Abstract
Background
Injection of a suspension of miriplatin into the hepatic artery has been employed for the treatment of hepatocellular carcinoma (HCC). The efficacy and safety of transcatheter arterial chemoembolization (TACE) using miriplatin were evaluated.
Methods
A total of 236 patients with unresectable HCC received miriplatin administration through the hepatic artery, followed by embolization with porous gelatin particles. The efficacy of this treatment modality was evaluated by contrast-enhanced computed tomography performed 1 month later and its safety based on the Common Terminology Criteria for Adverse Events (CTCAE).
Results
Miriplatin was used at a median dose of 66 mg. The therapeutic efficacy was evaluated in 130 patients, and the overall and complete response rates were 70.0 and 37.7%, respectively. The efficacies differed depending on the staging and Japan integrated staging (JIS) scores of the HCCs, with the overall and complete response rates being 87.7 and 66.7% for stage I and stage II HCC, and 56.2 and 15.1% for stage III and stage IV HCC, respectively; the corresponding rates were 93.2 and 70.5%, respectively, for HCCs with score 0 and score 1, and 58.1 and 20.9%, respectively, for those with scores 2–4. The stage of HCC was a significant independent factor associated with curative effects of TACE using miriplatin. Grade 3 elevation of serum transaminase levels was found in 23.4% of the patients; however, the values returned to the baseline levels.
Conclusions
Miriplatin is a useful and safe agent for TACE in patients with HCC stage I or II and/or JIS score 0 or 1 only when radiofrequency ablation and liver resection cannot be performed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Japan, more than 30,000 people die of hepatocellular carcinoma (HCC) each year, and HCC ranks third and fifth, respectively, in men and women as a cause of death due to malignant neoplasms [1]. Surgical resection and radiofrequency ablation (RFA) of tumors, chemotherapy through the hepatic artery with or without embolization of the feeding arteries, molecular-targeted therapy, or cadaveric or living-donor liver transplantation have been selected as therapeutic procedures for HCC depending on three factors: degree of liver damage, number of tumors, and the diameter of the tumors [2].
Surgical resection may be the most preferable therapeutic procedure for HCC in suitable candidates. However, it can be performed as the initial treatment in only about 30% of the patients, according to a report by the Liver Cancer Study Group of Japan [3]. Hepatectomy is precluded in the large number of HCC patients with decreased liver function due to underlying cirrhosis and/or the presence of multiple tumors in the liver. Even when curative hepatectomy is performed, recurrent HCC develops in about 80% of the patients within 5 years after the resection because of intrahepatic metastasis from the primary tumors or the multicentric carcinogenesis of HCC [4]. RFA therapy has been employed as an alternative procedure to surgical resection for the treatment of HCC [5]. Although RFA therapy has been revealed to show almost equivalent therapeutic efficacy to hepatectomy in cases of HCC with small tumors (tumor diameter of 3 cm or less) [6], the procedure is not suitable for the treatment of HCC patients with three or more tumors and/or tumors measuring more than 3 cm in diameter [2, 6]. On the other hand, liver transplantation is recommended for HCC patients with class C liver damage when the number of tumors is 3 or less and the tumor diameters do not exceed 3 cm, or a single tumor is present, with a diameter not exceeding 5 cm (Milan’s criteria) [2, 7].
According to the guideline for treatment of HCC proposed by the Japan Society of Hepatology in 2009, transcatheter arterial chemoembolization (TACE) is recommended for HCC patients with class A and B liver damage when the number of tumors is 2 or 3 and the tumor diameter is greater than 3 cm [2, 8]. Also, both TACE and hepatic arterial infusion chemotherapy are recommended for HCC patients with 4 or more tumors [2, 9]. Thus, chemotherapy through the hepatic artery with or without subsequent arterial embolization plays a central role in the treatment of HCC patients with large and/or multiple tumors. Miriplatin is a novel lipophilic platinum complex that was approved in Japan for use as a transhepatic arterial chemotherapeutic agent in the treatment of HCC in 2010 [10]. In general, miriplatin is suspended in an oily contrast medium and injected through the hepatic artery without successive embolization with porous gelatin particles. It has been reported, however, that the tumor necrosis is more extensive in cases receiving TACE than in those receiving transarterial infusion chemotherapy, and that the former procedure yields superior survival rates as compared with the latter [11, 12]. These observations prompted us to postulate that the therapeutic efficacy of transhepatic arterial injection of miriplatin may be increased when the intra-arterial administration is followed by embolization of the tumor feeding arteries. Thus, we performed an open trial to evaluate the therapeutic efficacy and safety of TACE therapy using miriplatin in patients with unresectable HCC.
Patients and methods
Patients
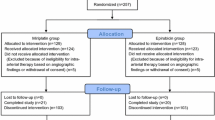
The subjects were 236 consecutive patients with unresectable HCC who underwent TACE therapy using miriplatin at Saitama Medical University Hospital between February and December 2010. Written informed consent was obtained from each patient, and the study was conducted with the approval of the hospital’s institutional review board. The diagnosis of HCC was confirmed by means of at least two of the following imaging modalities: ultrasonography with or without contrast medium, contrast-enhanced computed tomography (CT), and gadolinium-EOB-enhanced magnetic resonance imaging (MRI).
The demographic and clinical characteristics of the patients are shown in Table 1. The patients consisted of 160 males and 76 females, ranging in age from 48 to 91 years. All patients had underlying chronic hepatitis or liver cirrhosis, and the degree of liver damage (Child–Pugh classification) was grade A, B, and C in 149, 86 and 1 patients, respectively. The extent of HCC progression was as follows: (1) the number of tumors was 2 or more in 144 patients (61.0%), (2) the diameter of the largest tumor was greater than 2 cm in 138 patients (58.5%), and (3) portal vein thrombosis was found in 17 patients (7.2%). Thus, 119 patients (50.4%) were classified as having stage III HCC, characterized by the absence of distant metastasis and fulfillment of two of the three above intrahepatic conditions, based on the staging system of the Liver Cancer Study Group of Japan [13]. On the other hand, 101 (42.8%) patients were diagnosed as having stages I and II HCC, and TACE with miriplatin was performed in these patients on the basis of the following reasons: (1) RFA therapy cannot be done because of the locations of tumors, where ablation may provoke insufficient therapeutic efficacy and/or adverse effects against neighborhood organs; (2) the number of tumors was 3 or more; (3) surgical resection was not performed because of liver damage or refusal by the patients. Also, 17 patients (7.2%) were assigned a JIS score of 0, and 65 (27.5%), 87 (36.9%), and 67 patients (28.4%) were assigned scores of 1, 2, and 3–4, respectively, according to the JIS scoring system proposed by the same group [14].
Therapeutic procedures
A 3-Fr or 4-Fr Shepherd Hook catheter (FansacIV or Angiomaster, Terumo Clinical Supply, Gifu, Japan) was inserted via the right femoral artery, and portography through the superior mesenteric artery and celiac arteriography were performed according to Seldinger’s method. Then, a 2.0-Fr or 2.1-Fr microcatheter (Sniper 2, Terumo Clinical Supply or Tangent, Boston Scientific Japan, Tokyo, Japan) was advanced into the feeding arteries of each tumor, and miriplatin (Miripla, Dainippon-Sumitomo Pharmaceutical Co. Ltd., Osaka, Japan) suspended in lipiodol solution (Lipiodol Ultra-Fluid, Dainippon-Sumitomo Pharmaceutical Co. Ltd) was injected into the hepatic artery at a concentration of 20 mg/mL. The dose of miriplatin was determined depending on the size of the tumors, but the injection was discontinued immediately before the flow ceased completely. In cases of treatment for multiple tumors, the injection was repeated through the corresponding feeding arteries; however, the total dose of miriplatin per session of the procedure was limited to 120 mg. Thereafter, the feeding arteries to the tumors were embolized with porous gelatin particles (Gerpart, Nippon Kayaku, Tokyo, Japan). The extent of embolization was determined depending on the number and location of the tumors and the degree of liver damage. A 5-HT3 antagonist was administered before the miriplatin injection, whereas hydration by intravenous administration of fluids was not undertaken before the TACE procedure.
Evaluation of the therapeutic efficacy
The therapeutic efficacy was evaluated by contrast-enhanced CT performed 1 month after the TACE procedures, according to the criteria proposed by the Liver Cancer Study Group of Japan [13]. According to these criteria, the percentages of necrotic areas in the tumors are 100%, between 50 and 99%, and less than 50%, respectively, in cases classified as showing TE4, TE3, and TE2, and the extent of tumor progression is less than 25 and at least 25%, respectively in cases showing TE2 and TE1.
The patients receiving additional therapies, such as surgical resection and RFA, within 1 month after the procedure were excluded from the analysis of the therapeutic efficacy of TACE. Also, patients with a history of previous TACE or transarterial infusion chemotherapy using miriplatin were excluded from the evaluation. In contrast, the safety of the TACE was evaluated in all patients for 90 days following the procedures. Adverse events were graded according to the Common Terminology Criteria for Adverse Events (CTCAE), version 4.0, published by the National Cancer Institute [15], except for peripheral blood cells counts and serum levels of albumin and bilirubin, because derangement of these parameters was found frequently even before the TACE procedures in HCC patients with underlying chronic liver disease. For these latter parameters, the severity of the adverse effect was classified according to the gradient of increase of the CTCAE grade after the TACE procedure as compared with that at the baseline, after adaptation of the values for CTCAE grading. The serum creatinine level was also excluded from the evaluation of adverse effects in patients under maintenance hemodialysis for chronic renal failure.
Statistical analysis
The Fisher’s exact test and chi-square test were used to analyze the relation between the tumor response rates and the demographic and clinical characteristics of the patients. Multivariate logistic regression analysis was done to elucidate significant factors influencing the therapeutic efficacy of TACE using miriplatin. p values of less than 0.05 were considered as indicating statistical significance.
Results
Miriplatin was used at the median dose of 66 mg (range 10–120 mg) for a single TACE procedure. Among the 236 patients who underwent TACE using miriplatin, the therapeutic efficacy was evaluated in 130 patients, because 16 patients required RFA therapy or surgical resection within 1 month after the TACE procedure, and 83 patients had a previous history of undergoing TACE and/or transarterial infusion chemotherapy using miriplatin. The reasons for exclusion of the remaining 7 patients from the efficacy evaluation were that 2 of the patients died within 1 month after the TACE procedure, and imaging examinations were not performed in 5 patients.
As shown in Table 2, the overall response rate (TE3 and TE4) and complete response rate (TE4) for the TACE procedures were 70.0 and 37.7%, respectively. When the therapeutic efficacy was assessed according to the stage of the HCC, the overall and complete response rates were 87.7 and 66.7%, respectively, in patients with stages I or II HCC, and 56.2 and 15.1%, respectively, i.e., significantly lower, in patients with stage III or IV HCC. Furthermore, both the overall and complete response rates in the HCC patients differed significantly depending on the JIS scores; the overall and complete response rates were 93.2 and 70.5%, respectively, in cases with a score of 0 or 1, and 58.1 and 20.9%, respectively, in cases with scores of 2–4. Moreover, both the response rates were significantly higher in patients without a previous history of TACE than in those who had undergone TACE using antitumor agents other than miriplatin. As shown in Table 3, multivariate analysis revealed that the stage of HCC (stages I and II vs. III and IV) was a factor associated with the curative effect of TACE using miriplatin with odds ratio of 4.87 (p = 0.001), whereas previous TACE with anticancer agents other than miriplatin was not selected as an independent factor that influenced the curative effect (odds ratio = 2.30, p = 0.063).
The adverse effects observed following TACE with miriplatin are shown in Table 4. Fever and nausea were found transiently in most patients, but both symptoms were mild; the percentages of patients showing fever and nausea of grade 2 or more were 4.7 and 7.7%, respectively. Also, the serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels increased after the TACE procedures in most of the patients, and grade 2, 3, and 4 elevations were found in 56 (23.8%), 53 (22.6%), and 2 patients (0.8%), respectively. The serum AST and ALT levels returned to the baseline levels within a month in all patients. Elevation of the serum total bilirubin concentrations up to CTCAE grade 3 (greater than 3.6 mg/dL) was observed in 6 patients. Among them, serum total bilirubin level concentrations corresponding to CTCAE grade 2 (between 1.8 and 3.6 mg/dL) and grade 1 (between 1.3 and 1.7 mg/dL) were already present in 4 and 2 patients, respectively, before the TACE procedures. Thereby, the extent of elevation of the total serum bilirubin concentration was classified as grade 2 and grade 3 in 33 (14.0%) and 0 patients, respectively. Derangements of the blood cell counts and serum albumin and creatinine concentrations were found in only a few patients; the percentages of patients showing grade 2 or more severe derangements were 2.1% for neutropenia, 0% for anemia, 1.7% for thrombocytopenia, 0.4% for decrease of the serum albumin concentration, and 3.0% for elevation of the serum creatinine concentration.
As shown in Table 5, 6 patients (2.5%) of this study died between 10 and 56 days after the TACE procedures. The extension of HCC progression was stage III or IV in all of these patients, and there were no treatment-related deaths; the cause of death was HCC progression in 2 patients, HCC rupture in 3 patients, and complicating pneumonia in 1 patient.
Discussion
HCC tumors receive their blood supply from the hepatic artery. Thus, TACE and transarterial infusion chemotherapy are performed to induce necrosis and apoptosis of HCC cells through the action of anticancer agents, as well as through the ischemia induced by embolization with porous gelatin particles and/or lipiodol, an oily contrast medium. Several anticancer agents have been used for these procedures, e.g., epirubicin, doxorubicin, mitomycin C, carboplatin, and cisplatin. These agents are injected into the hepatic artery after being suspended in lipiodol. Lipiodol is distributed and retained in the microcirculation of HCC tumors for long periods of time [16], suggesting that the anticancer agents concomitantly injected with lipiodol may accumulate in HCC tissues and exert their anticancer effects exclusively on the tumors for prolonged periods of time. However, all of these agents are water soluble, and not stable in suspension in lipiodol. Zinostatin stimalamer, a lipophilic anticancer agent, approved for transhepatic arterial administration, has been used for the therapy of HCC in Japan since 1994 [17]. However, zinostatin stimalamer is not suitable for TACE, because this agent frequently produces vascular damage, necessitating discontinuation of the procedures. Thus, a novel lipid-soluble anticancer agent for the treatment of HCC patients that would not produce vascular damage has been awaited.
Miriplatin, (SP-4-2)-[(1R,2R)-cyclohexane-1,2-diamine-N,N′]-bis(tetradecanoato-O) platinum, is a novel lipophilic platinum complex reported by Maeda et al. [18]. Miriplatin can easily be suspended in lipiodol and releases active platinum compounds into the aqueous phase gradually [19]. This agent was approved for use in chemolipiodolization therapy through the hepatic artery for HCC in 2010. Hanada et al. [20] reported that the concentrations of platinum compounds were greater in the tumors than in the non-tumor regions of the liver, when miriplatin suspension in lipiodol was injected into the hepatic artery of rats bearing hepatoma AH109A tumors in the liver. They also found that the concentrations of the platinum compounds in the tumors decreased more slowly in cases administered miriplatin than in those administered cisplatin similarly suspended in lipiodol [20]. Also, a randomized phase II trial revealed that miriplatin was more effective as an agent for transarterial infusion chemotherapy against HCC as compared with zinostatin stimalamer; the complete response rate was 26.5% in miriplatin-treated patients, whereas it was 17.9% in zinostatin stimalamer-treated patients, 48.4% of whom developed drug-induced vascular damage [10]. Considering these observations, miriplatin would seem to be among the most useful of anticancer agents currently available for TACE as well as transarterial infusion chemotherapy in the treatment of unresectable HCC.
Thus, the efficacy and safety of TACE using miriplatin were evaluated in patients with unresectable HCC. The majority of patients had underlying liver cirrhosis due to hepatitis C virus infection, and the extent of liver damage was classified as Child–Pugh class A or class B in 99.6% of the patients. In contrast, the patients showed marked divergence in respect of the stage of progression of the HCC; the percentages of patients with stage I, II, III, and IV disease were 11.4, 31.4, 50.4, and 6.8%, respectively, according to the staging criteria proposed by the Liver Cancer Study Group of Japan, and those with JIS scores of 0, 1, 2, and 3–4 were 7.2, 27.5, 36.9, and 28.4%, respectively, as shown in Table 1. The doses of miriplatin and the extent of embolization by the porous gelatin particles were determined depending on both the extent of liver damage and the stage of HCC progression in each patient.
In the present study, the overall response rate and complete response rate were 70.0 and 37.7%, respectively, both of which were greater than those obtained in a randomized phase II trial performed to evaluate the efficacy of transarterial infusion chemotherapy using miriplatin [10]. Ikeda et al. [21] reported that the overall response rate was 73%, with complete response rate of 32%, in a clinical trial conducted to evaluate the therapeutic efficacy of TACE using cisplatin suspended in lipiodol. These data are almost equivalent to those obtained in our study. The ratios of TE3 and/or TE4 may be altered depending on the time points of evaluation with CT after TACE procedures. The response rates might be decreased when the therapeutic efficacy was evaluated later than 1 month after the TACE procedure with miriplatin. These matters should be investigated in the future. Also, the percentages of patients with stages I and II HCC may influence the therapeutic efficacies of TACE procedures. Thus, a randomized controlled study is warranted to compare therapeutic efficacy of TACE using miriplatin with that using cisplatin especially in patients with advanced HCC.
It is noteworthy that the therapeutic efficacy of TACE using miriplatin was excellent in patients with stage I or II HCC; the overall response rates in patients with stage I and stage II disease were 100 and 83.7%, respectively. Similar excellent therapeutic efficacy was found in HCC patients with a JIS score of 0 and 1, who showed overall response rates of 100 and 91.7%, respectively. However, it should be noted that TE4 therapeutic efficacy, characterized by complete necrosis of HCC, was not obtained in 28.6% of patients with stage I HCC and 34.9% of those with stage II HCC. TACE with miriplatin should be done in patients with stage I or II HCC only when RFA and liver resection cannot be performed because of medical and personal reasons.
In contrast, both the response rates were low in HCC patients with stage III or IV disease and those with JIS scores of 2–4. Thus, the optimal doses of miriplatin and optimal technique of embolization for the treatment of advanced HCC should be investigated further. Also, the usefulness of TACE with miriplatin for patients receiving TACE with anticancer agents other than miriplatin should be further investigated, because the previous TACE was not selected as an independent factor influencing the overall response rate (p = 0.063).
TACE therapy using miriplatin produced elevations of the serum AST and ALT levels up to CTCAE grade 3 or grade 4 in 23.4% of the patients, although the elevation was only transient in all of the patients. Transient elevations of the serum transaminase levels are commonly observed following TACE using other anticancer agents, such as epirubicin, doxorubicin, and cisplatin [21–24]. Elevation of the serum total bilirubin concentration up to CTCAE grade 2 was found in 14.0% of the patients, and the values eventually returned to the baseline in all patients. There were no cases who showed progression of liver failure following the TACE procedures. Also, there were no treatment-related deaths. Thus, TACE therapy using miriplatin is considered to be safe when embolization procedures are performed completely or partially, depending on the number and size of tumors and the degree of liver damage. In the present study, anorexia and vomiting of CTCAE grade 3 were observed in only 0.4 and 0% of the patients, respectively. Even though hydration was not undertaken before the TACE procedures in the present study, elevation of the serum creatinine concentration of CTCAE grade 3 or more was not found in any patients. In contrast, in a phase II study of transarterial infusion chemotherapy using a fine-powder formulation of cisplatin, anorexia, vomiting, and elevation of the serum creatinine concentration of CTCAE grade 3 were found in 22.5, 6.3, and 2.5% of the enrolled patients, respectively [25]. It would seem that miriplatin, which is stable in lipiodol and is retained in the tumors for prolonged periods of time, evokes fewer adverse effects derived from toxicity to the extrahepatic organs.
In conclusion, miriplatin appears to be a useful agent for TACE in patients with unresectable HCC. Therapeutic modifications to improve the treatment efficacy for patients with advanced HCC as well as those with a previous history of TACE need to be further investigated, because TACE using miriplatin may be associated with fewer adverse reactions derived from toxicity to the extrahepatic organs.
References
Umemura T, Ichijo T, Yoshizawa K, Tanaka E, Kiyosawa K. Epidemiology of hepatocellular carcinoma in Japan. J Gastroenterol. 2009;44(Suppl):102–7.
Arii S, Sata M, Sakamoto M, Shimada M, Kumada T, Shiina S, et al. Management of hepatocellular carcinoma: report of consensus meeting in the 45th annual meeting of the Japan Society of Hepatology (2009). Hepatol Res. 2010;40:667–85.
Ikai I, Arii S, Ichida T, Okita K, Omata M, Kojiro M, et al. Report of the 16th follow-up survey of primary liver cancer. Hepatol Res. 2005;32:163–72.
Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38:200–7.
Rossi S, Buscarini E, Garbagnati F, Garbagnati F, Stasi MD, Quaretti P, et al. Percutaneous treatment of small hepatic tumors by an expandable RF needle electrode. Am J Roentgenol. 1998;170:1015–22.
Arii S, Yamaoka Y, Futagawa S, Inoue K, Kobayashi K, Kojiro M, et al. Results of surgical and nonsurgical treatment for small-sized hepatocellular carcinomas: a retrospective and nationwide survey in Japan. The Liver Cancer Study Group of Japan. Hepatology. 2000;32:1224–9.
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–9.
Llovet JM, Real MI, Montana X, Planas R, Coll S, Aponte J, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359:1734–9.
Sumie S, Yamashita F, Ando E, Tanaka M, Yano Y, Fukumori K, et al. Interventional radiology for advanced hepatocellular carcinoma: comparison of hepatic artery infusion chemotherapy and transcatheter arterial lipiodol chemoembolization. Am J Radiology. 2003;181:1327–34.
Okusaka T, Kasugai H, Ishii H, SM-11355 Japan Study Group. A randomized phase II trial of intraarterial chemotherapy using a novel lipophilic platinum derivative (SM-11355) in comparison with zinostatin stimalamer in patients with hepatocellular carcinoma. J Clin Oncol. 2009;27:222s.
Takayasu K, Shima Y, Muramatsu Y, Moriyama N, Yamada T, Makuuchi M, et al. Hepatocellular carcinoma: treatment with intraarterial iodized oil with and without chemotherapeutic agents. Radiology. 1987;163:345–51.
Takayasu K, Arii S, Ikai I, Kudo M, Matsuyama Y, Kojiro M, et al. Overall survival after transarterial lipiodol infusion chemotherapy with or without embolization for unresectable hepatocellular carcinoma: propensity score analysis. Am J Radiol. 2010;194:830–7.
The Liver Cancer Study Group of Japan. The general rules for the clinical and pathological study of primary liver cancer. Tokyo: Kanehara; 2003.
Kudo M, Cung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan integrated staging score (JIS score). J Gastroenterol. 2003;38:207–15.
National Cancer Institute. Common terminology criteria for adverse events (CTCAE), version 4.0. 2011. http://evs.nci.nih.gov/ftp1/CTCAE/. Accessed 9 May 2011.
Nakakuma K, Tashiro S, Hiraoka T, Ogata K, Ootsuka K. Hepatocellular carcinoma and metastatic cancer detected by iodized oil. Radiology. 1985;154:15–7.
Taguchi T, Saito T, Ota J, Nakao I, Ohashi K, Nakamura H, et al. Phase II study of YM881 (zinostatin stimalamer) suspension injected into the hepatic artery. Jpn J Cancer Chemother. 1991;18:1665–75.
Maeda H, Uchida NA, Sasaki T. Liposoluble platinum(II) complexes with antitumor activity. Jpn J Cancer Res. 1986;77:523–5.
Kishimoto S, Noguchi T, Yamaoka T, Fukushima S, Takeuchi Y. In vitro release of SM-11355, cis[((1R,2R)-1,2-cyclohexanediamine-N,N’)bis(myristato)] platinum (II) suspended in lipiodol. Biol Pharm Bull. 2000;23:637–40.
Hanada M, Baba A, Tsutsumishita Y, Noguchi T, Yamaoka T, Chiba N, et al. Intra-hepatic arterial administration with miriplatin suspended in an oily lymphographic agent inhibits the growth of tumors implanted in rat livers by including platinum-DNA adducts to form and massive apoptosis. Cancer Chemother Pharmacol. 2009;64:473–83.
Ikeda M, Maeda S, Shibata J, Muta R, Ashihara H, Tanaka M, et al. Transcatheter arterial chemotherapy with and without embolization in patients with hepatocellular carcinoma. Oncology. 2004;66:24–31.
Ono Y, Yoshimaru T, Ashikaga R, Inoue M, Shindou H, Fuji K, et al. Long-term results of lipiodol-transcatheter arterial embolization with cisplatin or doxorubicin for unresectable hepatocellular carcinoma. Am J Clin Oncol. 2000;23:564–8.
Yodono H, Matsuo K, Shinohara A. A retrospective comparative study of epirubicin-lipiodol emulsion and cisplatin-lipiodol suspension for use with transcatheter arterial chemoembolization for treatment of hepatocellular carcinoma. Anti-Cancer Drugs. 2011;22:277–82.
Kawamura Y, Ikeda K, Hirakawa M, Hosaka T, Kobayashi M, Saitoh S, et al. Efficacy of platinum analogue for advanced hepatocellular carcinoma unresponsive to transcatheter arterial chemoembolization with epirubicin. Hepatol Res. 2009;39:346–54.
Yoshikawa M, Ono N, Yodono H, Ichida T, Nakamura H. Phase II study of hepatic arterial infusion of a fine-powder formulation of cisplatin for advanced hepatocellular carcinoma. Hepatol Res. 2008;38:474–83.
Acknowledgments
This study was supported in part by Grants-in-Aid from the Ministry of Health, Labor, and Welfare of Japan to Research on Hepatitis.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Imai, Y., Chikayama, T., Nakazawa, M. et al. Usefulness of miriplatin as an anticancer agent for transcatheter arterial chemoembolization in patients with unresectable hepatocellular carcinoma. J Gastroenterol 47, 179–186 (2012). https://doi.org/10.1007/s00535-011-0475-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0475-x