Abstract
Anterior cervical decompression and fusion with anterior plating of the cervical spine is a well-accepted treatment for cervical radiculopathy. Recently, to minimise the extent of surgery, anterior interbody fusion with cages has become more common. While there are numerous reports on the primary stabilising effects of the different cervical cages, little is known about the subsidence behaviour of such cages in vivo. We retrospectively reviewed eight patients with cervical radiculopathy operated upon with anterior discectomy and fusion with a stand-alone titanium cervical cage. During surgery, only the cartilage portion of the end plate was removed and the cages were filled with autologous cancellous bone graft from the iliac crest. To assess possible subsidence or migration, three different radiographic measurements in the sagittal plane were taken for each case, postoperatively and at the latest follow-up. Subsidence was defined as any change in at least one of our parameters of at least 3 mm. Follow-up time was 12–18 months (average 15 months). Five of the nine fused levels had radiological signs of cage subsidence. No posterior or anterior migration was observed. However, subsidence did not correlate with clinical symptoms in four of the five patients. The remaining patient with signs of subsidence, whose neck pain and neurologic symptoms had regressed in the early postoperative course, suffered recurrence of radiculopathy 6 months after the surgery. Her symptoms were explained by the subsidence of the cage and the subsequent foraminal stenosis observed on the magnetic resonance imaging (MRI) scan. At 15 months' follow-up, her cage was broken. Our preliminary results, so far limited in number, represent a serious warning to the proponents of stand-alone cervical cages
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, Van Limbeck et al., in a systematic literature review, failed to identify the best method for a single-level anterior cervical interbody fusion [13]. With the introduction of different interbody fusion devices, such as cages, surgical strategies to achieve anterior cervical fusion have evolved. The first papers on such promising techniques have been published [4, 7, 10, 14]. However, Wigfield, in a thorough literature review, concluded that there was limited evidence supporting the use of a cervical interbody fusion device in place of autologous bone [15].
We therefore reviewed our first cases of stand-alone cervical cages with a specific emphasis on the subsidence behaviour of such cages. This was prompted by a clinical impression of settling of the implants during the follow-up of our patients
Materials and methods
We conducted a retrospective review of the first eight patients that we operated on with a stand-alone cervical cage. All patients initially presented with a cervical radiculopathy and concordant soft disc herniation that had persisted despite conservative management. Anterior discectomy and stand-alone cervical cage interbody fusion were performed in the C5-C6 segment in three cases and in the C6-C7 segment in six cases, using the same technique (one patient had a two-level cage insertion). Two independent observers reviewed hospital charts, operative reports and all radiographs. Follow-up time ranged from 12 to 18 months (average 15 months). The age of the patients ranged from 33 to 61 years (average age 43 years). Seven patients were male and one female.
Surgical technique
All patients were operated according to the same standardised technique. After insertion of a cervical spine distractor, a complete discectomy and a neural decompression were performed. Great care was taken to avoid damaging the cortical structures of the bony end plates. Using cage trials under fluoroscopy, the appropriate size of cage was assessed. The cage was then filled with cancellous bone from the anterior iliac crest that was harvested through a mini-incision. A standard convex SynCage-C anterior cervical interbody fusion implant (Synthes USA, Paoli, Pa., USA; Fig. 1) was then inserted under fluoroscopy for an exact placement, the cervical distractor was then removed and the cage tested for stability. Additional bone graft was applied in front of the cage. Patients were kept in a soft collar for 4–6 weeks.
Cervical cage used in the study. The Syncage-C has a porous shaped box design with a superior and inferior central opening. The inferior opening is larger than the superior one, as it is used to fill the cage with cancellous bone. The two central openings permit bony ingrowth into and from the adjacent end plate, allowing the fusion to take place. The superior aspect of the cage is convex, the inferior aspect straight, to match the anatomy of the inferior and superior end plate of the cervical vertebra
Radiological evaluation
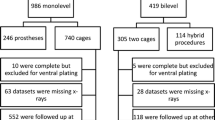
Plain radiographs in anterior-posterior and lateral views were performed postoperatively before discharge and at the different follow-ups. In order to assess subsidence or migration, three different measurements on the lateral radiographs were taken for each case, postoperatively and at the latest follow-up (see Fig. 2, Table 1). Subsidence was defined as any change in at least one of our parameters of 3 mm or more. When settling was present, it was then characterised as a superior migration, an inferior migration or a bi-directional migration. Segmental kyphosis or lordosis was measured by the angle between the upper and lower adjacent end plate line. Functional cervical radiographs in flexion and extension were used to assess segmental cervical motion. We assumed that stability was present if the difference on the flexion and extension radiographs was not greater than 2°.
Results
There were no intra- or postoperative complications. Neurologic symptoms regressed initially in all patients.
Radiologically, only three patients out of the eight studied (or four cages out of the nine inserted) did not show any change in the studied parameters (Table 1, Fig. 3).
A change in at least one of our defined radiological parameters of at least 3 mm was observed in five of nine segments (Table 1, Fig. 4). There was no case of anterior or posterior migration of the cage. Superior migration of the cage into the superior end plate was obvious on the lateral radiographs in two cases. Inferior cage migration into the inferior end plate was observed in two patients. Simultaneous superior and inferior end plate migration was observed in two cases. All the patients had functional radiographic evaluation, and no segmental motion or kyphosis was observed in any of these cases.
At the last follow-up, one patient had recurrence of her radiculopathy. This latter patient (patient 7) had experienced an initial regression of her neck pain and C7 radiculopathy following surgery, but her symptoms recurred again 6 months later. An obvious reduction of the intervertebral space with subsidence of the cage was observed on plain radiographs, and at 15 months' follow-up one could notice a fracture of the cage (Fig. 5). The patient required revision, removal of the cage, further cervical decompression, iliac crest bone graft and anterior plating.
Same patient as in Fig. 4. At 15 months' follow-up the cage is broken (left). Right Aspect of the cage during its retrieval
Discussion
Uninstrumented fusion with graft shows collapse, extrusion or resorption, followed by neural compression, instability and pseudarthrosis [1]. To reduce these problems, anterior plating has been used in the past. In a recent meta-analysis by Floyd and Ohnmeiss, anterior cervical fusion with autograft was found to be superior to allograft as far as pseudarthrosis and disc space collapse were concerned [3]. More recently, reports have claimed advantages of stand-alone cervical cages over classic autologous bone graft with or without anterior plating [4, 7, 10, 14]. However, strong evidence of the superiority of cages is missing. Wigfield and Nelson claimed there was very little evidence to justify their use [15]. Vavruch et al., in a prospective randomised study comparing the Cloward procedure and a carbon-fibre cage, concluded that the clinical outcomes were similar, the anatomic alignment was better with cages, but the fusion rate was much higher with the Cloward procedure (86%) than with the carbon-fibre cages (62%) [14].
Our results demonstrated subsidence in five out of nine cages measured by a decrease in the disc space narrowing of at least 3 mm. One of the nine cages broke during the follow-up period. Our series, though small as yet, is very alarming, and we assume that subsidence in cervical stand-alone interbody cage fusion is a major problem and additional stabilisation is necessary to avoid this problem, as has already been reported in vitro [8, 11, 12].
The causes of subsidence may stem from the instability created by the discectomy, the postoperative cervical motion, the cage design, the end plate preparation, or the bone mineral density [2, 5, 6, 9, 16]. At any rate, subsidence is not classically observed after anterior cervical fusion with a plate.
Does cage subsidence or pseudarthrosis really matter clinically? In the study by Vavruch et al., the carbon-fibre cage group did as well as the group with the classic Cloward procedure, but the pseudarthrosis rate of their cage group (38%) is, to our mind, unacceptable in the long run [14]. Their exact rate and quantification of subsidence remains unknown.
Conclusions
The results of this small series of homogeneous patients, with the high incidence of cage subsidence and one cage breakage, indicates the need for caution with the use of stand-alone titanium cervical cages in anterior cervical surgery. We felt that, ethically, we could not continue using stand-alone cervical cages without the addition of anterior cervical plating. The subsidence that we observed does not seem to be specific to the particular cage design that we used, as other studies have significant subsidence with other cages, at least in vitro. This paper should represent a serious warning to those who want to use stand-alone cervical cages.
References
Cahil CW, Sonstein WS (1999) Anterior cervical instrumentation. Tech Neurosurg 5:133–145
Curylo LJ, Lindsey RW, Doherty BJ, LeBlanc A (1996) Segmental variations of bone mineral density in the cervical spine. Spine 21:319–322
Floyd T, Ohnmeiss D (2000) A meta-analysis of autograft versus allograft in anterior cervical fusion. Eur Spine J 9:398–403
Hacker RJ (2000) A randomized prospective study of an anterior cervical interbody fusion device with a minimum of 2 years of follow-up results. J Neurosurg 93 [2 Suppl]:222–226
Hollowell JP, Vollmer DG, Wilson CR, Pintar FA, Yoganandan N (1996) Biomechanical analysis of thoracolumbar interbody constructs: how important is the endplate? Spine 21:1032–1036
Kettler A, Wilke HJ, Claes L (2001) Effects of neck movements on stability and subsidence in cervical interbody fusion: an in vitro study. J Neurosurg 94 [1 Suppl]:97–107
Matge G, Leclercq TA (2000) Rationale for interbody fusion with threaded titanium cages at cervical and lumbar levels. Results on 357 cases. Acta Neurochir 142:425–433
Oxland TR, Lund T (2000) Biomechanics of stand-alone cages and cages in combination with posterior fixation: a literature review. Eur Spine J 9 [Suppl 1]:95–101
Panjabi MM, White AA, Johnson RM (1975) Cervical spine mechanics as a function of transection of components. J Biomech 8:327–336
Profeta G, de Falco R, Ianniciello G, Profeta L, Cigliano A, Raja AI (2000) Preliminary experience with anterior cervical microdiscectomy and interbody titanium cage fusion (Novus CT-Ti) in patients with cervical disc disease. Surg Neurol 53:417–426
Shimamoto N, Cunningham BW, Dmitriev AE, Minami A, McAfee PC (2001) Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine. Spine 26:E432–436
Shono Y, McAfee PC, Cunningham BW, Brantigan JW (1993) A biomechanical analysis of decompression and reconstruction methods in the cervical spine. Emphasis on a carbon-fiber-composite cage. J Bone Joint Surg Am 75:1674–1684
van Limbeek J, Jacobs WC, Anderson PG, Pavlov PW (2000) A systematic literature review to identify the best method for a single level anterior cervical interbody fusion. Eur Spine J 9:129–136
Vavruch L, Hedlung R, Javid D, Leszniewski W, Shalabi A (2002) A prospective randomized comparison between the Cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiologic study. Spine 27:1694–1701
Wigfield CC, Nelson RJ (2001) Non autologous interbody fusion materials in cervical spine surgery: how strong is the evidence to justify their use? Spine 26:687–694
Wilke HJ, Kettler A, Goetz C, Claes L (2000) Subsidence resulting from simulated postoperative neck movements: an in vitro investigation with a new cervical fusion cage. Spine 25:2762–2770
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gercek, E., Arlet, V., Delisle, J. et al. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12, 513–516 (2003). https://doi.org/10.1007/s00586-003-0539-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-003-0539-6