Abstract
To avoid complications associated with plating in anterior cervical discectomy and fusion (ACDF), stand-alone anchored PEEK cage was developed and favourable outcomes with a low rate of dysphasia have been described. The objective of this study was to compare the clinical and radiological outcomes of ACDF using a standalone anchored PEEK cage (PREVAIL; Medtronic Sofamor Danek, Memphis, TN) with those of a PEEK cage with plating in a prospective randomized manner. Fifty patients with single-level cervical radiculopathy were randomly assigned to a PREVAIL or a PEEK cage with plating. Following 3, 6, 12, and 24 months, clinical and radiological outcomes were assessed. The mean surgical time for the patients with a PREVAIL was significantly shorter than that for those with a PEEK cage with plating. The clinical outcomes evaluated by visual analogue scale for pain and the Odom’s criteria were comparable between both the groups. Both the groups demonstrated the high fusion rate (92 % in PREVAIL; 96 % in PEEK cage with plating). The subsidence rate and the improvement of cervical alignment were comparable between both the groups. The incidence of adjacent-level ossification was significantly lower for patients with a PREVAIL than that for those with a PEEK cage with plating. The rate of dysphasia graded by the method of Bazaz and measurement of prevertebral soft tissue swelling indicated no significant differences between both the groups. Our prospective randomized study confirmed that stand-alone anchored PEEK cage is a valid alternative to plating in ACDF with a low rate of adjacent-level ossification. However, the potential to reduce the incidence of dysphasia was not confirmed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative cervical disease is a major cause of radicular arm pain with or without neurologic deficits. When non-operative treatment fails, surgery may be considered. Anterior cervical discectomy and fusion (ACDF) is one of the surgical procedures of choice for the treatment of cervical radiculopathy. Autogenous iliac crest bone graft (AICG) for ACDF has been considered the “gold standard” treatment option for decades. Although AICG is highly effective procedure, numerous complications such as chronic pain, haematomas, infections, iliac crest fractures, and unsightly scars have been reported [1–3]. To prevent these complications, allografts and synthetic interbody cages have been developed as a substitute for AICG. The other clinical consideration is the advantage of anterior plating. Many surgeons prefer to add an anterior plate in fusion procedures for enhancing stabilizing properties, as several studies suggest that this leads to increased fusion rates [4–6].
The addition of a plate is, however, not without side effects. Although the profile of current anterior plate is thinner than that of earlier designs, 2–67 % of the patients may complain of dysphasia in the early post-operative period [7, 8]. Most of these symptoms disappear during the first 3 months after surgery. The incidence of chronic dysphasia-related symptoms after ACDF ranges from 3 to 21 % in the current literature [9–11], whereas the pathophysiologic cause still remains unclear. Additionally, implant-related mechanical complications have been reported in a recent literature review [12].
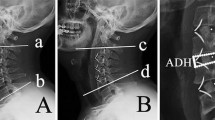
Based on these results, stand-alone anchored cage was developed to potentially avoid complications associated with anterior plating. The PREVAIL (Medtronic Sofamor Danek, Memphis, TN) is a stand-alone cervical fusion implant that involves an internal screw fixation and a zero-step locking mechanism that eliminates the need for external supplemental fixation. It is made of polyetheretherketone (PEEK) spacer with an anterior flange, and screw fixation is provided by two 3.5-mm-diameter screws inserted midline, one above and one below (Fig. 1). While several recent data described the effectiveness of stand-alone anchored PEEK cage with satisfactory clinical and radiological outcomes [13–15], most of these studies have been retrospective with a short-term follow-up. Therefore, the objective of this study was to confirm the efficacy of the PREVAIL by comparing to the plate fixation with a PEEK cage in a prospective randomized manner at a 2-year follow-up.
Materials and methods
We enroled 50 patients with single-level cervical radiculopathy presenting with chronic neck pain and irradiating upper extremity symptoms. All patients were randomly assigned to ACDF using a PREVAIL (PREVAIL group) or ACDF enhanced by plating using a PEEK cage (PLATE group) from August 2010 to January 2012. All operations were performed by the same senior doctor. Randomization procedure involved opening one of the 50 envelopes for each of the 50 patients. The contents of envelop allocated the patients to the PREVAIL group or the PLATE group. The patients received an explanation of the study protocol and agreed to participate in the study. All the patients gave their written informed consent prior to enrolment into the study before surgery. Inclusion and exclusion criteria are summarized in Table 1.
Surgery consisted of single-level ACDF. To perform the intervention, the patient was placed on a surgical bed in the supine position with neck extended slightly; under general anaesthesia, anterior-oblique longitudinal approach was used, overlying the medial border of the sternocleidomastoid muscle at the level of operated intervertebral disc. The trachea and oesophagus were retracted medially and the neurovascular bundle with the sternocleidomastoid muscle laterally. After fluoroscopic confirmation of the affected level, a complete discectomy and careful endplate preparation were performed under microscope. The upper and lower endplates were prepared by removing the overlying cartilage and preserving the hardest subchondral bone. After the decompression was completed, intraoperative evaluations using a trial cage were made to determine the appropriate cage size. A PREVAIL or a CORNERSTONE PEEK cage (Medtronic Sofamor Danek, Memphis, TN) was used. The cage was filled with autograft cancellous bone, which was obtained from the anterior iliac crest. For the patients with a CORNERSTONE PEEK cage, a dynamic plate (PREMIER, Medtronic Sofamor Danek, Memphis, TN) was used for augmentation. The size and the position of the plate were determined to minimize soft tissue irritation and provide adequate stability. The superior and inferior edge of the plate was located so as not to extend to the position beyond 5 mm from the adjacent disc space. After the plate size was selected, anterior surface of the spine was flattened by using a burr or rongeur to make a space for the plate to sit flush. Screws were angled cephalad and caudad away from the disc space and directed slightly medial. Intraoperative landmarks including endplate orientation and uncovertebral joints were used for optimal plate positioning. Finally, confirmatory fluoroscopy was obtained to ensure appropriate plate and graft positions and screw lengths.
Typical post-operative images of the patient with use of a PREVAIL are shown in Fig. 2. In both the groups, no neck collars were used post-operatively.
The clinical findings were assessed using the visual analogue scale (VAS) and the Odom’s criteria [16]. A 10-point VAS scores for neck and arm pain were obtained preoperatively and at 3, 6, 12, and 24 months post-operatively. At 24 months after surgery, the outcomes were rated according to the Odom’s criteria as excellent, good, fair, or poor, depending on the resolution, improvement, or persistence of preoperative symptoms. The rate of dysphasia was graded depending on the patient’s state as none, mild, moderate, or severe according to the method of Bazaz et al. [17].
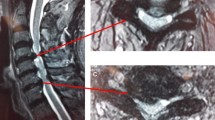
At 12 and 24 months post-operatively, the fusion was evaluated by assessing the multi-planar reconstruction computed tomography (MPR-CT). Fusion was confirmed by the presence of continuous trabecular bone bridges in at least one of the following locations: anterior, within, or posterior to the cage.
Sagittal alignment of the cervical spine (SACS) and sagittal segmental alignment (SSA) on lateral radiographs were evaluated preoperatively and at 3, 6, 12, and 24 months post-operatively. SACS was defined as the angle between the inferior endplate of C2 and C7. SSA was defined as the angle between the upper endplate of the upper vertebral body and the lower endplate of the lower vertebral body.
Subsidence was defined as a decrease in the total intervertebral disc height between the two fused vertebral bodies and was determined by comparing the follow-up lateral radiographs with the first post-operative radiographs taken at 1 week after surgery. A decrease in total intervertebral disc height ≥2 mm was considered to be significant subsidence (Fig. 3).
Prevertebral soft tissue swelling (PSTS) was measured according to the method by Song et al. [18]. In the lateral radiographs at follow-up, the distance from the anterior margin of plates to the posterior margin of the airway shadow was measured. The preoperative distance from the anterior surface of the operated vertebra to the airway shadow was used as control. The measurement ratio of post-operative distance to control (PSTS ratio) was calculated and used for analysis.
The adjacent-level ossification (ALO) was graded on a score of 0 (normal) to 3 (severe), according to the classification by Park et al. [19]. Grade 0 is characterized by no ossification, Grade 1 is characterized by ossification occupying <50 % of the adjacent disc space height, Grade 2 is characterized by ossification extending beyond 50 % of the adjacent disc space height, and Grade 3 is characterized by bridging of 100 % of the adjacent disc space with bone. The scores were then analysed for ALO differences within and between the groups. The distance between the tip of the plate and the adjacent disc space (plate-to-disc distance) was measured on the immediate post-operative lateral radiograph for the PLATE group.
All measurements were obtained using a picture archiving and communication system, workstation. Radiological variables were measured by an experienced spine surgeon not involved in the care of study subjects.
Statistical analysis
The data from this study were analysed through the use of the SPSS 17.0 statistics software program (SPSS Inc., Chicago, USA). A t test was used for normally distributed continuous variables. Categorical variables were analysed with Fisher’s exact test or with a Chi-square analysis. If needed, a Bonferroni correction was performed. A p value <0.05 was considered statistically significant.
Intra-observer reliability was assessed by calculating the intra-class correlation coefficients (ICC) for numeric variables and κ values for categorical variables. A κ value >0.40 indicated poor agreement; 0.41–0.60, moderate agreement; 0.61–0.80, substantial agreement; and 0.81 or greater, excellent agreement. Intra-observer reliability was tested by repeated measurements for SACS, SSA, and PSTS. ICC of the SACS, SAS, and PSTS was 0.84, 0.91, and 0.82. Because ICC indicated high test–retest reliability, measurements were taken three times and the mean of the readings was used.
Results
Of the 50 patients initially enroled in the study, 46 reached the final follow-up interval with complete clinical and radiological evaluations; one patient in the PREVAIL group and three patients in the PLATE group were excluded due to incomplete data. Table 2 shows the baseline characteristics of both the groups. No significant differences were found between both the groups.
The mean surgical time was significantly shorter for the patients in the PREVAIL group (116.4 ± 17.1 min) than that for those in the PLATE group (128.5 ± 17.4 min; p < 0.05). The mean surgery-related blood loss was 27.7 ± 19.0 ml in the PREVAIL group and 30.1 ± 25.8 ml in the PLATE group with no significant difference (p = 0.717). The cage height in the PREVAIL group was 5 mm in 8 cases, 6 mm in 11 cases, and 7 mm in 5 cases, whereas 5 mm in 5 cases, 6 mm in 14 cases, and 7 mm in 3 cases in the PLATE group, respectively.
The neck pain and arm pain were improved at 24 months after surgery in both the groups (p < 0.001).The VAS score for neck pain and arm pain did not reveal any significant differences between both the groups at any follow-up points (Table 3). The comprehensive clinical outcome using Odom’s criteria at 24 months after surgery was similar between both the groups.
The radiological fusion rate did not show any significant differences between both the groups. At 12 months, 22 patients (92 %) in the PREVAIL group and 21 patients (96 %) in the PLATE group had undergone fusion. At 24 months, fusion rate was 96 % in the PREVAIL group and 100 % in the PLATE group.
Preoperative SACS and SSA were significantly improved at 24 months after surgery in both the groups (p < 0.001, SSA; p < 0.001, SACS). There were no significant differences between both the groups at preoperatively and at any follow-up points (Table 4).
The subsidence rate of the PREVAIL group (3 cases; 12.5 %) was higher than that of the PLATE group (2 cases; 9.1 %) at 12 months. At 24 months, the subsidence rate of the PREVAIL group (4 cases; 16.7 %) was also higher compared with that of the PLATE group (3 cases; 13.6 %). However, the difference was not statistically significant between both the groups regardless of the period (p = 0.711 at 12 months; p = 0.775 at 24 months). Subsidence at the upper endplate was observed in 2 cases, and in the remaining 5 cases, lower endplate was involved.
Table 5 shows the change of averaged ALO scores during follow-up. Preoperatively, ALO was observed in two patients (8.3 %) for the PREVAIL group and one patient (4.5 %) for the PLATE group without significant difference. The ALO score was increased during the follow-up period in both the groups (p < 0.001 at 24 months). At 24 months, newly developed ALO was observed in 14 patients (63.6 %) for the PLATE group and three patients (12.5 %) for the PREVAIL group with statistically significant difference (p < 0.01). The PREVAIL group had significantly lower ALO score than the PLATE group at 24 months. In the PLATE group, 15 patients had a plate-to-disc distance of <5 mm. Of those, 11 patients (73.3 %) developed ALO. In seven patients with a plate-to-disc distance ≥5 mm, ALO was developed in three patients (42.9 %). There was a trend towards the higher incidence of ALO in the patients with a plate-to-disc distance of <5 mm, but no significant difference was found between both the groups (p = 0.166).
In the early post-operative period, nine patients (38 %) in the PREVAIL group and ten patients (46 %) in the PLATE group complained about dysphasia. The difference was not significant (p = 0.584). All patients presented with mild dysphasia. At 1 month after surgery, the incidence of dysphasia was 13 % for the PREVAIL group and 18 % for the PLATE group without significant difference (p = 0.592). At 3 months, we had no patients complained about dysphasia in both the groups.
PSTS was observed at 1 week after surgery in both the groups. The PLATE group had a greater soft tissue swelling than the PREVAIL group at 1 week and 1 month after surgery. However, these differences were not significant (p = 0.107 at 1 week; p = 0.073 at 1 month). At 3 months, PSTS was decreased to the preoperative level in both the groups (Fig. 4).
Intra-observer reliabilities
The κ value of intra-observer agreement was 0.85 for bony fusion and 0.94 for cage subsidence.
Discussion
ACDF and cervical arthroplasty are two possible operative techniques for the treatment of cervical disc diseases. However, Auerbach et al. [20] reported that only 43 % of patients met their inclusion criteria for cervical arthroplasty. In the cases without indications for arthroplasty, ACDF is still the gold standard for surgical treatment. If ACDF is considered as a treatment option, numerous reports have documented the effective use of additional plating in order to avoid pseudoarthrosis, subsidence, and local kyphosis [4–6, 21]. However, the use of additional plating is associated with various complications. Accordingly, recently developed stand-alone anchored cage can be expected to offer a theoretical advantage of favourable clinical and radiological outcomes. Several recent reports described that this type of new stand-alone cage achieved similar clinical and radiological outcomes with lower dysphasia, compared with using a cage with plating [13–15]. Scholz et al. [13] first described the efficacy of this new implant (Zero-P; Synthes GmbH Switzerland, Oberdorf, Switzerland) in 38 patients and demonstrated solid fusion and post-operative pain reduction associated with a low rate of dysphasia, but their analysis was retrospective and a short-term follow-up. Similar favourable outcomes were also reported by Miao et al. [14]. They prospectively compared the application of Zero-P with the use of a PEEK cage with plating and concluded that clinical and radiographic efficacies were similar to those of ACDF using a plate, with a lower incidence of dysphasia. However, their evaluation of fusion status was made by flexion–extension radiographs, and the change of the segment adjacent to the fused level could not be evaluated because of the short-term follow-up.
Despite the small patient population, this is the first detailed prospective study evaluating efficacies of the stand-alone anchored cage with a 2-year follow-up. Similar to the results of previous reports [13–15], the improvement of VAS scores for neck and arm pain, and modified Odom’s criteria in the PREVAIL group was comparable to that of the PLATE group. The mean surgical time was significantly shorter for the PREVAIL group, indicating less invasiveness compared with the PLATE group. This is possibly because fewer steps are needed to introduce the PREVAIL, which has a one-step locking mechanism with simple insertion of the cage and the tightening of the screws.
Solid fusion constitutes a goal of ACDF, since non-union has been linked to poor outcomes. Fraser et al. [6] reported in a meta-analysis that the fusion rate of ACDF with plating has been estimated to be 97.1 % for single-level procedures. Based on the accurate evaluation by MPR-CT, we found the comparable high fusion rate in both the PREVAIL group (96 %) and the PLATE group (100 %). Additionally, the improvement of SACS and SSA was comparable between both the groups. These results indicate that the PREVAIL holds the equivalent capability for solid fusion and correction of cervical alignment to that of the plate fixation.
A relatively high incidence of subsidence in the stand-alone cage has been reported [22]. Clinical outcome of the patients affected by the cage subsidence is controversial. However, subsidence with the secondary kyphotic change may be regarded as a risk factor contributing to progression of degenerative changes in adjacent segments. The subsidence of a stand-alone anchored PEEK cage has not been specifically evaluated in the previous reports. Lee et al. [23] described that the subsidence rate of a Zero-P (58.6 %) was higher than that of a PEEK cage with plating (38.5 %), indicating that plate fixation can support the anterior disc height and prevent subsidence. In contrast, Scholz et al. [13] reported that cage subsidence was not observed in the cases with Zero-P, but their follow-up was 6 months and comparative study with plate fixation was not performed. Our preliminary results suggest that the subsidence rate of a PREVAIL is not higher compared to that of a PEEK cage with plating with intermediate follow-up. Unlike plating, in which anterior surface of the spine is flattened by resecting the osteophytes to make a space for the plate to sit flushes, applying a PREVAIL does not require such procedure. This, along with a secure and rigid screw fixation, probably contributes to preserve the anterior bony support which may potentially reduce the occurrence of subsidence in a PREVAIL. Barsa et al. [24] also reported the advantage of biomechanical support by anterior osteophyte in order to prevent cage subsidence. However, it is well known that the occurrence of cage subsidence might be related to various factors including size, position, and contact surface ratio of a cage as well as bone density and applied distraction during surgery. Therefore, further investigation using a large sample with a longer follow-up has to be needed to reach the definite conclusion.
ACDF with plating is known to be associated with the development of ALO. Park et al. [19] reported that if the plate was <5 mm from the adjacent disc space, the prevalence of ALO development was significantly increased. Therefore, we measured the plate-to-disc distance according to their method. However, significant difference in the rate of ALO was not detected between the patients who had a distance <5 mm and those who had a distance ≥5 mm. Garrido et al. [25] also demonstrated that ALO was developed in 50 % of the patients who had a plate-to-disc distance <5 mm. Yang et al. [26] described that ALO was uncommon after ACDF without plate fixation, developing in 5.5 %, in contrast with the rate of 45.4 % following ACDF with plating. These findings suggest that the fusion itself may not be a major contributor to the ALO development. Lower incidence of ALO in the PREVAIL group in our study supports this hypothesis. Although the exact mechanism has to be elucidated, more extensive stripping of the anterior longitudinal ligament or anterior fibres of the annulus fibrosis and other technical as well as biomechanical considerations associated with plating might be considered as contributing factors.
Dysphasia is a complication that occurs relatively frequent after ACDF. Although no clear mechanism has been suggested, swelling by traction, haematoma, and damage to the pharyngeal nerve plexus and to the hypoglossal nerve during surgery in the upper area have been suggested as risk factors. In addition, damaged soft tissues may adhere to the larynx or oesophagus during healing process and induce dysphasia. Incidence of dysphasia following ACDF with Zero-P has been reported by several authors with different results. Miao [14] and Hofstetter [15] found a significant lower rate of dysphasia in patients with Zero-P compared with those with plating. In contrast, Vanek [27] and Chen [28] described that the potential of Zero-P to reduce the incidence of dysphasia was not confirmed. The result of our study is similar, showing no differences in the rate of dysphasia at any follow-up points between the PREVAIL group and the PLATE group. Additionally, we confirmed that prevertebral soft tissue swelling was also equivalent between both the groups. The reason for these differences is not clear, but the differences in the patient population, the evaluation method, or study design might be the possible factors.
The main limitation is the small number of patients available from this single military installation, although the numbers were sufficient to reach statistical significance. Most of our patients were male military personnel, and their average age is noticeably lower than that of those reported in other studies. These may not be representative of the patient population at other facilities. Accordingly, further study will be needed to evaluate if clinical and radiological findings vary by age or by sex. Second, we did not perform the comparative study between the PREVAIL and the stand-alone PEEK cage. Therefore, a large number of cases with a longer follow-up, comparing the PREVAIL with the stand-alone PEEK cage, have to be studied to confirm our observations. In conclusion, compared to a PEEK cage with plating, a stand-alone anchored PEEK cage (PREVAIL) provided comparable clinical and radiological outcomes with significant lower rate of ALO. However, the potential to reduce the incidence of dysphasia was not confirmed on this sample of patients.
References
Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, Vaccaro AR, Albert TJ (2003) Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 28:134–139
Reynolds AF Jr, Turner PT, Loeser JD (1978) Fracture of the anterior superior iliac spine following anterior cervical fusion using iliac crest. Case Report. J Neurosurg 48:809–810
Samartzis D, Shen F, Goldberg EJ, An HS (2005) Is autograft the gold standard in achieving radiographic fusion with rigid anterior plate fixation? Spine 30:1756–1761
Song KJ, Lee KB (2006) A preliminary study of the use of cage and plating for single-segment fusion in degenerative cervical spine disease. J Clin Neurosci 13:181–187
Kaiser MG, Haid RW Jr, Subach BR, Barnes B, Rodts GE Jr (2002) Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50:229–236
Fraser JF, Hartl R (2007) Anterior approaches to fusion of the cervical spine: a meta-analysis of fusion rates. J Neurosurg Spine 6:298–303
Tortolani PJ, Cunningham BW, Vigna F, Hu N, Zorn CM, McAfee PC (2006) A comparison of retraction pressure during anterior cervical plate surgery and cervical disc replacement: a cadaveric study. J Spinal Disord Tech 19:312–317
Lee MJ, Bazaz R, Furey CG, Yoo J (2005) Influence of anterior cervical plate design on dysphasia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 18:406–409
Kasimatis GB, Panagiotopoulos E, Gliatis J, Tyllianakis M, Zouboulis P, Lambiris E (2009) Complications of anterior surgery in cervical spine trauma: an overview. Clin Neurol Neurosurg 11:118–127
Riley LH III, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG (2005) Dysphasia after cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine 30:2564–2569
Sasso RC, Ruggiero RA Jr, Reilly TM, Hall PV (2003) Early reconstruction failures after multilevel cervical corpectomy. Spine 28:140–142
Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, Garfin SR (1998) Early failure of long segment anterior cervical plate fixation. J Spinal Disord 11:410–415
Scholz M, Schnake KJ, Pingel A, Hoffmann R, Kandziora F (2011) A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop Relat Res 469:666–673
Miao J, Shen Y, Kuang K, Yang L, Wang X, Chen Y, Chen D (2013) Early follow-up outcomes of a new zero-profile implant used in anterior cervical discectomy and fusion. J Spinal Disord Tech 26:E193–E197. doi:10.1097/BSD.0b013e31827a2812
Hofstetter CC, Kesavabhotla K, Boockvar JA (2013) Zero-profile anchored spacer reduces rate of dysphasia compared to ACDF with anterior plating. J Spinal Disord Tech. doi:10.1097/BSD.0b013e31828873ed
Odom GL, Finney W, Woodhall B (1958) Cervical disc lesions. JAMA 166:23–28
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphasia after anterior cervical spine surgery: a prospective study. Spine 27:2453–2458
Song KJ, Choi BW, Kim HY, Jeon TS, Chang H (2012) Efficacy of postoperative radiograph for evaluating the prevertebral soft tissue swelling after anterior cervical discectomy and fusion. Clin Orthop Surg 4:77–82
Park JB, Cho YS, Riew KD (2005) Development of adjacent-level ossification in patients with an anterior cervical plate. J Bone Joint Surg Am 87:558–563
Auerbach JD, Jones KJ, Fras CI, Balderston JR, Rushton SA, Chin KR (2008) The prevalence of indications and contraindications to cervical disc replacement. Spine J 8:711–716
Schneeberger AG, Boos N, Schwarzenbach O, Aebi M (1999) Anterior cervical interbody fusion with plate fixation for chronic spondylotic radiculopathy: a 2- to 8-year follow-up. J Spinal Disord 12:215–220
Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A (2006) Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine 4:447–453
Lee CH, Hyun SJ, Kim MJ, Yeom JS, Kim WH, Kim KJ, Jahng TA, Kim HJ, Yoon SH (2013) Comparative analysis of 3 different construct systems for single-level anterior cervical discectomy and fusion: stand-alone cage, iliac graft plus plate augmentation, and cage plus plating. J Spinal Disord Tech 26:112–118
Barsa P, Suchomel P (2007) Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J 16:1395–1400
Garrido BJ, Wilhite J, Nakano M, Crawford C, Baldus C, Riew KD, Sasso RC (2011) Adjacent-level cervical ossification after Bryan cervical disc arthroplasty compared with anterior cervical discectomy and fusion. J Bone Joint Surg Am 93:1185–1189
Yang JY, Song HS, Lee M, Bohlman HH, Riew KD (2009) Adjacent level ossification development after anterior cervical fusion without plate fixation. Spine 34:30–33
Vanek P, Bradac O, Delacy P, Lacman J, Benes V (2013) Anterior interbody fusion of the cervical spine with Zero-P spacer: prospective comparative study-clinical and radiological results at a minimum 2 years after surgery. Spine 38(13):E792–E797. doi:10.1097/BRS.0b013e3182913400
Chen Y, He Z, Yang H, Liu X, Wang X, Chen D (2013) Anterior cervical discectomy and fusion for adjacent segment disease. Orthopedics 36(4):E501–E508. doi:10.3928/01477447-20130327-30
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nemoto, O., Kitada, A., Naitou, S. et al. Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol 25 (Suppl 1), 127–134 (2015). https://doi.org/10.1007/s00590-014-1547-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1547-4