39:E713–E718
Miyazaki M, Hong SW, Yoon SH, Morishita Y, Wang JC (2008) Reliability of a magnetic resonance imaging-based grading system for cervical intervertebral disc degeneration. J Spinal Disord Tech 21:288–292. doi:10.1097/BSD.0b013e31813c0e59
Braithwaite I, White J, Saifuddin A, Renton P, Taylor BA (1998) Vertebral end-plate (Modic) changes on lumbar spine MRI: correlation with pain reproduction at lumbar discography. Eur Spine J 7:363–368
Kjaer P, Korsholm L, Bendix T, Sorensen JS, Leboeuf-Yde C (2006) Modic changes and their associations with clinical findings. Eur Spine J 15:1312–1319. doi:10.1007/s00586-006-0185-x
Zhang YH, Zhao CQ, Jiang LS, Chen XD, Dai LY (2008) Modic changes: a systematic review of the literature. Eur Spine J 17:1289–1299. doi:10.1007/s00586-008-0758-y
Jensen TS, Karppinen J, Sorensen JS, Niinimaki J, Leboeuf-Yde C (2008) Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J 17:1407–1422. doi:10.1007/s00586-008-0770-2
Wang Y, Videman T, Battie MC (2012) Modic changes: prevalence, distribution patterns, and association with age in white men. Spine J 12:411–416. doi:10.1016/j.spinee.2012.03.026
Mann E, Peterson CK, Hodler J, Pfirrmann CW (2014) The evolution of degenerative marrow (Modic) changes in the cervical spine in neck pain patients. Eur Spine J 23:584–589. doi:10.1007/s00586-013-2882-6
Kuisma M, Karppinen J, Niinimaki J, Ojala R, Haapea M, Heliovaara M, Korpelainen R, Taimela S, Natri A, Tervonen O (2007) Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine (Phila Pa 1976) 32:1116–1122. doi:10.1097/01.brs.0000261561.12944.ff
Acknowledgments
This article has no financial relationship with the organization that sponsored the research. Authors have full control of all primary data and agree to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author K. Daniel Riew is a member of CSRS, KASS, received royalties from Osprey, Biomet, Medtronic Sofamor Danek and owns stock in Osprey, Expanding Orthopedics, Spineology, Spinal Kinetics, Amedica, Nexgen Spine, Vertiflex, Benvenue, Paradigm Spine, PSD. The other authors declare that they have no conflict of interest.
Additional information
The manuscript submitted does not contain information about medical device(s)/drug(s).
Rights and permissions
About this article
Cite this article
Park, M.S., Moon, SH., Kim, TH. et al. Relationship between modic changes and facet joint degeneration in the cervical spine. Eur Spine J 24, 2999–3004 (2015). https://doi.org/10.1007/s00586-015-4257-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4257-7