Abstract
Hepatocellular carcinoma (HCC) is the most common primary liver cancer, representing the sixth leading cause of cancer and the third leading cause of cancer-related mortality. Patient stratification and treatment allocation are based on tumour stage, liver function, and performance status. About 80% of patients with HCC are diagnosed with disease that is not amenable to liver transplantation or surgical resection. A majority of patients with unresectable HCC are referred for image-guided locoregional therapies. These interventional treatments include intra-arterial chemotherapy (IAC), transarterial embolization (TAE), transarterial chemoembolization (TACE) with or without drug-eluting beads (DEBs), and radioembolization using embolic particles loaded with a radioisotope, most commonly Yttrium-90. The main goal of these therapies is to cause an ischemic/hypoxic environment and, consequently, coagulative necrosis in the tumour by delivering selectively chemotherapeutic drugs to the tumour-feeding arteries. The anticancer effect of all embolization procedures is based on terminal arterial blockade and subsequent tumour ischemia. These therapies are accepted treatment modalities for providing survival benefit in selected patient populations. In this chapter, we describe the rationale behind IAC, TAE, conventional transarterial chemoembolization (cTACE), and transarterial chemoembolization (TACE) with drug-eluting beads (DEBs) and provide a review of the existing medical literature regarding the current clinical evidence of safety and efficacy of these therapies, critical appraisal of patient selection, comparison of cTACE and DEB-TACE, and TACE and systemic therapy/immunotherapy combination. Additionally, a brief summary about the TACE implementation in the Middle East countries based on literature screening from PubMed is provided.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hepatocellular carcinoma
- Locoregional therapies
- Intra-arterial chemotherapy
- Transarterial embolization
- Transarterial chemoembolization
- Conventional transarterial chemoembolization
- Transarterial chemoembolization with drug-eluting beads
1 Introduction
Transcatheter intra-arterial therapies are image-guided locoregional therapies mostly used in the interventional radiology for the treatment of patients with primary and metastatic tumours, most commonly localized in the liver [1]. These therapies include intra-arterial chemotherapy (IAC), transarterial embolization (TAE), transarterial chemoembolization (TACE) with or without drug-eluting beads (DEBs), and radioembolization using embolic particles loaded with a radioisotope, most commonly Yttrium-90. The main goal of these therapies is to cause an ischemic/hypoxic environment and, consequently, coagulative necrosis in the tumour by delivering selectively chemotherapeutic drugs to the tumour-feeding arteries. The anticancer effect of all embolization procedures is based on terminal arterial blockade and subsequent tumour ischemia. IAC consists of intra-arterial infusion of the chemotherapeutic drugs by selective catheterization of the hepatic artery targeting the delivery of high concentrations of chemotherapeutic drugs directly to the tumour. TACE (with or without drug-eluting beads) combines targeted chemotherapeutic drug delivery with simultaneous embolization of the tumour-feeding artery. Transarterial radioembolization integrates delivery of internal radiation to the tumour with minimal embolic effect unlike other embolization treatments. These therapies are accepted treatment modalities for providing survival benefit in selected patient populations. In this chapter, we describe the rationale behind of IAC, TAE, conventional transarterial chemoembolization (cTACE), and transarterial chemoembolization (TACE) with drug-eluting beads (DEBs) and provide a review of the existing medical literature. Transarterial radioembolization is beyond the scope of this chapter.
2 Intra-arterial Chemotherapy: Rationale and Overview
IAC is a minimally invasive percutaneous image-guided radiologic procedure with employing angiographic catheter as a conduit to achieve a higher local concentration of chemotherapeutic agents to the targeted unresectable tumour with fewer significant systemic side effects [2]. The rationale for regional chemotherapy is to maximize drug concentrations and tumour drug uptake in the target organ and minimize systemic toxicity [3]. For successful IAC, several important principles regarding tumour biology, drug pharmacology, and delivery systems must be fulfilled [4]. These concepts are that (1) locoregional delivery of chemotherapeutic agent leads to increased local concentration of the drug, (2) increased locoregional concentration of the drug leads to increased therapeutic response, and (3) locoregional drug delivery leads to decreased systemic exposure of the used drug. Several variations of this technique are available, and no standard protocol has been uniformly adopted. Many centres have differed in the choice and/or dose of the anticancer agents used, treatment end points, and the schedule and/or interval of retreatment.
3 Intra-arterial Chemotherapy: Clinical Evidence of Safety and Efficacy
The results of IAC have been studied most extensively in patients with colorectal cancer and unresectable liver metastases . The role of TAC outside of metastatic colorectal cancer has been less researched. Okusaka et al. [3] published findings of the randomized phase III trial comparing TAC and TACE for the treatment of patients with unresectable HCC. In this prospective 161-patient study, there was no significant difference when the median overall survival time was compared between these two therapies. IAC produced less tumour necrosis than TACE, particularly in tumours more than 3 cm. The important thing is that the Barcelona Clinic Liver Cancer staging classification and treatment schedule [5], a worldwide used staging system for HCC management, does not include IAC in its algorithm of the treatment options for HCC. Also, the American Association for the Study of Liver Disease practice guidelines [6] did not recommend systemic or selective intra-arterial chemotherapy and warn not to use these treatment methods as standard of care. However, in Japan, TAC has traditionally been used to treat patients with advanced HCC with vascular invasion or multiple intrahepatic lesions or both [7].
4 Transarterial Embolization: An Overview
TAE (also known as bland embolization) is a minimally invasive image-guided procedure performed with the aim to restrict the tumour’s blood supply by delivering particles which do not contain a chemotherapeutic or radioactive agent. In the context of treating an HCC tumour with TAE, polyvinyl alcohol particles or gelatin-based microspheres are used most commonly, although alcohol with ethiodized oil and gelatin sponge has also been described [8]. Deficiency of arterial flow results in an ischemic/hypoxic environment and, consequently, coagulative necrosis in the tumour . The embolic agent can also potentially incite a localized inflammatory reaction and focal angionecrosis [9]. The therapeutic end point of TAE is the stasis of flow in the arteries supplying the tumour with pruning of the distal branches of the treated artery. The targeted tumoral arterial supply is interrupted with an embolic agent, most commonly microparticles ranging from 40 to 120 μm in size [10]. Depending on the disease distribution within the liver, the treatment approach can vary including lobar treatment for multifocal disease or targeted segmental treatment for unifocal disease [8]. The most common associated risk is that of postembolization syndrome, the severity and duration of which might be correlated with the degree of healthy tissue ischemia and underlying liver function [11]. The use of novel intraprocedural technologies such as cone-beam CT is utilized to ensure complete tumoral coverage while avoiding nontarget embolization [12]. TAE is reserved for nonsurgical candidates with liver-dominant disease. Studies have demonstrated that HCC patients in stage B of the Barcelona Clinic Liver Cancer staging classification system derive the most benefit from this procedure followed by stage C [13]. Patients in BCLC stage A may undergo TAE to maintain eligibility for transplantation per the Milan and University of California, San Francisco criteria [14]. The contraindications for TAE include decompensated cirrhosis (Child-Pugh B8 or higher), significantly reduced portal venous flow, creatinine clearance <30 mL/min, high tumour burden, severe comorbidities, untreated oesophageal varices, and elevated liver function markers [15].
5 Transarterial Embolization: Clinical Evidence of Safety and Efficacy
Llovet et al. [13] reported that TAE confers significant survival benefit compared to best supportive care. Tsochatzis et al. [14] published results from a meta-analysis of six randomized controlled trials comparing TACE with TAE, and none of them revealed significant differences in overall survival. Lee et al. [15] summarized evidence from three studies revealing no significant differences in 3-year survival rates, adverse events, or RECIST responses. Kluger et al. [16] found that TAE patients were significantly less likely to require retreatment before transplantation than TACE patients. Malagari et al. [17], in the prospective randomized comparison of chemoembolization with doxorubicin-eluting beads and bland embolization with Bead Block (Boston Scientific, Marlborough, MA) for HCC, found significant improvement in time-to-progression in the DEB-TACE group, but no change in overall survival.
Since induced ischemia from embolotherapy could be the dominant contributor to tumour cell death and bland embolization does spare the cost of chemotherapy and its toxicity profile, TAE should continue to be offered to appropriately selected patients.
6 Transarterial Chemoembolizations: An Overview
TACE is a minimally invasive image-guided procedure performed with the aim to restrict a tumour’s blood supply. According to the Society of Interventional Radiology guidelines [18], chemoembolization is currently defined as the infusion of a mixture of chemotherapeutic agents with or without iodized oil, followed by embolization with particles. During TACE, embolic particles with or without chemotherapeutic drugs are injected through an angiographic catheter directly into a tumour-feeding artery. There are two main mechanisms enabling TACE in patients with HCC. The carcinogenesis of HCC is a multistep process that leads to a gradual shift in tumour blood supply from predominantly portal to predominantly arterial circulation. Due to the predominately arterial feeding of HCC, transarterial embolization interrupts the tumour’s blood supply and slows down or stops the growth of the tumour [19]. Additionally, targeted administration of chemotherapeutic agents allows delivery of a higher dose to the tumour’s tissue while simultaneously reducing exposure for the liver parenchyma. After transarterial embolization, chemotherapeutic drugs are not washed out from the occluded tumour’s vessels that results in a higher concentration of drugs within the tumour with a longer period of the exposure to the cytotoxic effect. An ischemic necrosis induced by embolization causes a failure of the transmembrane pump, resulting in a greater absorption of tumoricidal agents by the tumour cells . Thus, the concentration of the agents within the tumour can be 40 times greater than that of the surrounding normal liver parenchyma [20]. As a consequence of the above, TACE selectively targets the tumour while normal liver is relatively preserved. According to the Barcelona Clinic Liver Cancer (BCLC) staging system [5], TACE is the first-line treatment for intermediate-stage disease, which includes asymptomatic patients with well-preserved liver function and limited to liver large or multifocal tumours and without macrovascular invasion or extrahepatic spread. For these patients, TACE is recognized as a treatment with proven survival effect on survival [13, 21, 22]. The BCLC system also recommends a treatment migration concept in that TACE should be used in patients with early-stage HCC in whom the recommended treatments are not feasible or have failed [5]. The use of TACE was also supported by other staging systems such as the Chinese University Prognostic Index [23], the Hong Kong Liver Cancer staging system [24], and the Japanese Integrated Staging scoring system [25]. There are two TACE techniques [1, 26], namely conventional TACE (cTACE), which uses a mixture of a chemotherapeutic agent with Lipiodol, and TACE with DEBs (DEB-TACE) which will be reviewed further separately.
7 Critical Appraisal of Patient Selection for TACE
Patient selection is crucial for the success of TACE [26]. The exclusion of absolute contraindications should always be the first step in the assessment of patient suitability for TACE. Absolute and relative contraindications include features of decompensated liver disease, extensive bilobar tumour load and impaired integrity of the portal vein, as well as untreated large varices, huge tumour size, and severe comorbidities [27, 28]. However, patients with moderate to severe hepatic insufficiency can still be treated with TACE if embolization is performed segmentally or sub-segmentally, targeting a small volume of the liver. The presence of segmental or sub-segmental portal vein invasion is acceptable for cTACE if only injection of the drug/Lipiodol emulsion without particulate embolization is performed in the portion of the liver parenchyma deprived of portal venous flow and particulate embolization is delivered only into the tumour-feeding arteries. This approach ensures that non-tumoural liver tissue can still rely on adequate arterial flow [29].
Accepted absolute contraindications for TACE are summarized as follows [19, 26,27,28]:
-
Eastern Cooperative Oncology Group [30] Patient Performance Status >1
-
Decompensated liver cirrhosis (Child-Pugh class B, score >8) with jaundice, clinically significant hepatic encephalopathy, refractory to treatment ascites, and/or hepatorenal syndrome
-
Impaired portal venous circulation due to portal vein thrombosis or high portal hypertension with hepatofugal blood flow
-
Extensive tumour involving both lobes of the liver
-
Main portal vein tumour thrombosis
-
Untreatable intrahepatic arteriovenous fistula
-
Impaired renal function
-
Active systemic infection
-
Uncorrectable bleeding disorder
-
Previous shock related to contrast media
Accepted relative contraindications for TACE are summarized as follows [19, 26,27,28]:
-
Presence of oesophageal varices with high risk of bleeding
-
Tumour larger than 10 cm
-
Severe comorbidities
-
Incompetent papilla with aerobilia
-
Biliary dilatation
8 Conventional Transarterial Chemotherapy: An Overview
cTACE involves the imaging-guided intra-arterial injection of a cytotoxic drug, such as cisplatin, doxorubicin, epirubicin , idarubicin, or mitomycin C, which is emulsified in the Lipiodol, into tumour-feeding artery thorough angiographic catheter. Lipiodol, also known as ethiodized oil, is a poppy-seed oil used by injection as a radiopaque contrast agent (Lipiodol® Ultra-Fluid; Guerbet, Villepinte, France). Intra-arterial injection of cytotoxic drug is followed by intra-arterial injection of an embolic agent, such as Gelfoam, polyvinyl alcohol, or acrylic copolymer gelatin particles [31]. During cTACE, Lipiodol carries and delivers chemotherapeutic agents to the tumour and causes embolization of the tumour microcirculation [32, 33]. cTACE is the current standard of care for large or multinodular tumours isolated to the liver for patients with preserved liver function and absence of portal vein invasion [34]. cTACE use has been reported in patients with more advanced HCC, such as microvascular or macrovascular invasion, or limited extrahepatic disease with adequately preserved hepatic function [35]. cTACE is also used in patients with early-stage HCC as a bridge to liver transplantation or for patients not eligible for liver transplantation, hepatic resection, and ablation [5]. cTACE is the recommended standard of care for the treatment of intermediate-stage HCC in most current international guidelines [34, 36]. A recent systematic review of cTACE efficacy that comprised a total of 10,108 HCC patients found that the median overall survival was 19.4 months and that the 5-year survival rate was 32.4% [37]. Despite these facts, some important limitations remain. One of the issues of cTACE is the huge heterogeneity of the techniques and schedules used in clinical practice. Further differences exist with regard to the selectivity of TACE (lobar versus segmental versus super-selective), which has been reported to be an important determinant of procedure tolerance and efficacy [38]. To deal with these limitations, a worldwide expert panel published consensus technical recommendations in order to encourage cTACE standardization [29].
The most important recommendations of the worldwide expert panel [18] are summarized below:
-
Eastern European Oncology Group [30] Patient Performance Status to be 0
-
Multiphasic computed tomography (CT) or dynamic contrast-enhanced magnetic resonance imaging (MRI) of the liver as the preferred modalities for the treatment allocation
-
Cone-beam CT use for the tumour visualization, targeting , and assessment of treatment completion
-
Doxorubicin (50–75 mg/m2) or cisplatin (50–100 mg/m2) as the most proven chemotherapeutic agent
-
Preparing water-in-oil emulsion (aqueous chemotherapy droplets in internal phase and Lipiodol in continuous external phase) to improve tumour deposition
-
Gelatine sponge use with 100–300 microns-sized calibrated microspheres with the aim to occlude distal vessels with preservation of feeding segmental arteries
-
Super-selective approach with microcatheter for treating a single tumour or small number of tumours
-
Lipiodol opacification of the small arterioportal sinusoids as a predictive factor for tumour response and local recurrence [39]
-
Assessing tumour viability using the mRECIST criteria [40]
-
At least two cTACE procedures 2–8 weeks apart in order to ensure a presence or absence of the tumour response
9 Conventional TACE: Clinical Evidence of Safety and Efficacy
cTACE has been established as the standard treatment for intermediate-stage HCC without portal vein invasion in consequences of two randomized controlled trial studies, which used either doxorubicin [13] or cisplatin [21] mixed with Lipiodol. These studies represent the only level 1 evidence for intra-arterial therapies for HCC demonstrating the superiority of cTACE over best supportive care. Regarding the safety of cTACE, symptoms related to postembolization syndrome (fever, nausea, and abdominal pain) may be observed in up to 80% of patients and were generally mild, transient, and manageable. The most common complications included liver failure, cholecystitis , gastrointestinal bleeding, ascites, and encephalopathy. Treatment-related death rates varied between 0% and 6% [41]. It is less likely to see deteriorated quality of life after TACE [42]. A multicentre prospective Asian cooperative study on intermediate-stage HCC patients treated with cTACE reported a median survival time and 1- and 2-year survival rates of 3.1 year and 89.6 and 75.0%, respectively [43]. cTACE has been reported in patients with more advanced HCC, such as macrovascular invasion or limited extrahepatic disease with adequately preserved hepatic function. In the prospective non-randomized study, HCC patients with segmental or sub-segmental portal vein invasion were treated with cTACE or conservative care according to the patient’s preference. The 12- and 24-month OS rates for the cTACE and conservative groups were 30.9%, 9.2%, and 3.8%, 0%, respectively (p < 0.001) [35]. In the USA, cTACE is also used in patients with early-stage HCC as a bridge to liver transplantation or when liver transplantation, hepatic resection, and image-guided ablation are not possible [44].
10 Transarterial Chemoembolization with Drug-Eluting Beads: An Overview
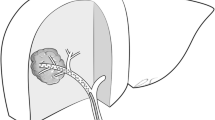
DEB-TACE, a different transarterial drug delivery technique , involves the intra-arterial injection of DEBs loaded with various types of chemotherapeutic agents [45]. DEBs are non-resorbable embolic microspheres loaded with a chemotherapeutic agent with the ability of slow drug release, which should ensure high local and low systemic drug concentrations. DEB-TACE was primarily developed to enhance the delivery of the chemotherapeutic agent while minimizing systemic toxicity and to provide a standardized embolizing effect. Commercialized DEBs are composed of various hydrophilic ionic polymers that can bind to anthracycline drugs via an ion exchange mechanism. Several microsphere diameters are available, ranging from 40 to 900 μm. The unique properties of these beads, and therefore of this transarterial drug delivery system, allow the fixing drug doses and the ability to release the chemotherapeutic agents in a sustained and controlled manner . Different microspheres are available for DEB-TACE . DC Bead (BTG International, London, UK) is a relatively new drug delivery embolization system comprising a range of hydrogel microspheres that are biocompatible, hydrophilic, non-resorbable, and precisely calibrated. DC Beads are available in four different ranges – 70–150 μm, 100–300 μm, 300–500 μm, and 500–700 μm – with drug loadings varying from 5 to 45 mg/mL hydrated beads. HepaSphere (MeritMedical, MA) is a biocompatible, non-resorbable, expandable, and loadable microsphere. The HepaSphere beads are available in a range of sizes: 30–60 μm, 50–100 μm, 100–150 μm, and 150–200 μm. TANDEM microspheres (CeloNova Biosciences/Boston Scientific, MA) (Fig. 1a–c) are non-resorbable polymethacrylate hydrogel that are available in three sizes: 40 ± 10 μm, 75 ± 15 μm, and 100 ± 25 μm. LifePearl (Terumo Corporation, Tokyo, Japan) are polyethylene glycol embolization microspheres that can be loaded with chemotherapeutic agents (such as doxorubicin, irinotecan, idarubicin, and epirubicin). LifePearl microspheres offer a wide range of drug loading options, enhanced suspension characteristics, and tight calibration. LifePearl microspheres are available in three sizes: 100 ± 25 μm, 200 ± 50 μm, and 400 ± 50 μm. DC Bead LUMI (BTG International, London, UK) (Fig. 2a–e) is radiopaque, biocompatible, non-resorbable hydrogel beads, produced from polyvinyl alcohol-like conventional DC Bead, but incorporating a tri-iodobenzyl radiopaque moiety with a covalent bond. DC Bead LUMI is designed to be inherently radiopaque and thus perfectly visible under X-ray-based imaging modalities, such as CT, cone-beam CT, and fluoroscopy . DC Bead LUMI is available in three size ranges: 70–150 μm, 100–300 μm, and 300–500 μm.
(a) T2-weighted magnetic resonance imaging demonstrated histologically proven hepatocellular carcinoma in the right lobe of the liver in 73-year-old female patient later treated with DEB-TACE using TANDEM 40 μm microspheres loaded with doxorubicin. (b) Contrast-enhanced magnetic resonance imaging demonstrated hypervascular hepatocellular carcinoma in the same patient before treatment. (c) Contrast-enhanced magnetic resonance imaging demonstrated avascular and shrunken tumour in the same patient 3 years after the treatment . These findings were evaluated as complete response according to mRECIST criteria
(a) T2-weighted fat saturated magnetic resonance imaging demonstrated hepatocellular carcinoma in the right lobe of the liver in a 69-year-old male patient later treated with DEB-TACE using DC Bead LUMI 70–150 μm microspheres loaded with doxorubicin. (b) Contrast-enhanced magnetic resonance imaging demonstrated hypervascular hepatocellular carcinoma in the same patient before treatment. (c) Non-contrast computed tomography performed the day after the treatment with DC Bead LUMI demonstrated distribution of the radiopaque microspheres within the tumour in the same patient. (d) Non-contrast computed tomography performed 1 week after the treatment with DC Bead LUMI demonstrated distribution of the radiopaque microspheres within the tumour in the same patient. (e) Control contrast-enhanced magnetic resonance imaging demonstrated avascular and shrunken tumour in the same patient 19 months after the treatment. These findings were evaluated as complete response according to mRECIST criteria
11 Transarterial Chemoembolization with Drug-Eluting Beads: Clinical Evidence of Safety and Efficacy
Safety and efficacy of DEB-TACE have become the object of a number of studies. Generally, safety and efficacy of DEB-TACE were evaluated by the randomized European Precision V phase II trial in 212 patients with predominately intermediate-stage HCC [28], and a post hoc comparison showed a significant reduction in drug-related systemic and liver toxicity. Grosso et al. [46] published initial results of a multicentre trial that employed HepaSphere microspheres loaded with doxorubicin or epirubicin to treat 50 patients with unresectable HCC. The technical success was achieved in all cases, and no major complications were experienced. The authors evaluated tumour response 1 and 6 months after the procedure, observing an objective response rate of 84 and 77.4%, respectively, at the first and second follow-up time points. Therefore, they concluded that DEB-TACE using HepaSphere is a feasible, effective, and safe procedure. Malagari et al. [47] reported similar promising midterm outcomes using doxorubicin-loaded DC beads as treatment of 3–10 cm HCCs in 71 patients. Overall survival at 12, 18, 24, and 30 months was 97.05%, 94.1%, 91.1%, and 88.2%, respectively. Sustained overall survival was seen in 66.2% of patients. Despite postembolization syndrome being observed in all patients, the rate of severe procedure-related complications was just 4.2%. Therefore, authors stated that DEB-TACE with DC Bead is an effective and safe procedure in the treatment of HCC with high rates of response and midterm survival. Spreafico et al. [48] reported a study with the aim to evaluate the short-term safety and efficacy of the 70–150 μm DC BeadM1 loaded with doxorubicin in 45 patients with HCC undergoing DEB-TACE as a primary therapy or as a bridge to liver transplantation. The authors reported an OR rate of 77.7% and a grade 3/4 adverse event rate as low as 1.5%. Moreover, pathology demonstrated that 35% of the treated nodules presented a coagulative necrosis area larger than 90% of their volume. Thus, the authors concluded that DEB-TACE with DC BeadM1 is an effective and safe procedure, providing either tumour downstaging or necrosis. Two different prospective studies that investigated the potential role of DEB-TACE, experiencing the use of both HepaSphere 30–60 μm [49] and TANDEM [50], reported good response rates in both cases: the OR was 68.9% in the HepaSphere study and 61.3% in the TANDEM study. Recently, Greco et al. [51] achieved encouraging results in terms of tumour response using 40 μm Embozene TANDEM particles with overall response of 72.6%. Richter et al. [52] in the MIRACLE I prospective multicentre study reported similar results using 75 μm Embozene TANDEM particles with a higher overall response as 95%. Balli et al. [53] demonstrated that super-selective DEB-TACE with doxorubicin-loaded beads sized 40–75 μm was an effective and safe treatment method with prolonged time-to-progression and progression-free survival in early and intermediate stages of HCC. An analysis concerning the particles size was performed by Prajapati et al. [54] who retrospectively compared the overall survival, efficacy, and safety of small (100–300 μm) and large (300–500 and 500–700 μm) DEB-TACE beads in two groups of patients with unresectable HCC. The authors found that the use of 100–300-μm-sized particles was linked with significantly higher survival rate and lower complications than the employment of 300–500 and 500–700-μm-sized DEBs. In another retrospective comparative study, Balli et al. [55] reported a higher response rates, prolonged overall survival, and progression-free survival after DEB-TACE performed with doxorubicin-loaded microspheres sized below 100 μm than in above 100 μm patient group. In conclusion, these findings underline that implementation of DEB-TACE may be further increased by the adoption of small particle sizes.
12 Comparison of Conventional Transarterial Chemoembolization and Transarterial Chemoembolization with Drug-Eluting Beads
Both cTACE and DEB-TACE have been considered as the standard treatment for unresectable HCC. DEB-TACE ensures the loaded chemotherapeutic agent slowly releases to achieve a lower systemic drug peak compared to cTACE [56]. DEB-TACE was expected to improve the performance of conventional cTACE. Two retrospective studies [57, 58] have suggested the superiority of DEB-TACE, whereas other comparative studies have not confirmed this superiority. Idilman et al. [59] reported that no differences in survival or side effects were observed between the cTACE and DEB-TACE in their retrospective study. In a large comparative study of Western HCC patients, Facciorusso et al. [60] demonstrated that drug-eluting bead chemoembolization with 100–300 μm particles did not seem to improve survival in comparison with conventional chemoembolization, which in turn provided better tumour responses and time-to-progression. Moreover, the randomized controlled trial of DEB-TACE versus cTACE for HCC performed by PRECISION Italia Study Group [61] showed that adverse effect incidence and severity did not differ between the arms, except for post-procedural pain, more frequent and severe after cTACE (P < 0.001). The 1- and 2-year survival rates were 86.2% and 56.8% after DEB-TACE and 83.5% and 55.4% after cTACE (P = 0.949). Thus, the authors stated that DEB-TACE and the cTACE are equally effective and safe, with the only advantage of DEB-TACE being less post-procedural abdominal pain. Additionally, Karalli et al. [62], in their retrospective real-life analysis, reported that DEB-TACE had better tolerability compared to cTACE, but overall survival did not differ between the two treatments. Zhang et al. [63] also demonstrated that compared to cTACE, DEB-TACE offered slightly better disease control rate and tolerability for HCC patients. However, DEB-TACE does not provide higher progression-free survival than cTACE.
Two meta-analyses [64, 65] and one systematic review [66] regarding comparability or superiority of cTACE and DEB-TACE were recently published. In the first meta-analysis performed by Facciorusso et al. [64], 4 randomized controlled trials and 8 observational studies with 1449 patients were evaluated. Non-significant trends in favour of DEB-TACE were observed as for 1-year (odds ratio: 0.76, 0.48–1.21, p = 0.25), 2-year (odds ratio: 0.68, 0.42–1.12, p = 0.13), and 3-year survival (odds ratio: 0.57, 0.32–1.01, p = 0.06). Meta-analysis of plotted hazard ratios confirmed this trend (hazard ratio: 0.86, 0.71–1.03, p = 0.10). Pooled data of objective response showed no significant difference between cTACE and DEB-TACE (odds ratio: 1.21, 0.69–2.12, p = 0.51). No statistically significant difference in adverse events was registered (odds ratio: 0.85, 0.60–1.20, p = 0.36). Based on these results, the authors stated that results of performed meta-analysis stand for a non-superiority of DEB-TACE with respect to cTACE in HCC patients. In the second meta-analysis regarding comparability of cTACE and DEB-TACE [65], no significant difference was found in overall response at 3, 6, 9, and 12 months, complete response, partial response, disease control rate, stable disease, overall survival, and complications between cTACE and DEB-TACE. The authors stated that DEB-TACE had similar therapeutic effects to those of cTACE. Furthermore, major complications in both therapies were similar; thus, the authors concluded that superiority of DEB-TACE over cTACE remains unclear, and further research with high-quality evidence is needed. However, in the recently published systematic review, Yang et al. [66] evaluated the effects of DEB-TACE, TARE, and cTACE in terms of overall survival , tumour response, and complications. The authors found that DEB-TACE had a better overall survival at 1 year (p = 0.006), 2 years (p = 0.046), and 3 years (p = 0.035) when compared with cTACE.
In conclusion, despite the theoretical advantages of DEB-TACE over cTACE, it is still controversial as to whether DEB-TACE is superior to cTACE in terms of efficacy. However, it seems that DEB-TACE shows at least similar clinical outcomes and less adverse events than cTACE. Further organized prospective studies are required to identify combination strategies and to develop better treatment approaches for patients with HCC.
13 Future Directions: Transarterial Chemoembolization and Systemic Therapy Combination
TACE has been established as the most widely used therapeutic intervention for patients with intermediate-stage HCC. Despite level 1 evidence of survival benefit for TACE in BCLC stage B, it remains a palliative treatment. This may be explained by the hypoxic environment created by the TACE procedure, which can induce neoangiogenesis by stimulating vascular endothelial growth factor and other angiogenic pathways, promoting revascularization and growth of residual viable tumour [5, 67]. In an effort to address this problem, many studies have been conducted combining TACE with systemic anti-angiogenic agents, most commonly sorafenib (Nexavar; Bayer AG, Leverkusen, Germany), based on its proven activity against advanced HCC. The GIDEON trial [68] was an observational registry of 3202 patients with HCC of BCLC A, B, and C stages treated with sorafenib alone or in combination with TACE. Adverse events were reported in 2732 (85.3%) patients overall, with no notable differences in the incidence of adverse events, regardless of TACE treatment history. Overall survival was 12.7 months in prior TACE patients, 9.2 months in non-prior TACE patients, 21.6 months in concomitant TACE patients, and 9.7 months in non-concomitant TACE patients. The authors stated that the combination of TACE with sorafenib appears to be a well-tolerated and viable therapeutic approach. The SPACE trial [69], a prospective randomized phase II trial in patients with BCLC stage B HCC, included 307 patients allocated randomly to DEB-TACE with sorafenib and DEB-TACE with placebo. There was no difference in TTP between the two arms (169 vs. 166 days in the sorafenib and placebo arms, respectively, p = 0.072). Overall the trial had a negative outcome with no impact on overall survival (p = 0.29). A further subgroup analysis from the SPACE trial suggested that patients with more advanced disease could benefit more than those with intermediate-stage disease [70]. In a phase III trial of TACE with sorafenib (TACE-2) [71], 313 patients were randomized to sorafenib or placebo with DEB-TACE 2–5 weeks later and additional TACE on demand. This trial reported no significant difference regarding a median progression-free survival (7.9 vs. 7.8 months in the sorafenib and placebo arms, respectively, p = 0.94) and median overall survival (21.1 and 19.7 months in the sorafenib and placebo groups, respectively, p = 0.57). In the phase III STAH trial [72], 169 patients were randomized to sorafenib alone or sorafenib combined with cTACE within 7–21 days of randomization. Compared with sorafenib alone, sorafenib combined with cTACE did not improve overall survival in patients with advanced HCC. However, sorafenib combined with cTACE significantly improved time-to-progression, progression-free survival, and tumour response rate. For combined treatment and sorafenib alone, median time-to-progression was 5.3 and 3.5 months, respectively (p = 0.003); median progression-free survival was 5.2 and 3.6 months, respectively (p = 0.01); and median overall survival was 12.8 and 10.8 months, respectively (p = 0.290). The authors stated that sorafenib alone remains the first-line standard of care for patients with advanced HCC. Kudo et al. [73], in the randomized, multicentre prospective TACTICS trial, compared the efficacy and safety of TACE plus sorafenib with TACE alone using a newly established TACE-specific end point and pretreatment of sorafenib before initial TACE. Patients in the combination group received sorafenib 400 mg once daily for 2–3 weeks before TACE, followed by 800 mg once daily during on-demand cTACE sessions until time to untreatable progression, defined as untreatable tumour progression, transient deterioration to Child-Pugh C, or appearance of vascular invasion/extrahepatic spread. Median progression-free survival was significantly longer in the TACE plus sorafenib than in the TACE alone group (25.2 vs. 13.5 months; p = 0.006). Overall survival was not analysed because only 73.6% of overall survival events were reached. Median time to untreatable progression (26.7 vs. 20.6 months; p = 0.02) was also significantly longer in the TACE plus sorafenib group. Overall survival at 1 year and 2 years in TACE plus sorafenib group and TACE alone group were 96.2% and 82.7% and 77.2% and 64.6%, respectively. The authors stated that TACE plus sorafenib significantly improved progression-free survival over TACE alone in patients with unresectable HCC. Meta-analyses [74, 75] of TACE in combination with sorafenib have reported improved time-to-progression in patients with a combination; however, the addition of sorafenib failed to improve significantly in overall survival compared to TACE alone. In conclusion, a number of clinical trials inquiring addition of sorafenib to TACE did not demonstrate any significant improvement of overall survival due to addition of sorafenib to TACE for patients with intermediate-stage HCC.
Another systemic agent (bevacizumab; Roche Diagnostics GmbH, Mannheim, Germany) was tested in combination with TACE . Pinter et al. [76], in a randomized phase II study investigating the addition of bevacizumab to TACE, reported no evidence of increased efficacy assessed by radiological response rate. Smolka et al. [77], in the study comparing TACE + bevacizumab to TACE alone, reported that bevacizumab did not change quantitative tumour response to TACE. Briefly, the combination of TACE with anti-angiogenic drugs has been disappointing in terms of survival outcomes; however, due to potential safety, further studies are warranted in patients with advanced HCC.
14 Future Directions: Transarterial Chemoembolization and Immunotherapy Combination
A substantial body of evidence supports the development of immunotherapy to treat HCC. It is logical to combine TACE therapy with checkpoint inhibitors because the tumour burden will be less than in patients with advanced disease; checkpoint inhibitors will be administered in a immunogenic environment with probability of overcoming local tumour-mediated immune suppression; and both TACE and checkpoint inhibitors have been shown to stimulate immune responses against HCC [78] . Experiments in immunotherapy such immune checkpoint inhibitors are also underway. Several combination strategies of immunotherapies with thermal ablations and cryoablation were investigated in vitro and in animal models of HCC [79]. Recently, Marinelli et al. [80] investigated the safety of locoregional treatment (transarterial chemoembolization or Yttrium-90 transarterial radioembolization) combined with nivolumab for intermediate and advanced hepatocellular carcinoma (HCC) . The authors reported that during a median follow-up of 11.5 months (range, 1.8–35.1), no grade III/IV adverse events attributable to nivolumab were observed. In addition, there were no nivolumab-related deaths, and 30-day mortality after LRT was 0%. Thus, the authors demonstrate that locoregional treatment performed concomitantly with nivolumab immunotherapy had an acceptable safety profile in patients with intermediate and advanced HCC. In conclusion, current evidences suggest that the combination of systemic treatments and TACE seems to be a relatively safe option for treating patients with advanced disease. More studies are necessary to produce solid data over a longer follow-up period.
15 Current Implementation of Transarterial Chemoembolization in the Middle East Countries
We aimed to report a brief summary about the TACE implementation in the Middle East countries based on literature screening from PubMed. Indeed, it is not possible to describe all articles; thus, only newest investigations from the last 5 years were included into this brief literature review. Zaky et al. [81] evaluated the short-term outcome of the decision, taken by the multidisciplinary tumour board for the treatment of HCC patients with surgical resection, local ablative therapy, cTACE, and palliative supportive care. The authors found that the management of HCC was better performed through a multidisciplinary team decision, and cTACE has a success rate of 33.3%. El Sherbiny et al. [82] investigated changes in Doppler parameters of portal pressure after interventional management of HCC, including TACE, and reported improved portal hypertension parameters after TACE. The authors recommended Doppler ultrasound use as a reliable and effective method of evaluation of portal hypertension after TACE for HCC. Abdelmaksoud et al. [83] evaluated the prognostic factors and management in patients with HCC with portal vein thrombosis. The authors reported a significantly worse prognosis in patients with more than two tumours, abdominal lymphadenopathy, and serum bilirubin >2 mg/dL. Additionally, specific treatment significantly increased survival compared to patients left untreated (p = 0.027). Thus, TACE was considered as a promising procedure for unresectable portal vein thrombosis-associated HCCs. Abdelaziz et al. [84] studied a combined ablation techniques and assess survival benefit comparing TACE with radiofrequency versus TACE with microwave ablation techniques. A higher tendency to provide complete response rates after TACE with microwave ablation comparing with TACE with radiofrequency ablation was reported (p = 0.06). This was particularly evident with lesions sized 3–5 cm (p = 0.01). Rates of complications showed no significant difference between the groups. The authors concluded that TACE with microwave ablation led to better response rates with tumours 3–5 cm, with no difference in survival rates. Moustafa et al. [85] reviewed the factors influencing the development of an extrahepatic collateral arterial blood supply to HCC and described a systematic approach to enhance the ability to predict the presence of extrahepatic collateral arteries. They also describe the proper technique for TACE of each extrahepatic collateral artery and how to avoid potential technique-related complications. Abdella et al. [86] assessed the outcomes after TACE in patients with segmental portal vein thrombosis regarding Child-Pugh classification, radiological response, and 1-year survival. TACE succeeded to achieve disease control in 93.3%, 86.3%, 57.7%, and 44.4% of patients after 1, 3, 6, and 12 months, respectively. Post-TACE liver decompensation occurred in the form of ascites in 30%, jaundice in 10%, and hepatic encephalopathy in 3.3% within 1 month of TACE. One-month survival after TACE was 100%, 3 months was 96.6%, 6 months was 86.6%, and 1 year was 60%. Mean overall survival of the included patients was 17 months (s.e. = 1.59). The authors concluded that TACE seems an alternative option for unrespectable HCC with portal vein thrombosis in patients with preserved liver function. Hassan et al. [87] evaluated the frequency of regulatory T cells and serum levels of IL-6 and IL-10 before and after TACE. HCC patients had a significantly higher level of IL-6 and IL-10 when compared to the control group (p = 0.0002, p < 0.0001), respectively. However, after treatment, there was an elevation in the levels of IL-6 and IL10 followed by a decrease to the baseline levels. Patients with large tumours (≥5 cm) showed higher levels of both IL-6 and IL-10 than those with smaller tumours. Moreover, HCC patients showed a higher frequency of regulatory T cells in comparison with the controls (p = 0.002). No significant correlation was observed between the frequency of regulatory T cells and IL-10 before and after treatment (r = 0.38, p = 0.30). The authors concluded that HCC patients have significantly higher levels of IL-6 and IL-10 and a higher percentage of regulatory T cells than controls; the regulatory T-cell levels were altered after chemoembolization; and IL-6 have a potential in reflecting the patient’s condition after treatment, thus helping in monitoring therapy. Khalid et al. [88] investigated the prognostic value of the albumin-bilirubin grade in patients undergoing TACE for unresectable HCC. The mean duration of survival at the last follow-up was of 12.1 ± 12.14 months (range 1–49). Univariate analysis showed serum albumin (p = 0.003), serum bilirubin (p = 0.018), Child-Pugh score (p = 0.019), albumin-bilirubin grade (p = 0.001), and presence of varices (p = 0.04) to be the main predictors of 6-month survival after TACE. On Cox analysis, only ALBI score (p = 0.038) showed statistical significant association. The authors concluded that albumin-bilirubin grade may serve as a surrogate marker in predicting the prognosis of HCC patients undergoing TACE. Hassan et al. [89] evaluated the role of diffusion-weighted magnetic resonance imaging in the detection of residual HCC after DEB-TACE. Diffusion-weighted magnetic resonance imaging had a sensitivity of 77.1%, a specificity of 60.7%, a positive predictive value of 71.05%, and a negative predictive value of 68%. The difference between the malignant and benign groups’ ADC variables was statistically significant (p < 0.003). The ROC curve showed that the area under the curve is C = 0.718 with SE = 0.069 and 95% confidence interval from 0.548 to 0.852. The authors concluded that diffusion-weighted magnetic resonance imaging has limited diagnostic value in the assessment of viable tumour tissue after DEB-TACE in cases of HCC. Balli et al. [53] evaluated the effectiveness and safety of super-selective TACE with doxorubicin-loaded DEB sized 40–75 μm for HCC in early and intermediate stages according to BCLC staging system. Median follow-up was 22 months (range, 13–31), and 42 (93.3%) patients were followed up for more than 1 year. Overall complete response, partial response, and progressive disease rates were 53.3%, 33.3%, and 13.4% at 1 year and 22.2%, 26.7%, and 13.3% at 3 years, respectively. For target lesions, these rates were 60.0%, 26.7%, and 13.3% at 1 year and 28.9%, 6.7%, and 4.4% at 3 years, respectively. Median overall survival duration was 24 months (95% CI, 20.9–31.9 months). At 1 year and 3 years, overall survival rates were 71.0% and 44.4%, respectively. The only statistically significant relationship with overall survival was presence of chronic liver disease, which worsened the overall survival rate (p = 0.031). Time-to-progression was 23 months (95% CI, 15.1–40.0), and progression-free survival was 28 months (95% CI, 6.2–39.8). Postembolization syndrome occurred in ten patients (22.2%). Transient grade I/II bilirubin and aminotransferase elevation was observed in 26 (57.7%) and 18 (40%) patients, respectively. The authors stated that super-selective DEB-TACE with doxorubicin-loaded beads sized 40–75 μm is an effective and safe treatment method with prolonged time-to-progression and progression-free survival in early and intermediate stages of HCC. Presence of chronic liver disease is the only significant factor that worsened overall survival ratios after DEB-TACE. Balli et al. [55] compared the efficacy and safety of super-selective DEB-TACE with doxorubicin-loaded microspheres sized below and above 100 microns for treatment of HCC. Although statistically insignificant, median overall survival (19 months vs. 32 months, p = 0.190) and median progression-free survival (13 months vs. 20 months (p = 0.574) were longer, and 1–3-year objective response rates (7.40% vs. 23.33%, p = 0.330) were higher in above-100-microns group than in below-100-microns group, respectively. No mortality or major complications were observed. Grade I/II adverse events were detected in all patients. Transient elevations in liver function tests (grade III adverse events) were similar in both groups (3.57% vs. 3.33%; p = 0.980). The authors concluded that super-selective DEB-TACE with doxorubicin-loaded microspheres sized <100 microns is an effective and safe method for the HCC treatment. Objective response rates are higher and survival durations are longer after DEB-TACE is performed with doxorubicin-loaded microspheres sized below 100 microns. Farid et al. [90] measured serum vascular endothelial growth factor levels before and after cTACE versus DEB-TACE and evaluated its efficacy in predicting response to therapy and tumour recurrence. Vascular endothelial growth factor level was higher than baseline after cTACE (p < 0.001) and DEB-TACE (p = 0.004). It was also significantly higher in patients with progressive disease (p < 0.001). Vascular endothelial growth factor level at cutoff values of 97.3, 149.8, and 104.1 pg/mL could discriminate disease progression from treatment success with area under ROC curves of 0.806, 0.775, and 0.771, respectively. The sensitivity was 88.9%, 88.9%, and 77.8% and specificity was 62.5%, 64.6%, and 66.7%, respectively. However, no relation to tumour recurrence in complete response group could be detected after 1 year. The authors concluded that vascular endothelial growth factor serum levels may predict response to therapy in patients treated by DEB-TACE or cTACE, but it has no relation to tumour recurrence.
This brief literature review demonstrates that various technical, methodological, clinical, and prognostic aspects regarding TACE in HCC are under investigation in the Middle East countries.
References
Lewandowski RJ, Geschwind JF, Liapi E, Salem R. Transcatheter intraarterial therapies: rationale and overview. Radiology. 2011;259(3):641–57. https://doi.org/10.1148/radiol.11081489.
Ganeshan A, Upponi S, Hon LQ, Warakaulle D, Uberoi R. Hepatic arterial infusion of chemotherapy: the role of diagnostic and interventional radiology. Ann Oncol. 2008;19(5):847–51. https://doi.org/10.1093/annonc/mdm528.
Collins JM. Pharmacologic rationale for regional drug delivery. J Clin Oncol. 1984;2(5):498–504. https://doi.org/10.1200/jco.1984.2.5.498.
Melendez FDH. Pharmacologic principles of regional therapy in the traetment of liver metastases or primary liver tumors. In: Interventional oncology: principles and practice. Cambridge, England: Cambridge University Press; 2008.
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–14. https://doi.org/10.1016/s0140-6736(18)30010-2.
Bruix J SM. In: AASLD practice guideline: management of hepatocellular carcinoma: an update. 2020. https://www.aasld.org/publications/practice-guidelines. Accessed 01.10.2020.
Yamashita T. Current status of hepatocellular carcinoma treatment in Japan: hepatic arterial infusion chemotherapy. Clin Drug Investig. 2012;32 Suppl 2:15–23. https://doi.org/10.1007/bf03265493.
Gaba RC, Lokken RP, Hickey RM, Lipnik AJ, Lewandowski RJ, Salem R, et al. Quality improvement guidelines for transarterial chemoembolization and embolization of hepatic malignancy. J Vasc Interv Radiol. 2017;28(9):1210–23.e3. https://doi.org/10.1016/j.jvir.2017.04.025.
Vaidya S, Tozer KR, Chen J. An overview of embolic agents. Semin Intervent Radiol. 2008;25(3):204–15. https://doi.org/10.1055/s-0028-1085930.
Rand T, Loewe C, Schoder M, Schmook MT, Peck-Radosavljevic M, Kettenbach J, et al. Arterial embolization of unresectable hepatocellular carcinoma with use of microspheres, lipiodol, and cyanoacrylate. Cardiovasc Intervent Radiol. 2005;28(3):313–8. https://doi.org/10.1007/s00270-004-0153-y.
Wigmore SJ, Redhead DN, Thomson BN, Currie EJ, Parks RW, Madhavan KK, et al. Postchemoembolisation syndrome-tumour necrosis or hepatocyte injury? Br J Cancer. 2003;89(8):1423–7. https://doi.org/10.1038/sj.bjc.6601329.
Cornelis FH, Borgheresi A, Petre EN, Santos E, Solomon SB, Brown K. Hepatic arterial embolization using cone beam CT with tumor feeding vessel detection software: impact on hepatocellular carcinoma response. Cardiovasc Intervent Radiol. 2018;41(1):104–11. https://doi.org/10.1007/s00270-017-1758-2.
Llovet JM, Real MI, Montaña X, Planas R, Coll S, Aponte J, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359(9319):1734–9. https://doi.org/10.1016/S0140-6736(02)08649-X.
Tsochatzis EA, Fatourou E, O’Beirne J, Meyer T, Burroughs AK. Transarterial chemoembolization and bland embolization for hepatocellular carcinoma. World J Gastroenterol. 2014;20(12):3069–77. https://doi.org/10.3748/wjg.v20.i12.3069.
Lee EW, Khan S. Recent advances in transarterial embolotherapies in the treatment of hepatocellular carcinoma. Clin Mol Hepatol. 2017;23(4):265–72. https://doi.org/10.3350/cmh.2017.0111.
Kluger MD, Halazun KJ, Barroso RT, Fox AN, Olsen SK, Madoff DC, et al. Bland embolization versus chemoembolization of hepatocellular carcinoma before transplantation. Liver Transpl. 2014;20(5):536–43. https://doi.org/10.1002/lt.23846.
Malagari K, Pomoni M, Kelekis A, Pomoni A, Dourakis S, Spyridopoulos T, et al. Prospective randomized comparison of chemoembolization with doxorubicin-eluting beads and bland embolization with BeadBlock for hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2010;33(3):541–51. https://doi.org/10.1007/s00270-009-9750-0.
Brown DB, Gould JE, Gervais DA, Goldberg SN, Murthy R, Millward SF, et al. Transcatheter therapy for hepatic malignancy: standardization of terminology and reporting criteria. J Vasc Interv Radiol. 2007;18(12):1469–78. https://doi.org/10.1016/j.jvir.2007.08.027.
Pesapane F, Nezami N, Patella F, Geschwind JF. New concepts in embolotherapy of HCC. Med Oncol (Northwood, London, England). 2017;34(4):58. https://doi.org/10.1007/s12032-017-0917-2.
Kruskal JB, Hlatky L, Hahnfeldt P, Teramoto K, Stokes KR, Clouse ME. In vivo and in vitro analysis of the effectiveness of doxorubicin combined with temporary arterial occlusion in liver tumors. J Vasc Interv Radiol. 1993;4(6):741–7. https://doi.org/10.1016/s1051-0443(93)71965-x.
Lo CM, Ngan H, Tso WK, Liu CL, Lam CM, Poon RT, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology (Baltimore, Md). 2002;35(5):1164–71. https://doi.org/10.1053/jhep.2002.33156.
Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003;37(2):429–42. https://doi.org/10.1053/jhep.2003.50047.
Chan SL, Mo FK, Johnson PJ, Liem GS, Chan TC, Poon MC, et al. Prospective validation of the Chinese University Prognostic Index and comparison with other staging systems for hepatocellular carcinoma in an Asian population. J Gastroenterol Hepatol. 2011;26(2):340–7. https://doi.org/10.1111/j.1440-1746.2010.06329.x.
Yau T, Tang VY, Yao TJ, Fan ST, Lo CM, Poon RT. Development of Hong Kong Liver Cancer staging system with treatment stratification for patients with hepatocellular carcinoma. Gastroenterology. 2014;146(7):1691–700.e3. https://doi.org/10.1053/j.gastro.2014.02.032.
Kokudo N, Hasegawa K, Akahane M, Igaki H, Izumi N, Ichida T, et al. Evidence-based clinical practice guidelines for hepatocellular carcinoma: the Japan Society of Hepatology 2013 update (3rd JSH-HCC guidelines). Hepatol Res. 2015;45(2) https://doi.org/10.1111/hepr.12464.
Sieghart W, Hucke F, Peck-Radosavljevic M. Transarterial chemoembolization: modalities, indication, and patient selection. J Hepatol. 2015;62(5):1187–95. https://doi.org/10.1016/j.jhep.2015.02.010.
Raoul JL, Sangro B, Forner A, Mazzaferro V, Piscaglia F, Bolondi L, et al. Evolving strategies for the management of intermediate-stage hepatocellular carcinoma: available evidence and expert opinion on the use of transarterial chemoembolization. Cancer Treat Rev. 2011;37(3):212–20. https://doi.org/10.1016/j.ctrv.2010.07.006.
Forner A, Gilabert M, Bruix J, Raoul JL. Treatment of intermediate-stage hepatocellular carcinoma. Nat Rev Clin Oncol. 2014;11(9):525–35. https://doi.org/10.1038/nrclinonc.2014.122.
de Baere T, Arai Y, Lencioni R, Geschwind JF, Rilling W, Salem R, et al. Treatment of liver tumors with lipiodol tace: technical recommendations from experts opinion. Cardiovasc Intervent Radiol. 2016;39(3):334–43. https://doi.org/10.1007/s00270-015-1208-y.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Coldwell DM, Stokes KR, Yakes WF. Embolotherapy: agents, clinical applications, and techniques. Radiographics. 1994;14(3):623–43. https://doi.org/10.1148/radiographics.14.3.8066276.
Kan Z, Wright K, Wallace S. Ethiodized oil emulsions in hepatic microcirculation: in vivo microscopy in animal models. Acad Radiol. 1997;4(4):275–82. https://doi.org/10.1016/s1076-6332(97)80029-3.
Kan Z, Wallace S. Sinusoidal embolization: impact of iodized oil on hepatic microcirculation. J Vasc Interv Radiol. 1994;5(6):881–6. https://doi.org/10.1016/s1051-0443(94)71629-8.
EASL-EORTC Clinical Practice Guidelines: management of hepatocellular carcinoma. Eur J Cancer. 2012;48(5):599–641. https://doi.org/10.1016/j.ejca.2011.12.021.
Luo J, Guo RP, Lai EC, Zhang YJ, Lau WY, Chen MS, et al. Transarterial chemoembolization for unresectable hepatocellular carcinoma with portal vein tumor thrombosis: a prospective comparative study. Ann Surg Oncol. 2011;18(2):413–20. https://doi.org/10.1245/s10434-010-1321-8.
Verslype C, Rosmorduc O, Rougier P. Hepatocellular carcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23 Suppl 7:vii41–8. https://doi.org/10.1093/annonc/mds225.
Lencioni R, de Baere T, Soulen MC, Rilling WS, Geschwind JF. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: a systematic review of efficacy and safety data. Hepatology (Baltimore, Md). 2016;64(1):106–16. https://doi.org/10.1002/hep.28453.
Bouvier A, Ozenne V, Aubé C, Boursier J, Vullierme MP, Thouveny F, et al. Transarterial chemoembolisation: effect of selectivity on tolerance, tumour response and survival. Eur Radiol. 2011;21(8):1719–26. https://doi.org/10.1007/s00330-011-2118-2.
Kim DY, Ryu HJ, Choi JY, Park JY, Lee DY, Kim BK, et al. Radiological response predicts survival following transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma. Aliment Pharmacol Ther. 2012;35(11):1343–50. https://doi.org/10.1111/j.1365-2036.2012.05089.x.
Llovet JM, Lencioni R. mRECIST for HCC: performance and novel refinements. J Hepatol. 2020;72(2):288–306. https://doi.org/10.1016/j.jhep.2019.09.026.
Boily G, Villeneuve JP, Lacoursière L, Chaudhury P, Couture F, Ouellet JF, et al. Transarterial embolization therapies for the treatment of hepatocellular carcinoma: CEPO review and clinical recommendations. HPB (Oxford). 2015;17(1):52–65. https://doi.org/10.1111/hpb.12273.
Toro A, Pulvirenti E, Palermo F, Di Carlo I. Health-related quality of life in patients with hepatocellular carcinoma after hepatic resection, transcatheter arterial chemoembolization, radiofrequency ablation or no treatment. Surg Oncol. 2012;21(1):e23–30. https://doi.org/10.1016/j.suronc.2011.10.005.
Ikeda M, Arai Y, Park SJ, Takeuchi Y, Anai H, Kim JK, et al. Prospective study of transcatheter arterial chemoembolization for unresectable hepatocellular carcinoma: an Asian cooperative study between Japan and Korea. J Vasc Interv Radiol. 2013;24(4):490–500. https://doi.org/10.1016/j.jvir.2013.01.003.
Pomfret EA, Washburn K, Wald C, Nalesnik MA, Douglas D, Russo M, et al. Report of a national conference on liver allocation in patients with hepatocellular carcinoma in the United States. Liver Transpl. 2010;16(3):262–78. https://doi.org/10.1002/lt.21999.
Hong K, Khwaja A, Liapi E, Torbenson MS, Georgiades CS, Geschwind JF. New intra-arterial drug delivery system for the treatment of liver cancer: preclinical assessment in a rabbit model of liver cancer. Clin Cancer Res. 2006;12(8):2563–7. https://doi.org/10.1158/1078-0432.ccr-05-2225.
Grosso M, Vignali C, Quaretti P, Nicolini A, Melchiorre F, Gallarato G, et al. Transarterial chemoembolization for hepatocellular carcinoma with drug-eluting microspheres: preliminary results from an Italian multicentre study. Cardiovasc Intervent Radiol. 2008;31(6):1141–9. https://doi.org/10.1007/s00270-008-9409-2.
Malagari K, Alexopoulou E, Chatzimichail K, Hall B, Koskinas J, Ryan S, et al. Transcatheter chemoembolization in the treatment of HCC in patients not eligible for curative treatments: midterm results of doxorubicin-loaded DC bead. Abdom Imaging. 2008;33(5):512–9. https://doi.org/10.1007/s00261-007-9334-x.
Spreafico C, Cascella T, Facciorusso A, Sposito C, Rodolfo L, Morosi C, et al. Transarterial chemoembolization for hepatocellular carcinoma with a new generation of beads: clinical-radiological outcomes and safety profile. Cardiovasc Intervent Radiol. 2015;38(1):129–34. https://doi.org/10.1007/s00270-014-0907-0.
Malagari K, Pomoni M, Moschouris H, Kelekis A, Charokopakis A, Bouma E, et al. Chemoembolization of hepatocellular carcinoma with HepaSphere 30-60 μm. Safety and efficacy study. Cardiovasc Intervent Radiol. 2014;37(1):165–75. https://doi.org/10.1007/s00270-013-0777-x.
Malagari K, Kiakidis T, Pomoni M, Moschouris H, Emmanouil E, Spiridopoulos T, et al. Pharmacokinetics, safety, and efficacy of chemoembolization with doxorubicin-loaded tightly calibrated small microspheres in patients with hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2016;39(10):1379–91. https://doi.org/10.1007/s00270-016-1382-6.
Greco G, Cascella T, Facciorusso A, Nani R, Lanocita R, Morosi C, et al. Transarterial chemoembolization using 40 μm drug eluting beads for hepatocellular carcinoma. World J Radiol. 2017;9(5):245–52. https://doi.org/10.4329/wjr.v9.i5.245.
Richter G, Radeleff B, Stroszczynski C, Pereira P, Helmberger T, Barakat M, et al. Safety and feasibility of chemoembolization with doxorubicin-loaded small calibrated microspheres in patients with hepatocellular carcinoma: results of the MIRACLE I prospective multicenter study. Cardiovasc Intervent Radiol. 2018;41(4):587–93. https://doi.org/10.1007/s00270-017-1839-2.
Ballı HT, Aikimbaev K. Super-selective transarterial chemoembolization of hepatocellular carcinoma with doxorubicin-eluting beads sized 40-75 microns: assessment of efficacy and safety. Diagn Interv Radiol. 2020;26(5):482–7. https://doi.org/10.5152/dir.2020.19410.
Prajapati HJ, Xing M, Spivey JR, Hanish SI, El-Rayes BF, Kauh JS, et al. Survival, efficacy, and safety of small versus large doxorubicin drug-eluting beads TACE chemoembolization in patients with unresectable HCC. AJR Am J Roentgenol. 2014;203(6):W706–14. https://doi.org/10.2214/ajr.13.12308.
Balli H, Aksungur E, Khalatai B, Aikimbaev K. Super-selective transarterial chemoembolization with doxorubicin-loaded drug-eluting beads sized below and above 100 microns in hepatocellular carcinoma: a comparative study. J Belg Soc Radiol. 2019;103(1):47. https://doi.org/10.5334/jbsr.1841.
Varela M, Real MI, Burrel M, Forner A, Sala M, Brunet M, et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: efficacy and doxorubicin pharmacokinetics. J Hepatol. 2007;46(3):474–81. https://doi.org/10.1016/j.jhep.2006.10.020.
Dhanasekaran R, Kooby DA, Staley CA, Kauh JS, Khanna V, Kim HS. Comparison of conventional transarterial chemoembolization (TACE) and chemoembolization with doxorubicin drug eluting beads (DEB) for unresectable hepatocelluar carcinoma (HCC). J Surg Oncol. 2010;101(6):476–80. https://doi.org/10.1002/jso.21522.
Song MJ, Chun HJ, Song DS, Kim HY, Yoo SH, Park CH, et al. Comparative study between doxorubicin-eluting beads and conventional transarterial chemoembolization for treatment of hepatocellular carcinoma. J Hepatol. 2012;57(6):1244–50. https://doi.org/10.1016/j.jhep.2012.07.017.
Idilman I, Peynircioğlu B, Cil BE, Doğanay Erdoğan B, Yalçın S, Bayraktar Y, et al. Transarterial chemoembolization for treatment of hepatocellular carcinoma: a single center experience. Turk J Gastroenterol. 2013;24(2):141–7. https://doi.org/10.4318/tjg.2013.0709.
Facciorusso A, Mariani L, Sposito C, Spreafico C, Bongini M, Morosi C, et al. Drug-eluting beads versus conventional chemoembolization for the treatment of unresectable hepatocellular carcinoma. J Gastroenterol Hepatol. 2016;31(3):645–53. https://doi.org/10.1111/jgh.13147.
Golfieri R, Giampalma E, Renzulli M, Cioni R, Bargellini I, Bartolozzi C, et al. Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer. 2014;111(2):255–64. https://doi.org/10.1038/bjc.2014.199.
Karalli A, Teiler J, Haji M, Seth E, Brismar TB, Wahlin S, et al. Comparison of lipiodol infusion and drug-eluting beads transarterial chemoembolization of hepatocellular carcinoma in a real-life setting. Scand J Gastroenterol. 2019;54(7):905–12. https://doi.org/10.1080/00365521.2019.1632925.
Zhang ZS, Li HZ, Ma C, Xiao YD. Conventional versus drug-eluting beads chemoembolization for infiltrative hepatocellular carcinoma: a comparison of efficacy and safety. BMC Cancer. 2019;19(1):1162. https://doi.org/10.1186/s12885-019-6386-6.
Facciorusso A, Di Maso M, Muscatiello N. Drug-eluting beads versus conventional chemoembolization for the treatment of unresectable hepatocellular carcinoma: a meta-analysis. Dig Liver Dis. 2016;48(6):571–7. https://doi.org/10.1016/j.dld.2016.02.005.
Wang H, Cao C, Wei X, Shen K, Shu Y, Wan X, et al. A comparison between drug-eluting bead-transarterial chemoembolization and conventional transarterial chemoembolization in patients with hepatocellular carcinoma: a meta-analysis of six randomized controlled trials. J Cancer Res Ther. 2020;16(2):243–9. https://doi.org/10.4103/jcrt.JCRT_504_19.
Yang B, Liang J, Qu Z, Yang F, Liao Z, Gou H. Transarterial strategies for the treatment of unresectable hepatocellular carcinoma: a systematic review. PLoS One. 2020;15(2):e0227475. https://doi.org/10.1371/journal.pone.0227475.
Fernández M, Semela D, Bruix J, Colle I, Pinzani M, Bosch J. Angiogenesis in liver disease. J Hepatol. 2009;50(3):604–20. https://doi.org/10.1016/j.jhep.2008.12.011.
Geschwind JF, Kudo M, Marrero JA, Venook AP, Chen XP, Bronowicki JP, et al. TACE treatment in patients with sorafenib-treated unresectable hepatocellular carcinoma in clinical practice: final analysis of GIDEON. Radiology. 2016;279(2):630–40. https://doi.org/10.1148/radiol.2015150667.
Lencioni R, Llovet JM, Han G, Tak WY, Yang J, Guglielmi A, et al. Sorafenib or placebo plus TACE with doxorubicin-eluting beads for intermediate stage HCC: the SPACE trial. J Hepatol. 2016;64(5):1090–8. https://doi.org/10.1016/j.jhep.2016.01.012.
Gbolahan OB, Schacht MA, Beckley EW, LaRoche TP, O’Neil BH, Pyko M. Locoregional and systemic therapy for hepatocellular carcinoma. J Gastrointest Oncol. 2017;8(2):215–28. https://doi.org/10.21037/jgo.2017.03.13.
Meyer T, Fox R, Ma YT, Ross PJ, James MW, Sturgess R, et al. Sorafenib in combination with transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma (TACE 2): a randomised placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol Hepatol. 2017;2(8):565–75. https://doi.org/10.1016/S2468-1253(17)30156-5.
Park JW, Kim YJ, Kim DY, Bae SH, Paik SW, Lee YJ, et al. Sorafenib with or without concurrent transarterial chemoembolization in patients with advanced hepatocellular carcinoma: the phase III STAH trial. J Hepatol. 2019;70(4):684–91. https://doi.org/10.1016/j.jhep.2018.11.029.
Kudo M, Ueshima K, Ikeda M, Torimura T, Tanabe N, Aikata H, et al. Randomised, multicentre prospective trial of transarterial chemoembolisation (TACE) plus sorafenib as compared with TACE alone in patients with hepatocellular carcinoma: TACTICS trial. Gut. 2020;69(8):1492–501. https://doi.org/10.1136/gutjnl-2019-318934.
Wang G, Liu Y, Zhou SF, Qiu P, Xu L, Wen P, et al. Sorafenib combined with transarterial chemoembolization in patients with hepatocellular carcinoma: a meta-analysis and systematic review. Hepatol Int. 2016;10(3):501–10. https://doi.org/10.1007/s12072-015-9700-7.
Casadei Gardini A, Santini D, Aprile G, Silvestris N, Felli E, Foschi FG, et al. Antiangiogenic agents after first line and sorafenib plus chemoembolization: a systematic review. Oncotarget. 2017;8(39):66699–708. https://doi.org/10.18632/oncotarget.19449.
Pinter M, Ulbrich G, Sieghart W, Kölblinger C, Reiberger T, Li S, et al. Hepatocellular carcinoma: a phase II randomized controlled double-blind trial of transarterial chemoembolization in combination with biweekly intravenous administration of bevacizumab or a placebo1. Radiology. 2015;277(3):903–12. https://doi.org/10.1148/radiol.2015142140.
Smolka S, Chapiro J, Manzano W, Treilhard J, Reiner E, Deng Y, et al. The impact of antiangiogenic therapy combined with transarterial chemoembolization on enhancement based quantitative tumor response assessment in patients with hepatocellular carcinoma. Clin Imaging. 2017;46:1–7. https://doi.org/10.1016/j.clinimag.2017.05.007.
Palmer DH, Malagari K, Kulik LM. Role of locoregional therapies in the wake of systemic therapy. J Hepatol. 2020;72(2):277–87. https://doi.org/10.1016/j.jhep.2019.09.023.
Slovak R, Ludwig JM, Gettinger SN, Herbst RS, Kim HS. Immuno-thermal ablations-boosting the anticancer immune response. J Immunother Cancer. 2017;5(1):78. https://doi.org/10.1186/s40425-017-0284-8.
Marinelli B, Cedillo M, Pasik SD, Charles D, Murthy S, Patel RS, et al. Safety and efficacy of locoregional treatment during immunotherapy with nivolumab for hepatocellular carcinoma: a retrospective study of 41 interventions in 29 patients. J Vasc Interv Radiol. 2020; https://doi.org/10.1016/j.jvir.2020.07.009.
Zaky S, Makhlouf NA, Abdel Malek MO, Bakheet AA, Seif HM, Hamza HM, et al. Multidisciplinary decision making in the management of hepatocellular carcinoma: a hospital-based study. Turk J Gastroenterol. 2015;26(6):498–505. https://doi.org/10.5152/tjg.2015.0158.
El Sherbiny W, AbdelRahman A, Diasty M, Shaltout SW. Changes in Doppler parameters of portal pressure after interventional management of hepatocellular carcinoma. Abdom Radiol (New York). 2016;41(8):1532–8. https://doi.org/10.1007/s00261-016-0704-0.
Abdelmaksoud AH, Mandooh S, Nabeel MM, Elbaz TM, Shousha HI, Monier A, et al. Portal vein thrombosis in unresectable hcc cases: a single center study of prognostic factors and management in 140 patients. Asian Pac J Cancer Prev. 2017;18(1):183–8. https://doi.org/10.22034/apjcp.2017.18.1.183.
Abdelaziz AO, Abdelmaksoud AH, Nabeel MM, Shousha HI, Cordie AA, Mahmoud Sh H, et al. Transarterial chemoembolization combined with either radiofrequency or microwave ablation in management of hepatocellular carcinoma. Asian Pac J Cancer Prev. 2017;18(1):189–94. https://doi.org/10.22034/apjcp.2017.18.1.189.
Moustafa AS, Abdel Aal AK, Ertel N, Saad N, DuBay D, Saddekni S. Chemoembolization of hepatocellular carcinoma with extrahepatic collateral blood supply: anatomic and technical considerations. Radiographics. 2017;37(3):963–77. https://doi.org/10.1148/rg.2017160122.
Abdella H, Shaker MK, Montasser IF, Sobhi M, Aly H, Sayed A, et al. Outcome of transarterial chemoembolization in Egyptian patients with hepatocellular carcinoma and branch portal vein thrombosis. Indian J Gastroenterol. 2018;37(2):127–32. https://doi.org/10.1007/s12664-018-0830-4.
Hassan EA, Ahmed EH, Nafee AM, El-Gafary N, Hetta HF, El-Mokhtar MA. Regulatory T cells, IL10 and IL6 in HCV related hepatocellular carcinoma after transarterial chemoembolization (TACE). Egypt J Immunol. 2019;26(1):69–78.
Khalid MA, Achakzai IK, Hanif FM, Ahmed S, Majid Z, Luck NH. To determine the prognostic value of the albumin-bilirubin grade (ALBI) in patients underwent transarterial chemoembolization for unresectable hepatocellular carcinoma. Gastroenterol Hepatol Bed Bench. 2019;12(2):110–5.
Hassan AE, Mostafa RE, Nada A, Elazab MS, Awad AS, Hamed IM. Diagnostic accuracy of intermediate b-value diffusion-weighted imaging for detection of residual hepatocellular carcinoma following transarterial chemoembolization with drug-eluting beads. Indian J Radiol Imaging. 2019;29(2):195–200. https://doi.org/10.4103/ijri.IJRI_383_18.
Farid K, Elalfy H, Abo El-Khair SM, Elgamal H, Besheer T, Elmokadem A, et al. Prognostic value of vascular endothelial growth factor in both conventional and drug eluting beads transarterial chemoembolization for treatment of unresectable hepatocellular carcinoma in HCV patients. Expert Rev Gastroenterol Hepatol. 2020:1–12. https://doi.org/10.1080/17474124.2020.1823215.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Balli, H.T., Aikimbaev, K. (2021). Intra-arterial Chemotherapy and Transarterial Chemoembolization in Hepatocellular Carcinoma. In: Carr, B.I. (eds) Liver Cancer in the Middle East. Springer, Cham. https://doi.org/10.1007/978-3-030-78737-0_10
Download citation
DOI: https://doi.org/10.1007/978-3-030-78737-0_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-78736-3
Online ISBN: 978-3-030-78737-0
eBook Packages: MedicineMedicine (R0)