Abstract
Purpose
Lumbar disc degeneration may be associated with intensity of neovascularization in disc herniations. Our study was designed to evaluate how much the severity of histodegeneration is related to the development of neovascularization and to the level of pleiotrophin in the herniated lumbar discs.
Methods
Surgically excised lumbar disc specimens were obtained from 29 patients with noncontained (i.e., extruding through the posterior longitudinal ligament) and 21 patients with contained disc herniations. The histodegeneration scores and levels of neovascularization were estimated according to semiquantitative analysis in lumbar disc and endplate samples. Immunohistochemical staining were performed to identify the newly formed blood vessels and to detect the presence of pleiotrophin in the specimens.
Results
Higher levels of disc and endplate neovascularity were registered in noncontained herniations. The level of neovascularization was significantly related to the score of histodegeneration in the herniated disc tissues but not in the endplate specimens. Both contained and noncontained herniations had the highest values of histodegeneration in conjunction with the highest level of neovascularization but the relations between neovascularity and degenerative changes remained to be significant only in the group of noncontained herniations. Registration or frequency of pleiotrophin positive cells did not correlate significantly with histodegeneration or level of neovascularization in the disc samples.
Conclusion
Severe histodegeneration of the lumbar disc herniations is associated with enhanced neovascularization and potentially also spontaneous regression of the herniated tissue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neovascularization is recognized as an important factor potentially related to the spontaneous resorption of the herniated intervertebral discs (IVDs) [1–4]. Disc herniation into the epidural space may precipitate inflammatory cell infiltration, granulation tissue formation, neovascularization, and activation of proteolytic enzymes potentially leading to shrinkage of the herniations [1, 2, 5–7].
The normal IVD is a predominantly avascular structure, and blood vessels exist only in the longitudinal ligaments and the outer layers of the anulus fibrosus. Several authors have described degenerative changes in conjunction with enhanced neovascularization in the lumbar disc herniations [2, 5, 8], but infiltration of blood vessels into the degenerating disc has been detected also without herniations [9–11]. Furthermore, Nehrlich et al. [12] have established that vascular ingrowth should not be considered as a distinct feature of disc degeneration and different ability of neovascularization has been observed in different compartments of the disc [4, 13].
Vascular ingrowth into the disc has been described to occur together with breakdown of the proteoglycan matrix of the IVD, proliferation of granulation tissue and accumulation of cytokines and growth factors [2, 3, 6, 14, 15]. Angiogenic factors such as vascular endothelial growth factor (VEGF) [16] and basic fibroblast growth factor [17] have been demonstrated to induce neovascularization of the herniated disc. Johnson et al. [14] showed that IVD aggrecan is inhibitory to endothelial cell migration, but pleiotrophin (PTN) is present in pathologic intervertebral disc tissues and increased levels of pleiotrophin expression may function as an angiogenic factor in stimulating neovascularization of diseased or damaged human IVD [18–20]. PTN is a heparin-binding growth factor with numerous biological activities, most frequently related to the pathological processes of the nervous system and associated with tumor growth and angiogenesis [21]. However, information about associations of PTN with degenerative changes and angiogenesis in IVD is scarce.
Our study was designed to evaluate how much the severity of histodegeneration is related to the development of neovascularization and to the level of pleiotrophin in the herniated lumbar discs.
Methods
Patients and surgical specimen collection
We studied 50 patients (age 24–68 years, mean 40.6 ± 9.9 years) with lumbar IVD herniations (at L3/4 level in one patient, at L4/5 level in 20 patients and at L5/S1 level in 29 patients). Twenty four of the patients were men and 26 were women. All disc specimens were obtained using a standard posterior microdiscectomy approach. Clinical data on the duration of radicular pain were registered. Visual analog scales (VAS), ranging from 0 to 100, were used for assessment of pain (indicating average radicular or lumbar pain in the last 2 days).
Herniations were categorized depending on their relation to the posterior longitudinal ligament (PLL) as contained herniations (CH), i.e., herniations not penetrating through the PLL, and noncontained herniations (NCH), i.e., herniations entering the epidural space. Thus, the CH group included subligamentous disc protrusions or extrusions and the NCH group included transligamentous extrusions or sequestrations. Twenty nine patients had NCH-s (mean age 41.7 ± 9.6 years) and 21 patients had CH-s (mean age 39.1 ± 10.2 years).
The study was approved by the institutional Ethics Review Committee on Human Research.
Tissue processing
The removed specimens were immediately fixed in the buffered 10 % formaline (pH 7.4) for 24 h and subsequently decalcified in 0.5 M EDTA (pH 8.0) over a 6 weeks period at 4 °C. The decalcified specimens were then embedded into paraffin wax. From the resulting tissue blocks, serial 5-μm paraffin sections were cut and placed on glass slides for routine staining: hematoxylin-eosin (H&E), Alcian blue stain with periodic acid-Schiff (Alcian blue-PAS) and Elastica van Gieson using standard histochemical protocols. The specimens were further evaluated qualitatively by an independent pathologist.
Evaluation of histological tissue degeneration
H&E, Alcian blue-PAS and Elastica van Gieson stained sections of the IVD tissue were evaluated for chondrocyte proliferation (0–6 points), mucoid matrix change (0–4), cell death (0–4), tears and clefts formation (0–4) and granular matrix changes (0–4). Briefly, the extent of the degenerative parameter was evaluated and ranked according to the evaluation protocol where zero represented “normal” and higher values indicated increasing severity of degeneration, i.e., mucoid matrix change (mucous degeneration) was estimated as cystic, oval, or irregular homogenous areas with an intense deposition acid mucopolysaccharides staining dark blue with Alcian blue-PAS and quantified as 0 = absent; 1 = rarely present; 2 = present in intermediate amounts of 1–3; 3 = abundantly present [11]; and cell death was assessed as loss of cells and extracellular matrix (0 = absent; 1 = rarely present; 2 = present in intermediate amounts of 1–3; 3 = abundantly present) [11]. For assessment of histological changes in the cartilaginous endplate fragments, ratings for chondrocyte cluster formation (0–4 points), cartilage disorganization (0–4), cracks (0–4), microfractures (0–2), new bone formation (0–2) and bony sclerosis (0–2) were used. The overall histodegeneration score (HDS) for IVD and endplate samples were calculated as described in detail by Boos et al. [11] by adding the scores for each parameter.
Immunohistochemical staining
Immunohistochemical staining was performed with (1) CD34 (DAKO) for endothelial cells to identify the newly formed blood vessels and with (2) anti-human PTN antibody (1:50; Santa Cruz Biotechnology Inc., sc-74443) to detect PTN positive IVD cells. For immunostaining, the sections were deparaffinized and subsequently incubated for antibody retrieval, as indicated by the manufacturers. For detection of neovascularization, the sections were washed and incubated with peroxidase blocking solution and with the specific anti-human monoclonal antibody against the expressed protein. Detection of PTN positive cells was performed in IVD tissue specimens, the tissue sections were incubated with the specific anti-human pleiotrophin antibody at room temperature for 1 h under humid conditions. After several washings, the antigen–antibody complexes were visualized using DAKO REAL™ EnVision Detection System, Peroxidase/DAB+, Rabbit/Mouse. Slides were counterstained with hematoxyline, dehydrated and coverslipped for light microscopy. Neovascularization was assessed using the rating for density of newly formed blood vessels (0–3) [11]: the sections were scored for CD34 postivity by scaling/grading (0 = absent; 1 = sparsely present 2 = present in intermediate amounts of 1–3; 3 = abundantly present). Chondrocyte staining for PTN and the percentage of positively stained cells in IVD tissue samples were determined in five randomly taken high power microscopic fields (×40). Only IVD cells that were clearly pleiotrophin positive were scored.
Data analysis
The continuous data were checked for normality using Shapiro–Wilk’s W test. The severity of histodegenerative changes in different groups was compared with Kruskal–Wallis one-way analysis of variance. Chi-square test was used to compare the differences in proportions for categorical variables (observed levels of neovascularity and detection of PTN positive cells in NCH and CH groups, etc.). One-way analysis of variance was used to compare the means for continuous data. The analyses were performed using the JMP software (version 8.0.1, SAS Institute Inc., Cary, NC, USA). A P value <0.05 was considered statistically significant.
Results
Altogether 29 NCH and 21 CH specimens were studied. The anatomic depiction of the specimens allowed us to evaluate the severity of histodegeneration and neovascularization in the tissue regions presumably representing IVD tissue (nucleus pulposus and anulus fibrosus) and cartilaginous endplate tissue. The NCH specimens included anulus fibrosus in 80 % and nucleus pulposus in 57 % of cases. Almost all the CH specimens included anulus fibrosus (98 %) as well as nucleus pulposus (96 %). Fragments of cartilaginous endplate were found in 17 cases (81 %) of the CH and in 15 cases (52 %) of the NCH specimens.
Histodegenerative changes
All specimens exhibited abundant degenerative signs throughout entire material and the lowest grades corresponding to normal findings were often missing. HDS was 11.3 ± 3.1 in the IVD specimens (maximum possible score: 22 points) and 6.4 ± 3.6 in the endplate samples (maximum possible score: 18 points). The values of HDS did not differ significantly between the NCH and the CH groups (11.1 ± 3.3 vs. 11.5 ± 2.9 in the IVD tissue and 7.5 ± 4.4 vs. 5.5 ± 2.6 in the endplate specimens).
Immunohistochemical findings
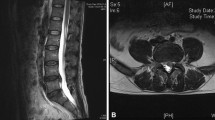
The newly formed blood vessels were present in 94 % of IVD specimens and 84 % of endplate fragments (Fig. 1). The presence of endothelial cells of the blood vessels were confirmed by the positive anti CD34 antibody immunohistochemical stains (Fig. 2a). Higher levels of neovascularization were registered more frequently in the IVD than in the endplate samples (Table 1). Higher levels of disc and endplate neovascularity were registered in the NCH than in the CH samples (Table 1) and the highest level neovascularization was detected significantly more frequently in the NCH group (12 vs. 3 in the IVD specimens and 6 vs. 1 in the endplate fragments; p < 0.05).
Examples of histological degeneration and edge neovascularity in disc tissues (a–c) and cartilaginous endplate (d). a Edge neovascularity level 1: clefts in the degenerated nucleus pulposus tissue (arrow) with few capillaries and slight monocyte infiltration (H&E, ×100). b Edge neovascularity level 2: the specimen consists of degenerative nucleus pulposus with granulation tissue containing capillaries (arrow) and monocyte infiltration (H&E, ×100). c Edge neovascularity level 3: the anulus fibrosus of the intervertebral disc tissue with abundant proliferation of granulation tissue and capillaries (arrow) (H&E, ×100). d A fragment of cartilaginous endplate with level 2 edge neovascularity—abundant capillaries in the granulation tissue (arrow) (H&E, ×100). Bar 200 μm
PTN positive disc cells were detected in 15 of the 42 examined IVD specimens (36 %, Fig. 2b). PTN positive IVD cells were detected in 38 % of NCH and 35 % of CH samples and the frequency of PTN positive disc cells was rather low: 0–22.2 % (mean 3.1 ± 5.3 %). Still, PTN immunoreactivity in the extracellular matrix was registered in most of the IVD specimens (33/42 samples; 79 %).
Relations between immunohistochemical findings and histodegeneration
The level of neovascularization was significantly related to the HDS in the IVD tissues but not in the endplate specimens (Table 2). Both NCH and CH specimens had the highest values of HDS in conjunction with level III neovascularization and the relations between the level of neovascularization and the severity of histodegeneration were significant in the group of NCH-s (Table 2).
Registration or frequency of PTN positive cells did not correlate significantly with HDS or level of neovascularization of the IVD samples.
Relations between histodegenerative changes, immunohistochemical findings and clinical variables
The duration of pain varied largely (from 5 to 360 days) but it was longer in the patients with CH-s (80.6 ± 85.2 vs. 106.7 ± 94.6 days; p = 0.1), and 76.2 % of patients in the CH group as compared to 41.1 % in the NCH group had duration of pain >2 months (p < 0.05). Pain intensity according to VAS was similar in both groups (44.6 ± 14.1 in the CH and 43.3 ± 15.8 in the NCH group).
No significant relations between HDS and patient’s age or duration and intensity of pain were detected.
The intensity of pain was similar in all the levels of IVD neovascularization (level I, 42.8 ± 3.7; level II, 50.0 ± 3.7 and level III. 40.7 ± 3.8) but the duration of pain until the operation was significantly shorter in the group with level III neovascularization of the herniation (level I, 101.3 ± 97.5; level II, 129.1 ± 103.7 and level III, 46.6 ± 22.5). At the same time, the duration and intensity of pain were not significantly related to the levels of endplate neovascularization. The levels of neovascularization were not affected by the age of the patients.
Registration or frequency of PTN positive cells did not correlate significantly with patient’s age or duration and intensity of pain.
Discussion
In this study, we described higher levels of neovascularization in the IVD and endplate herniations that penetrated into the epidural space and showed that the severity of histodegenerative changes is associated with enhanced neovascularization of the disc herniations.
The NCH specimens exhibited more intense edge neovascularity in our study than the CH samples. Our findings are consistent with earlier reports about more enhanced neovascularization in cases of extruded or sequestrated herniations [22]. Infiltration from the venous plexus of the epidural cavity, from the margins of vertebral bodies or from the PLL has been proposed as the origin of the new blood vessels in disc herniations [2, 22]. The pathogenesis of neovascularization can obviously differ depending on the localization of the herniated tissue. In the CH-s, the ingrowth of small blood vessels in the anulus fibrosus may be necessary for reinforced nourishment of the injured disc and indicate the process of repair. In the NCH-s, the vascularized granulation tissue is formed mainly in the margins of the disc tissue and intense accumulation of inflammatory factors is directed to promote the absorption of the tissue [23–25].
We found that the severity of histodegeneration is significantly related to the level of neovascularization in the IVD tissue and especially in cases of the NCH specimens. Several authors have demonstrated that degenerative changes in the disc tissue are related to neovascularization. Karamouzian et al. [5] found that the prevalence of angiogenesis was significantly related to the presence of microscopic calcifications in specimens of herniated nucleus pulposus. Koike et al. [2] described correlation between enhanced angiogenesis and the severity of degeneration as evaluated by optical density of the extracellular matrix of the extruded and sequestrated discs. Peng et al. [8] reported that ingrowth of vascularized granulation tissue occurred along the torn fissures of the disc, the occurrence of which has directly been related to the disc degeneration [26]. Different proteins, collagens and proteoglycan breakdown products may induce angiogenesis at the molecular level [27, 28] and, for instance, strong expression of growth factors has been noted as important regulator of neovascularization as well as disc degeneration [8]. Both IVD degeneration and angiogenesis in the disc tissue have been associated with matrix metalloproteinase (MMP)-1 and MMP-3, tumor necrosis factor (TNF)-a, basic fibroblast growth factor (bFGF), vascular endothelial growth factor (VEGF) and transforming growth factor (TGF)-β [7, 29–31]. It has been suggested that PTN may play a role in neovascularization of diseased or damaged disc tissue [18–20], but we did not find significant relations between IVD neovascularization or histodegeneration and registration of PTN positive IVD cells. According to our results, especially in the CH group, high values of disc degeneration can be found in conjunction with only minor signs of neovascularization. This finding is consistent with Nerlich et al. [12] who did not find vascular invasion deeper than the periphery of the degenerating disc which supported the hypothesis that vascular ingrowth is not a distinct feature of disc degeneration. Boos et al. [11] confirmed that blood vessels can be found only in the outer anulus fibrosus of normal adult discs and did not find neovascularization of the inner parts of the intervertebral discs during disc degeneration. Indeed, Rutges et al. [20] have established that PTN is expressed more in the anulus fibrosus cells of the disk and low frequency of PTN positive cells in our group could be partly explained by the fact that we did not analyze separately anulus fibrosus of the IVD specimens. However, the possible regulation of IVD angiogenesis by PTN deserves further study.
We found that neovascularization of the endplate fragments was also higher in the NCH samples, but significant associations between the severity of endplate degeneration and angiogenesis were not detected. The vertebral endplates form the boundaries of the IVD. Endplate sclerosis is known to play a role in disc degeneration by decreasing nutrient availability to the disc [32]. Our findings are consistent with a previous report by Carreon et al. [4] that cartilage endplate fails to induce neovascularization or diminishes the neovascular response, preventing its degradation. Cartilage endplate, such as articular cartilage, may contain substances that can inhibit neovascularization process [4]. Thus, disc herniations that contain a significant amount of endplate may not be degraded or absorbed and spontaneous remission of the clinical symptoms may be difficult to expect.
We found that the duration of pain was inversely related to the neovascularization level of the herniations. While interpreting these findings, it has to be considered that higher levels of neovascularization were found more often in the NCH group and the sequestrated herniations are more likely to cause serious radicular deficits that might prompt immediate surgical intervention. On the other hand, sequestrated herniations are easier to detect radiologically which might also contribute to the shorter time interval before the operation.
We can conclude that higher levels of disc and endplate neovascularity occur in the NCH group, and severe histodegeneration of lumbar IVD herniations is related to the intense neovascularization and potentially also to the spontaneous regression of the herniated tissue. Our study facilitates the understanding of pathophysiological mechanisms of neovascularization in lumbar disc herniations. More in-depth information about the histologic alterations in lumbar disc degeneration can lead to new opportunities for therapeutic interventions.
References
Kobayashi S, Meir A, Kokubo Y, Uchida K, Takeno K, Miyazaki T, Yayama T, Kubota M, Nomura E, Mwaka E, Baba H (2009) Ultrastructural analysis on lumbar disc herniation using surgical specimens: role of neovascularization and macrophages in hernias. Spine 34(7):655–662
Koike Y, Uzuki M, Kokubun S, Sawai T (2003) Angiogenesis and inflammatory cell infiltration in lumbar disc herniation. Spine 28(17):1928–1933
Pai RR, D’sa B, Raghuveer CV, Kamath A (1999) Neovascularization of nucleus pulposus. A diagnostic feature of intervertebral disc prolapse. Spine 24(8):739–741
Carreon LY, Ito T, Yamada M, Uchiyama S, Takahashi HE (1997) Neovascularization induced by anulus and its inhibition by cartilage endplate. Its role in disc absorption. Spine 22(13):1429–1434
Karamouzian S, Eskandary H, Faramarzee M, Saba M, Safizade H, Ghadipasha M, Malekpoor AR, Ohadi A (2010) Frequency of lumbar intervertebral disc calcification and angiogenesis, and their correlation with clinical, surgical, and magnetic resonance imaging findings. Spine 35(8):881–886
Kato T, Haro H, Komori H, Shinomiya K (2004) Sequential dynamics of inflammatory cytokine, angiogenesis inducing factor and matrix degrading enzymes during spontaneous resorption of the herniated disc. J Orthop Res 22(4):895–900
Matsui Y, Maeda M, Nakagami W, Iwata H (1998) The involvement of matrix metalloproteinases and inflammation in lumbar disc herniation. Spine 23(8):863–869
Peng B, Hao J, Hou S, Wu W, Jiang D, Fu X, Yang Y (2006) Possible pathogenesis of painful intervertebral disc degeneration. Spine 31(5):560–566
Repanti M, Korovessis PG, Stamatakis MV, Spastris P, Kosti P (1998) Evolution of disc degeneration in lumbar spine: a comparative histological study between herniated and postmortem retrieved disc specimens. J Spinal Disord 11(1):41–45
Vernon-Roberts B, Moore RJ, Fraser RD (2007) The natural history of age-related disc degeneration: the pathology and sequelae of tears. Spine 32(25):2797–2804
Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG (2002) Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo award in basic science. Spine 27(23):2631–2644
Nerlich AG, Schaaf R, Wälchli B, Boos N (2007) Temporo-spatial distribution of blood vessels in human lumbar intervertebral discs. Eur Spine J 16(4):547–555
Ikeda T, Nakamura T, Kikuchi T, Umeda S, Senda H, Takagi K (1996) Pathomechanism of spontaneous regression of the herniated lumbar disc: histologic and immunohistochemical study. J Spinal Disord 9(2):136–140
Johnson WE, Caterson B, Eisenstein SM, Roberts S (2005) Human intervertebral disc aggrecan inhibits endothelial cell adhesion and cell migration in vitro. Spine 30(10):1139–1147
Johnson WE, Eisenstein SM, Roberts S (2001) Cell cluster formation in degenerate lumbar intervertebral discs is associated with increased disc cell proliferation. Connect Tissue Res 42(3):197–207
Haro H, Kato T, Komori H, Osada M, Shinomiya K (2002) Vascular endothelial growth factor (VEGF)-induced angiogenesis in herniated disc resorption. J Orthop Res 20(3):409–415
Minamide A, Hashizume H, Yoshida M, Kawakami M, Hayashi N, Tamaki T (1999) Effects of basic fibroblast growth factor on spontaneous resorption of herniated intervertebral discs. An experimental study in the rabbit. Spine 24(10):940–945
Johnson WE, Patterson AM, Eisenstein SM, Roberts S (2007) The presence of pleiotrophin in the human intervertebral disc is associated with increased vascularization: an immunohistologic study. Spine 32(12):1295–1302
Neidlinger-Wilke C, Liedert A, Wuertz K, Buser Z, Rinkler C, Käfer W, Ignatius A, Claes L, Roberts S, Johnson WE (2009) Mechanical stimulation alters pleiotrophin and aggrecan expression by human intervertebral disc cells and influences their capacity to stimulate endothelial migration. Spine 34(7):663–669
Rutges J, Creemers LB, Dhert W, Milz S, Sakai D, Mochida J, Alini M, Grad S (2010) Variations in gene and protein expression in human nucleus pulposus in comparison with annulus fibrosus and cartilage cells: potential associations with aging and degeneration. Osteoarthr Cartil 18(3):416–423
Papadimitriou E, Mikelis C, Lampropoulou E, Koutsioumpa M, Theochari K, Tsirmoula S, Theodoropoulou C, Lamprou M, Sfaelou E, Vourtsis D, Boudouris P (2009) Roles of pleiotrophin in tumor growth and angiogenesis. Eur Cytokine Netw 20(4):180–190
Ozaki S, Muro T, Ito S, Mizushima M (1999) Neovascularization of the outermost area of herniated lumbar intervertebral discs. J Orthop Sci 4(4):286–292
Haro H, Shinomiya K, Komori H, Okawa A, Saito I, Miyasaka N, Furuya K (1996) Upregulated expression of chemokines in herniated nucleus pulposus resorption. Spine 21(14):1647–1652
Kikuchi T, Nakamura T, Ikeda T, Ogata H, Takagi K (1998) Monocyte chemoattractant protein-1 in the intervertebral disc. A histologic experimental model. Spine 23(10):1091–1099
Rothoerl RD, Woertgen C, Holzschuh M, Rueschoff J, Brawanski A (1998) Is there a clinical correlate to the histologic evidence of inflammation in herniated lumbar disc tissue? Spine 23(11):1197–1200
Osti OL, Vernon-Roberts B, Moore R, Fraser RD (1992) Annular tears and disc degeneration in the lumbar spine. A post-mortem study of 135 discs. J Bone Jt Surg Br 74(5):678–682
Koch AE, Nickoloff BJ, Holgersson J, Seed B, Haines GK, Burrows JC, Leibovich SJ (1994) 4A11, a monoclonal antibody recognizing a novel antigen expressed on aberrant vascular endothelium. Upregulation in an in vivo model of contact dermatitis. Am J Pathol 144(2):244–259
Thornalley PJ (1998) Cell activation by glycated proteins. AGE receptors, receptor recognition factors and functional classification of AGEs. Cell Mol Biol (Noisy-le-grand) 44:1013–1023
Tolonen J, Grönblad M, Virri J, Seitsalo S, Rytömaa T, Karaharju E (2001) Transforming growth factor beta receptor induction in herniated intervertebral disc tissue: an immunohistochemical study. Eur Spine J 10(2):172–176
Kokubo Y, Uchida K, Kobayashi S, Yayama T, Sato R, Nakajima H, Takamura T, Mwaka E, Orwotho N, Bangirana A, Baba H (2008) Herniated and spondylotic intervertebral discs of the human cervical spine: histological and immunohistological findings in 500 en bloc surgical samples. Laboratory investigation. J Neurosurg Spine 9(3):285–295
Zigouris A, Batistatou A, Alexiou GA, Pachatouridis D, Mihos E, Drosos D, Fotakopoulos G, Doukas M, Voulgaris S, Kyritsis AP (2011) Correlation of matrix metalloproteinases-1 and -3 with patient age and grade of lumbar disc herniation. J Neurosurg Spine 14(2):268–272
Gruber HE, Ashraf N, Kilburn J, Williams C, Norton HJ, Gordon BE, Hanley EN Jr (2005) Vertebral endplate architecture and vascularization: application of micro-computerized tomography, a vascular tracer, and immunocytochemistry in analyses of disc degeneration in the aging sand rat. Spine 30(23):2593–2600
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rätsep, T., Minajeva, A. & Asser, T. Relationship between neovascularization and degenerative changes in herniated lumbar intervertebral discs. Eur Spine J 22, 2474–2480 (2013). https://doi.org/10.1007/s00586-013-2842-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2842-1