Abstract
Purpose
Construct subsidence is a relatively common complication following anterior cervical fusion. Its occurrence has been revealed to be closely related to endplate-implant contact interface. But current literature focusing on the anatomy of cervical endplate is very scarce. The purpose of this morphometric study was to analyse the sagittal geometry, especially the concavity and slope, of vertebral endplates from C3 to C7 by employing data from CT scans.
Methods
Reformatted CT scans of 97 individuals were analyzed and endplate concavity depth, endplate concavity apex location, as well as endplate slope were measured in midsagittal plane. Those specific parameters were compared among different age and gender groups. Meanwhile, comparison between superior and inferior endplate of each vertebra was also performed.
Results
Age and gender did not influence endplate concavity depth, endplate concavity apex location, or endplate slope significantly (P > 0.05). Endplate concavity depths of superior endplates (range 0.9–1.2 mm) were significantly smaller than those of inferior endplates (range 2.1–2.7 mm). Endplate concavity apex was always located in the posterior half of the endplate, with the superior one ranged from 56 to 67 % and the inferior one 52 to 57 %. Average endplate slopes of superior endplates were between 4.5° and 9.0°, and average inferior endplate slopes ranged from 4.5° to 7.5°. Among all measured segments, C5 had the largest endplate slope values, while C7 the least.
Conclusions
Superior endplate is more flat than its inferior counterpart in middle and lower cervical spine, and the concavity apex is always located in the posterior half of the endplate. Endplate slope is correlated with cervical curvature, greater slope implying more significant lordosis. These sagittal endplate geometrical parameters should be taken into consideration when investigating implant subsidence following anterior cervical fusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anterior cervical fusion is a time tested surgical technique for treatment of various spinal pathologies of the middle and lower cervical spine (C3–C7) [1, 2]. The main goals of this procedure include complete neural elements decompression, sagittal balance correction, as well as cervical spine stabilization. Among those objectives, the first one could be achieved through careful and dedicate intraoperative manipulation, while to meet the needs of the latter two, both meticulous operation and well-designed implant are indispensable. However, despite of continuous improvements of both surgical techniques and implants, some postoperative complications still occur and cause long-term morbidity. Among them, subsidence of the implant into the vertebral endplate is relatively common and leads to gradual loss of anterior column height and cervical lordosis, loss of foraminal height, neuroforaminal stenosis, and recurrence of radiculopathy [3–5].
Because of the detrimental effect of subsidence, extensive researches have been carried out to find out its cause and potential mechanism [6, 7]. Recent studies have demonstrated the multifactorial nature of the subsidence genesis and the importance of the endplate-implant contact interface in that process [8–10]. Since then, biomechanical characteristics of the cervical endplate have drawn a lot of attentions. However, quite a few reports concerning quantitative anatomic data of the cervical endplate are available, and no study has investigated the sagittal endplate concavity in this region [11, 12].
The purpose of this study was to analyse the sagittal geometry, especially the concavity and slope of vertebral endplates from C3 to C7 by employing processed data from digitized CT scans. These messages were used to provide an accurate geometric description of the individual endplates from a different point of view.
Materials and methods
Subjects
Ninty-seven Patients (average age 41 years, range 25–51 years) that underwent a cervical CT scans (LightSpeed VCT, GE Healthcare, London, UK) were retrospectively selected from the Picture Archiving and Communication System (PACS). All those participants were scanned for head and neck symptoms and complained of no spinal problems. Exclusion criteria included marked osteophyte formation, significant vertebral degeneration, vertebral fracture, and neoplasms involving vertebral body on CT scans. Vertebrae with a visual axial rotation with respect to the axis of the scanner and vertebral columns with a large lateral slant were also excluded. According to the age (>40 years or not) and gender, those patients were divided into four groups (A1, A2, B1, B2). There were 22, 26, 28, 21 subjects in each group, respectively.
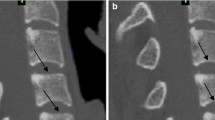
Images
CT scan parameters were as follows: field of view 180 mm, matrix 512*512, slice thickness 0.625 mm, and pitch 1.375:1. Window settings for measurements were as follows: width 1,800 Housefield units (HU) and center 700 HU. All the CT scan images have been multi-planar reformatted and geometric parameters were measured on midsagittal plane (MSP), which is defined as the image in which the complete contour of corresponding vertebral spinous process could be observed.
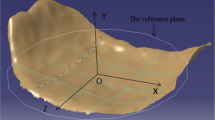
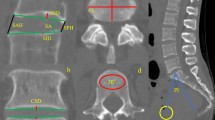
Measurements
Anatomic landmarks, including anterior (A) and posterior (P) rims of the endplate, the concavity apex points (Ca), as well as superior (S) and inferior (I) rims of the anterior wall of the vertebral body on the MSP, were marked manually using the internal measuring instrumentation of the PACS by a trained user (CH). The AP line represents the orientation of endplates, while the SI line stands for the direction of the anterior wall of the vertebral body. Subsequently, by employing the same software required angles and distances were measured. In drawing the perpendicular line from Ca to AP, one could get a point (C’) on the AP line, which could be regarded as the projective point of Ca in AP and be helpful in determining the location of the endplate concavity apex in the MSP. The following parameters were subsequently measured: (1) Endplate concavity depth (ECD), which measured the length of CaC’; (2) Endplate concavity apex (ECA) location, represented as the length of AC’ divided by the length of AP; (3) Endplate slope (ES), firstly measuring the angle formed by the AP and SI line, then subtracting that value from 90° (Figs. 1, 2, 3).
Schematic illustration of the measurement of superior endplate slope: first locate vertebral landmarks including anterior (A), posterior (P), superior (S), and inferior (I) rim of vertebral body, then connect points A, P as well as S, I, measure the angle formed by the AP and SI line, then subtract that value from 90°
Statistics
Statistical evaluation was performed with SPSS software version 16.0 (SPSS Inc, Chicago, IL, USA). Descriptive statistics (means and standard deviations) were obtained for quantitative variables. One-way analysis of variance (one-way ANOVA) and independent samples student t tests were employed for data analysis. The significance level was set at P < 0.05.
Results
Endplate concavity depth
No significant difference has been revealed among four groups (the least P = 0.34). As demonstrated in Table 1, for all participants, superior ECD values from C3 to C7 were between 0.9 and 1.2 mm, while inferior ECD values were between 2.1 and 2.7 mm, both demonstrating significant difference (the largest P < 0.00001). The superior ECDs were significantly smaller than its counterparts (the largest P < 0.00001), suggesting a more even geometry on the upper side of the cervical vertebral body.
Endplate concavity apex location
The inferior endplate concavity apex point could be identified with ease; however, its superior counterpart was obscure and indistinct due to the relatively flat nature of the upper vertebral endplate.
Age and gender showed no significant influence on ECA location (the least P = 0.42). In general, the ECA was always located in the posterior half of the endplate, with the superior one ranged from 56 to 67 % and the inferior one 52–57 % (See Table 2).
Endplate slope
Age and gender did not influence ES significantly (the least P = 0.054). For each vertebra, no significant difference has been found between its superior and inferior endplates except C5 (9.0° vs. 7.5°), suggesting parallelity of endplates within those segments. Overall, average ESs of superior endplates were between 4.5° and 9.0°, and average inferior ES values ranged from 4.5° to 7.5°. Among all measured segments, C5 had the largest ES values, while C7 the least (C5 superior 9.0°, C5 inferior 7.5°; C7 superior 4.5°, C7 inferior 4.5°). These data demonstrated the variability of endplate orientation in middle and lower cervical spine (See Table 3).
Discussion
Subsidence of constructs into the vertebral body is a well-known complication following anterior cervical fusion. A small degree of subsidence may provide some benefits, including immediate stability of the instrumentation and promotion of biologic fusion. However, when aggravated, it can result in loss of segmental lordosis and anterior column support, progressive deformity, and failure of anterior instrumentation [3–5]. Previously, its occurrence has been attributed to the implants’ material property such as modulus of elasticity [6, 7]. However, recent studies have revealed that this complication was mainly caused by the limited contact area between construct and endplate, which leaded to point loading at the construct-endplate interface [8–10].
It seems reasonable that, to acquire better primary implant stability, a small degree of subsidence is acceptable; thus some mismatch in the construct-endplate interface is beneficial. This may be especially true for cervical disc replacement, since its primary stability depends on the press-fit mechanism of artificial disc. However, the problem is no one could predict the extent of subsidence that would occur postoperatively. So, from a conservative point of view, the authors think the best solution is to prevent it from happening as possible as one can. Besides, with respect to cervical disc replacement, device subsidence has already been reported as a postoperative complication, suggesting that long-term stability is still an issue of concern with current press-fit technique [13]. Taken together, the authors believe that the avoidance of implant subsidence is of great importance.
The vertebral endplate is a thin layer of dense, subchondral bone adjacent to the intervertebral disc, which tends to be thinnest in the central region and thickest toward the periphery [14]. Based on the results of former studies, the surface shape of endplate is not totally flat, but rather approximates an arch, with the central area somewhat depressed [15–17]. However, in contrast to the morphological complexity of vertebral endplates, the endplate designs of anterior cervical fusion devices are significantly simplified, i.e, the sagittal profile of most currently available anterior cervical fusion constructs is limited to flat endplate or at the best minor convexity with some modularity of the slope angle. This oversimplification of the design would be doomed to bring about insufficient contact area between device and endplate, finally resulting in subsidence of construct.
One may argue that the construct-endplate interface conformity could be achieved through removal of peripheral region of endplate to make the contact surface flat and even. Nevertheless, this option is assumed to weaken the compressive strength of the vertebral body. Rockoff et al. [18] have reported that the endplate contributes 45–75 % of the peak strength of the vertebral body during compressive loading. Meanwhile, a recent investigation has revealed that the complete removal of the endplate could decrease nearly 39 % of compressive strength, and the central region of the endplate was the weakest portion, being 38 % weaker than the posterolateral position, indicating the importance of preserving the periphery area during endplate preparation from a biomechanical point of view [19]. Therefore, to solve the construct-endplate mismatch issue, it is indispensable to take the endplate morphology into consideration when designing the interbody construct. Since sagittal morphology of endplate is significantly variable and common morphological parameters have not yet been clearly identified, precise investigation of the shape and geometry of endplates of the middle and lower cervical spine, which is the common surgical site of anterior cervical fusion, is necessary.
The impact of age on the endplate concavity is controversial due to its complex nature. On one hand, osteoporosis, which usually starts in the fourth decade of life, would result in apparent or non-apparent vertebral fractures and deformity of vertebral body, leading to endplate concavity alteration. It has been reported that increased endplate concavity is always found with a loss of bone mineral density [20], suggesting that in elderly people, especially elderly women, the ECD would progressively increase. Recently, van der Houwen et al. [17] also showed that the ECD increased about 0.01 mm per year, suggesting an increasing endplate concavity along with growing age. However, others have found the tendency of decreasing concavity with osteoporosis [21]. So, there is still no consensus on the effect of osteoporosis on endplate concavity. On the other hand, spinal degeneration, which frequently occurs at cervical and lumbar spine, gradually occurs with aging and usually accelerates after 40 years of age. It would lead to changes of mechanical loading conditions and may also exert influences on endplate concavity. Miao et al. [22] have suggested that the lumbar degeneration is a correlator of lumbar endplate concavity, indicating less concavity along with more advanced degeneration. This finding has been confirmed by another research group who has found that lumbar vertebral endplate concave angle is positively related to the severity of lumbar degeneration [23]. In the current study, no significant differences of ECD have been revealed among each age group, suggesting age itself may not be an independent determinant of endplate concavity. Rather, it’s the bone mineral density or degeneration which plays the decisive role. Unfortunately, neither the bone mineral density value nor the extent of cervical degeneration of the participants in this study was evaluated, making it impossible to explore the relationship between those two parameters and concavity.
It was demonstrated in the present study that C5 had the largest ES value, while this very value of C7 was the least. Considering the fact that C5 is located at the apex of cervical lordosis whereas C7 is situated in the cervicothoracic junction, which is the transition region from lordosis to kyphosis, we consider cervical ES to be an important factor maintaining cervical lordosis. The larger the ES value, the more significant the curvature. Spinal curvature is of great importance when performing anterior fusion because if sagittal spinal alignment could not be restored postoperatively, asymmetric loading of the endplate may occur and finally cause subsidence and many other problems. In fact, some newly designed modular interbody fusion systems are combined with self-adjusting or angled endplates to get a better adaptation to the local anatomy [24, 25]. However, direct evaluation of this parameter in the cervical spine is quite sparse. More sophisticated studies are needed to investigate detailed correlations between ES and spinal curvature.
One significant limitation of this study is that only the midsagittal plane has been measured and analyzed. The data obtained is far from enough to be employed in implant design and modification. Nevertheless, these results could provide some preliminary information of the middle and lower cervical endplate geometry and assist in more sophisticated morphological study in the future. The second limitation is that only “normal subjects” are enrolled, thus lacking a comparative group representing patients with degenerative cervical diseases. As aforementioned, the relationship between degeneration and endplate concavity is still not clear, and further studies are needed to acquire better understanding.
Conclusions
In general, superior endplate is more flat than its inferior counterpart in middle and lower cervical spine, and the concavity apex is always located in the posterior half of the endplate. Endplate slope is correlated with cervical curvature, greater slope implying more significant lordosis. These sagittal endplate geometrical parameters should be taken into consideration when investigating implant subsidence following anterior cervical fusion.
References
Bohlman HH, Emery SE, Goodfellow DB, Jones PK (1993) Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am 75:1298–1307
Emery SE, Bolesta MJ, Banks MA, Jones PK (1994) Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine 19:660–663
van Jonbergen HP, Spruit M, Anderson PG, Pavlov PW (2005) Anterior cervical interbody fusion with a titanium box cage: early radiological assessment of fusion and subsidence. Spine J 5:645–649 discussion 649
Kao FC, Niu CC, Chen LH, Lai PL, Chen WJ (2005) Maintenance of interbody space in one- and two-level anterior cervical interbody fusion: comparison of the effectiveness of autograft, allograft, and cage. Clin Orthopaed Relat Res 430:108–116
Grob D, Daehn S, Mannion AF (2005) Titanium mesh cages (TMC) in spine surgery. Eur Spine J 14:211–221
Chou YC, Chen DC, Hsieh WA, Chen WF, Yen PS, Harnod T, Chiou TL, Chang YL, Su CF, Lin SZ, Chen SY (2008) Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci 15:1240–1245
Niu CC, Liao JC, Chen WJ, Chen LH (2012) Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech 23:310–316
Barsa P, Suchomel P (2007) Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J 16:1395–1400
Cabraja M, Oezdemir S, Koeppen D, Kroppenstedt S (2012) Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord 13:172
Buttermann GR, Beaubien BP, Freeman AL, Stoll JE, Chappuis JL (2009) Interbody device endplate engagement effects on motion segment biomechanics. Spine J 9:564–573
Kim MK, Kwak DS, Park CK, Park SH, Oh SM, Lee SW, Han SH (2007) Quantitative anatomy of the endplate of the middle and lower cervical vertebrae in Koreans. Spine 32:E376–E381
Tan SH, Teo EC, Chua HC (2004) Quantitative three-dimensional anatomy of cervical, thoracic and lumbar vertebrae of Chinese Singaporeans. Eur Spine J 13:137–146
Van Ooij A, Oner F, Verbout A (2003) Complications of artificial disc replacement: a report of 27 patients with the SB Charite disc. J Spinal Disord Tech 16:369–383
Edwards WT, Zheng Y, Ferrara LA, Yuan HA (2001) Structural features and thickness of the vertebral cortex in the thoracolumbar spine. Spine 26:218–225
Lakshmanan P, Purushothaman B, Dvorak V, Schratt W, Thambiraj S, Boszczyk M (2012) Sagittal endplate morphology of the lower lumbar spine. Eur Spine J Suppl 2:S160–S164
Chen H, Jiang D, Ou Y, Zhong J, Lv F (2011) Geometry of thoracolumbar vertebral endplates of the human spine. Eur Spine J 20:1814–1820
van der Houwen EB, Baron P, Veldhuizen AG, Burgerhof JG, van Ooijen PM, Verkerke GJ (2010) Geometry of the intervertebral volume and vertebral endplates of the human spine. Ann Biomed Eng 38:33–40
Rockoff SD, Sweet E, Bleustein J (1969) The relative contribution of trabecular and cortical bone to the strength of human lumbar vertebrae. Calcif Tissue Res 3:163–175
Lowe TG, Hashim S, Wilson LA, O’Brien MF, Smith DA, Diekmann MJ, Trommeter J (2004) A biomechanical study of regional endplate strength and cage morphology as it relates to structural interbody support. Spine 29:2389–2394
Twomey LT, Taylor JR (1987) Age changes in lumbar vertebrae and intervertebral discs. Clin Orthop Relat Res 224:97–104
Ferguson SJ, Steffen T (2003) Biomechanics of the aging spine. Eur Spine J Suppl 2:S97–S103
Miao S, Sha GZ, Wang YD, Yan LQ, Song LY, Guo Z, Fan L, Shao L (2008) Imageology change of degenerative cartilage endplate to different degree and its clinical significance. Zhongguo Gu Shang 21:414–417
He X, Liang A, Gao W, Peng Y, Zhang L, Liang G, Huang D (2012) The relationship between concave angle of vertebral endplate and lumbar intervertebral disc degeneration. Spine 37:E1068–E1073
Buttermann GR, Freeman AL, Beaubien BP (2010) In vitro biomechanics of an expandable vertebral body replacement with self-adjusting end plates. Spine J 10:1024–1031
Pflugmacher R, Schleicher P, Schaefer J, Scholz M, Ludwig K, Khodadadyan-Klostermann C, Haas NP, Kandziora F (2004) Biomechanical comparison of expandable cages for vertebral body replacement in the thoracolumbar spine. Spine 29:1413–1419
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, H., Zhong, J., Tan, J. et al. Sagittal geometry of the middle and lower cervical endplates. Eur Spine J 22, 1570–1575 (2013). https://doi.org/10.1007/s00586-013-2791-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2791-8