Abstract
Background
A mural nodule is a strong predictive factor for malignancy in branch duct intraductal papillary mucinous neoplasm (IPMN) of the pancreas, but the nodule size has hardly been considered. The aim of this study was to investigate whether a mural nodule of 10 mm was appropriate as an indicator of surgery for IPMN during follow-up.
Methods
The follow-up outcomes of 100 patients who had branch duct IPMN without mural nodules or who had branch duct IPMN with mural nodules of less than 9 mm in a tertiary care setting were investigated retrospectively. The patients underwent abdominal ultrasound (US) every 3 months and additional imaging examinations or cytologic examination of pancreatic juice when necessary. Surgery was recommended to them when a mural nodule developed or when a nodule enlarged and reached 10 mm.
Results
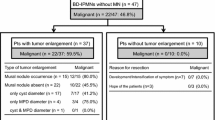
During an average follow-up period of 97 months, branch duct IPMNs developed mural nodules that reached 10 mm in 5 patients (0.62% per year). In one patient the IPMN was revealed to be non-invasive carcinoma by resection, 1 IPMN was shown to be malignant by further follow-up, and 3 were not resected because of refusal or the patient’s age. In 7 patients, mural nodules stayed within 9 mm. The remaining 88 patients lacked mural nodules in their branch duct IPMNs throughout the follow-up. The occurrence of invasive carcinoma around the IPMN was not indicated by imaging examinations in any patient. Univariate analysis showed that the size of the cyst at baseline significantly predicted the development of a mural nodule that reached 10 mm during follow-up (P = 0.05).
Conclusions
A mural nodule of 10 mm is appropriate as an indicator of surgery in the follow-up of branch duct IPMN.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas is being increasingly recognized, and is estimated to represent 1–3% of exocrine pancreatic neoplasms, 3–5% of all pancreatic neoplasms, and 20% of all cystic neoplasms of the pancreas [1, 2]. IPMN is a unique clinicopathological entity characterized by cystic dilatation of the pancreatic duct, mucus production, and papillary growth [1, 2]. IPMN is defined by histopathology as an intraductal mucin-producing neoplasm with tall columnar mucin-containing epithelium with or without papillary projections, and the neoplasm shows a wide spectrum of histological differentiation, from adenoma, dysplasia, and non-invasive carcinoma, to invasive carcinoma [1, 2]. The prognosis of IPMN is favorable compared with that of invasive ductal carcinoma if it is resected while noninvasive carcinoma is shown [3, 4].
IPMN is classified into 2 types according to site: main duct IPMN and branch duct IPMN, which are managed differently from each other. It has been recommended, by the consensus guidelines published recently, to resect all main duct IPMNs,because the average frequency of malignancy has been 70% and approximately two-thirds of them have been invasive. In contrast, on the grounds of lower frequencies of malignancy and invasive carcinoma, which have been 25 and 15%, respectively, surgery has been recommended only for branch duct IPMNs that had symptoms, cyst of more than 30 mm, mural nodule, or positive cytology [5]. However, recent studies showed that resection of branch duct IPMNs that had a cyst of more than 30 mm resulted in oversurgery in many cases [6–10]. Although a mural nodule is a predictor of malignancy in branch duct IPMN [6, 7, 11–16], nodule size has hardly been taken into consideration, with the exception of a few studies which found that branch duct IPMNs with mural nodules of more than 5 mm included not a few benign neoplasms [17–19]. In the present study, we followed up branch duct IPMNs without mural nodules and those with mural nodules of less than 9 mm until nodules developed or enlarged to a size of 10 mm, and we investigated whether the size of 10 mm was appropriate as an indicator of surgery for branch duct IPMN.
Patients and methods
The follow-up outcomes of 100 patients who had branch duct IPMN without mural nodules or with mural nodules less than 9 mm were investigated retrospectively.
Branch duct IPMNs were suggested by ultrasound (US), endoscopic ultrasound (EUS), or computed tomography (CT), and were confirmed by a dilated branch duct with a minimum size of 10 mm and mucus in it on endoscopic retrograde cholangiopancreatography (ERCP). The dilated branch duct corresponded to the cyst shown by imaging examinations in all patients. Branch duct IPMNs that had mural nodules of more than 10 mm or a positive result on cytologic examination of pancreatic juice collected during ERCP were excluded.
The study patients underwent US every 3 months for at least 36 months, and the sizes of the cyst, the main duct, and mural nodules were measured. The size of the mural nodule was expressed as its maximal diameter. When the cyst or the main duct was enlarged, or when mural nodules had developed or become enlarged on regular US, special imaging examinations such as EUS, CT, or magnetic resonance cholangiopancreatography (MRCP) were performed, and the sizes of the cyst, the main duct, and mural nodules were measured. Additional ERCP with cytologic examination of pancreatic juice was performed when the cyst or the main duct had enlarged significantly, or when mural nodules had developed or become enlarged. An increase in the size of the cyst by more than 50% and reaching 30 mm was defined as significant enlargement. Similarly, an increase in the size of the main duct by more than 50% and reaching 6 mm was defined as significant enlargement. Surgery was recommended to the patient when a mural nodule developed or had become enlarged and reached 10 mm, or when cytology indicated malignancy. A representative US image indicating a branch duct IPMN which developed a mural nodule of 10 mm is shown in Fig. 1.
This study protocol was approved by the institutional review board of Osaka Medical Center for Cancer and Cardiovascular Diseases. Informed consent was obtained from all the patients.
Statistical analysis was performed with SPSS software (SPSS, Chicago, IL, USA). Normally distributed continuous variables were compared by Student’s t-test, non-normally distributed variables by the Mann–Whitney U-test, and categorical variables by the Chi-square test or Fisher’s exact test. Hazard ratios of potential predictive variables were calculated with a univariate or multivariate Cox proportional hazard model, which was used for modeling time-to-event data in the presence of censored cases. A P value of <0.05 was considered to be statistically significant.
Results
Clinical characteristics of 100 patients with branch duct IPMN, and morphological features of their IPMNs
The clinical characteristics of 100 patients with branch duct IPMN and morphological features of their IPMNs at baseline are summarized in Table 1. The mean age of the patients was 65 years (range 40–80 years), and there was no significant preponderance in the gender of the patients. A small minority of patients were symptomatic or diabetic, and had a high carcinoembryonic antigen (CEA) or carbohydrate antigen (CA) 19-9 level. There was no significant preponderance in the anatomical location of the branch duct IPMNs. Approximately two-thirds of the branch duct IPMNs were multiple. The mean sizes of the cyst and the main duct were 21 mm (range 10–60 mm) and 3.8 mm (range 1–8 mm), respectively. Only 5 patients had mural nodules, with the mean size being 4.4 mm (range 3–5 mm). The median follow-up period was 97 months (range 37–257 months).
Morphological changes of branch duct IPMNs and results of cytology during follow-up
The cyst and the main duct were significantly enlarged in 28 (28%) and 11 (11%) patients, respectively. Five (5%) patients developed mural nodules that reached 10 mm during follow-up, and 2 (2%) patients developed mural nodules that did not reach 10 mm. The mural nodules that were present at baseline in 5 (5%) patients did not become enlarged during follow-up. The remaining 88 (88%) patients lacked mural nodules throughout the follow-up. The occurrence of invasive carcinoma around the IPMN was not indicated by imaging examinations in any patient. The rate of development of a mural nodule that reached 10 mm in branch duct IPMN during follow-up was 0.62% per year. Cytologic examination of pancreatic juice did not indicate malignancy in any patient in whom a mural nodule did not develop to reach 10 mm.
Comparison of clinical characteristics of patients and morphological features of their IPMNs at baseline between those which developed mural nodules that reached 10 mm and those which did not
High CEA and CA19-9 levels at baseline were less frequent in patients who developed mural nodules that reached 10 mm, although the differences were not significant. Branch duct IPMNs in the pancreatic head, solitary IPMNs, and IPMNs with a larger cyst developed mural nodules that reached 10 mm more frequently, although the difference did not reach statistical significance (Table 2).
Branch duct IPMNs which developed mural nodules that reached 10 mm during follow-up
The clinical characteristics of the 5 patients who developed mural nodules that reached 10 mm in branch duct IPMNs during follow-up, and their morphological features, are summarized in Table 3. The cyst and the main duct were enlarged significantly in 4 and 2 patients, respectively. Mural nodules that developed and reached 10 mm were detected by US in 3, EUS in 1, and MRCP in 1, and were also shown by other imaging examinations that were performed subsequently. In 1 patient (no. 1), a mural nodule reached 10 mm at 37 months without significant enlargement in the cyst or the main duct on EUS (Fig. 2). The IPMN was successfully resected, and was revealed to be a non-invasive intraductal papillary mucinous carcinoma (Fig. 3). In 3 patients (nos. 2–4), mural nodules developed that reached 10 mm at 105, 132, and 182 months, without a suggestion of the occurrence of invasive carcinoma around the IPMNs on imaging examinations. However, surgery recommended to these patients was not performed because of their age or refusal. They were followed up for a further 4, 15, and 31 months without any suggestion of the occurrence of invasive carcinoma around the IPMNs on imaging examinations. In the remaining 1 patient (no. 5), a mural nodule developed that reached 10 mm at 88 months without any suggestion of the occurrence of invasive carcinoma around the IPMN, but she refused cytologic examination or surgery recommended to her. EUS indicated cancer invasion beyond the IPMN 7 months later (Fig. 4), and she died of cancer a further 10 months later. Consequently, 2 IPMNs that developed mural nodules that reached 10 mm during follow-up were confirmed to be malignant.
Predictive factors at baseline for the development of mural nodules that reached 10 mm in branch duct IPMN
Univariate and multivariate analyses of potential predictive factors at baseline for the development of mural nodules that reached 10 mm, by Cox proportional hazard model, are summarized in Table 4. Univariate analysis showed that the size of the cyst at baseline was a predictive factor that was statistically significant (hazard ratio 2.4, 95% confidence interval 1.0–5.7, P value 0.05), although multivariate analysis failed to find statistical significance (P value 0.07). The location of the pancreatic head and solitary cyst at baseline predicted the development of a mural nodule that reached 10 mm, although not significantly. Other factors were not shown to predict the development of a mural nodule that reached 10 mm during follow-up. Analysis showed that the presence of symptoms, diabetes, a high level of CEA or CA19-9, and the presence of a mural nodule at baseline were not significant predictors of the development of a mural nodule that reached 10 mm.
Development of ductal carcinoma distinct from IPMN during follow-up
Ductal carcinoma of the pancreas, distinct from branch duct IPMN, developed in 2 patients during follow-up. Both of the cancers were detected at a resectable stage; one was successfully resected and the other was not submitted to surgery because of the age of the patient.
Discussion
In the management of branch duct IPMNs of the pancreas, surgery has been recommended to those with mural nodules irrespective of their size, because a mural nodule has been considered a strong predictor of malignancy [6, 7, 11–16]. However, the nodule’s size has to be considered, because larger nodules are likely to be malignant and smaller ones are likely to be benign [20, 21]. Recent studies showed that branch duct IPMNs with mural nodules of more than 5 mm included not a few benign neoplasms [17–19]. Therefore, in the present study, branch duct IPMNs without mural nodules or with mural nodules of less than 9 mm were followed up until nodules developed or became enlarged and reached 10 mm, when surgical resection was recommended to the patient. Branch duct IPMNs that could be followed up were selected, and also cytologic examination of pancreatic juice was performed for all the IPMNs during ERCP in order to exclude malignant neoplasms. Cytology is useful for discriminating benign from malignant branch duct IPMNs, although this modality is not as useful as it is for discriminating benign from malignant main duct IPMNs ([22] and our unpublished data).
In the present study, mural nodules developed or enlarged reaching10 mm in only 5 (5%) branch duct IPMNs during an average period of 97 months (0.62% per year). One IPMN was successfully resected and subsequent histological examination of the resected specimen disclosed a non-invasive carcinoma; 4 were not resected because of the patients’ age or refusal. Further follow-up examinations for 3 of these 4 did not indicate any development of invasive carcinoma around the IPMNs, suggesting they were still intraductal neoplasms. In 7 branch duct IPMNs whose mural nodules stayed within 9 mm, and the remaining 88 IPMNs which lacked mural nodules throughout the follow-up, the development of invasive carcinoma was not indicated around the IPMNs by imaging examinations. Without surgery, it could not be known whether or not they developed malignancy, but they were likely to remain benign neoplasms, considering that they grew slowly or were barely enlarged. These results showed that a 10 mm mural nodule was quite appropriate as an indicator of surgery for branch duct IPMNs during follow-up. Regrettably, in 1 patient who developed a mural nodule that reached 10 mm and refused surgery, EUS indicated an invasive carcinoma adjacent to the mural nodule 7 months after the identification of the nodule. It is possible that the IPMN could have been successfully resected while it was non-invasive carcinoma, but the patient refused surgery when the mural nodule had just reached 10 mm. However, we were not able to confirm that it was non-invasive carcinoma because surgery was not performed. Surgery should be strongly recommended for branch duct IPMNs that developmural nodules that reach 10 mm.
In the present study, univariate analysis by the Cox proportional hazard model showed that the size of the cyst was a significant predictive factor for the development of a mural nodule that reached 10 mm, although multivariate analysis failed to show statistical significance, with a P value of 0.07. In following up branch duct IPMNs with larger cysts, physicians should pay special attention to the development of mural nodules in the IPMNs. This does not always indicate that branch duct IPMNs with larger cysts should immediately be resected. Although a cyst of more than 30 mm has been reported to be a predictor of malignancy in branch duct IPMN [11, 18] and consensus guidelines published recently have recommended surgery for IPMNs in which the cyst was more than 30 mm [5], more recent studies have shown that resection of these branch duct IPMNs resulted in oversurgery in many cases [6–10]. In the present study, 28 (28%) branch duct IPMNs that progressed to exceed 30 mm in cyst size were not resected unless their mural nodules reached 10 mm; these patients were followed up without occurrence of invasive carcinoma around the IPMNs on imaging or positive cytology. Without surgery, we did not know whether or not they developed malignancy during follow-up, but the absence of invasive carcinoma around the IPMNs on imaging and the negative cytology indicated that the neoplasms were likely to remain benign. However, branch duct IPMNs that continue to enlarge in cyst size may need resection even if they lack mural nodules, positive cytology, or the occurrence of invasive carcinoma around the IPMNs on imaging, and even if they actually are not malignant neoplasms.
We had assumed that branch duct IPMN with a mural nodule at baseline might be at high risk for progression, because the presence of a mural nodule has been a strong predictor of malignancy [6, 7, 11–16]. However, in the present study, analysis failed to show the presence of a mural nodule at baseline as a predictive factor for the development of a mural nodule that reached 10 mm. The mural nodules in the 5 IPMNs that had already been present at baseline were barely enlarged during follow-up, and all of the 5 IPMNs that developed mural nodules that reached 10 mm during follow-up had lacked them at baseline.
Having our attention caught only by mural nodules, we may miss detecting the development of malignancy in branch duct IPMN without a mural nodule. To prevent such an oversight, in the present study, cytologic examination of pancreatic juice at ERCP was performed when the cyst or the main duct had become significantly enlarged during follow-up. We previously reported, for the first time, that cytology could differentiate benign from malignant IPMNs of the pancreas, when IPMNs had been called “mucin-producing tumors” [23]. Cytologic examination is useful for the discrimination of branch duct IPMNs, as mentioned before, although this examination’s sensitivity for malignancy was inferior to that for main duct IPMNs ([22] and our unpublished data). However, in the present study, cytology during follow-up did not indicate malignancy in any IPMN in which a mural nodule did not develop to a size of 10 mm.
We found that two (2%) ductal carcinomas occurred, distinct from branch duct IPMNs, during the follow-up. We found it difficult to believe they had already been present when the follow-up started, because they had not been indicated by high-resolution imaging or by cytologic examination of pancreatic juice. Further, the ductal carcinomas were detected at 45 and 112 months of follow-up. It is not possible that they had already been present for so long before detection, considering that ductal carcinoma of the pancreas is a rapidly progressing tumor. There have been a few reports on the synchronous or metachronous occurrence of ductal carcinoma and IPMN of the pancreas [24, 25]. Recently, we also reported the development of ductal carcinoma during the follow-up of branch duct IPMN [26]. In these branch duct IPMNs, the cysts were smaller in size, ranging from 10 to 30 mm [24, 26]. However, surgery for all IPMNs with smaller cysts would not be justified, because ductal carcinoma occurred in only 8–9% of branch duct IPMNs [25, 26]. This is a different issue from the selection of candidates for surgery in branch duct IPMN, which is argued in the present study, although a matter of importance considering the poor prognosis of ductal carcinoma compared with that of IPMN. Special attention should be paid to the occurrence of ductal carcinoma of the pancreas during the follow-up of branch duct IPMN.
In conclusion, it was shown that mural nodule size was appropriate as an indicator of surgery in the follow-up of branch duct IPMN. Surgery should be recommended for branch duct IPMNs that develop mural nodules that exceed 10 mm during follow-up, while IPMNs may be managed conservatively as long as their mural nodules do not reach 10 mm.
Abbreviations
- IPMN:
-
Intraductal papillary mucinous neoplasm
- US:
-
Ultrasound
- EUS:
-
Endoscopic ultrasound
- CT:
-
Computed tomography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- MRCP:
-
Magnetic resonance cholangiopancreatography
References
Longnecker DS, Adler G, Hruban RH, et al. Intraductal papillary mucinous neoplasms of the pancreas. In: Hamilton SR, Aaltonen LA, editors. World Health Organization classification of tumors. Pathology and genetics of tumours of the digestive system. Lyon: IARC Press; 2000. p. 237–40.
Hruban RH, Pitman MB, Klimstra DS. Intraductal papillary mucinous neoplasm. In: AFIP Atlas of tumor pathology. Tumors of the pancreas. Washington: ARP Press; 2007. p. 75–100.
D’Angelica M, Brennan MF, Suriawinata AA, et al. Intraductal papillary mucinous neoplasms of the pancreas: an analysis of clinicopathologic features and outcome. Ann Surg. 2004;239:400–8.
Sohn TA, Yeo CJ, Cameron JL, et al. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–99.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006;6:17–32.
Rodriguez JR, Salvia R, Crippa S, et al. Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology. 2007;133:72–9.
Salvia R, Crippa S, Falconi M, et al. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut. 2007;56:1086–90.
Pelaez-Luna M, Chari ST, Smyrk TC, et al. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am J Gastroenterol. 2007;102:1759–64.
Tang RS, Weinberg B, Dawson DW, et al. Evaluation of the guidelines for management of pancreatic branch-duct intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol. 2008;6:815–9.
Woo SM, Ryu JK, Lee SH, et al. Branch duct intraductal papillary mucinous neoplasms in a retrospective series of 190 patients. Br J Surg. 2009;96:405–11.
Sugiyama M, Izumisato Y, Abe N, et al. Predictive factors for malignancy in intraductal papillary-mucinous tumors of the pancreas. Br J Surg. 2003;90:1244–9.
Serikawa M, Sasaki T, Fujimoto Y, et al. Management of intraductal papillary-mucinous neoplasm of the pancreas: treatment strategy based on morphologic classification. J Clin Gastroenterol. 2006;40:856–62.
Fujino Y, Matsumoto I, Ueda T, et al. Proposed new score predicting malignancy of intraductal papillary mucinous neoplasms of the pancreas. Am J Surg. 2007;194:304–7.
Schmidt CM, White PB, Waters JA, et al. Intraductal papillary mucinous neoplasms. Predictors of malignant and invasive pathology. Ann Surg. 2007;246:644–54.
Rautou PE, Levy P, Vullierme MP, et al. Morphologic changes in branch duct intraductal papillary mucinous neoplasms of the pancreas: a midterm follow-up study. Clin Gastroenterol Hepatol. 2008;6:807–14.
Nara S, Onaya H, Hiraoka N, et al. Predictive evaluation of invasive and noninvasive intraductal papillary-mucinous neoplasms of the pancreas: clinical, radiological, and pathological analysis of 123 cases. Pancreas. 2009;38:8–16.
Kobayashi G, Fujita N, Noda Y, et al. Mode of progression of intraductal papillary-mucinous tumor of the pancreas: analysis of patients with follow-up by EUS. J Gastroenterol. 2005;40:744–51.
Okabayashi T, Kobayashi M, Nishimori I, et al. Clinicopathological features and medical management of intraductal papillary mucinous neoplasms. J Gastroenterol Hepatol. 2006;21:462–7.
Hirono S, Tani M, Kawai M, et al. Treatment strategy for intraductal papillary mucinous neoplasm of the pancreas based on malignant predictive factors. Arch Surg. 2009;144:345–9.
Kubo H, Chijiiwa Y, Akahoshi K, et al. Intraductal papillary-mucinous tumors of the pancreas: differential diagnosis between benign and malignant tumors by endoscopic ultrasonography. Am J Gastroenterol. 2001;96:1429–34.
Choi BS, Kim TK, Kim AY, et al. Differential diagnosis of benign and malignant intraductal papillary mucinous tumors of the pancreas: MR cholangiopancreatography and MR angiography. Korean J Radiol. 2003;4:157–62.
Yamaguchi T, Shira Y, Ishihara T, et al. Pancreatic juice cytology in the diagnosis of intraductal papillary mucinous neoplasm of the pancreas. Cancer. 2005;104:2830–6.
Uehara H, Nakaizumi A, Iishi H, et al. Cytologic examination of pancreatic juice for differential diagnosis of benign and malignant mucin-producing tumors of the pancreas. Cancer. 1994;74:826–33.
Tada M, Kawabe T, Arizumi M, et al. Pancreatic cancer in patients with pancreatic cystic lesions: a prospective study in 197 patients. Clin Gastroenterol Hepatol. 2006;4:1265–70.
Ingkakul T, Sadakari Y, Ienaga J, et al. Predictors of the presence of concomitant invasive ductal carcinoma in intraductal papillary mucinous neoplasm of the pancreas. Ann Surg. 2010;251:70–5.
Uehara H, Nakaizumi A, Ishikawa O, et al. Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut. 2008;57:1561–5.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uehara, H., Ishikawa, O., Katayama, K. et al. Size of mural nodule as an indicator of surgery for branch duct intraductal papillary mucinous neoplasm of the pancreas during follow-up. J Gastroenterol 46, 657–663 (2011). https://doi.org/10.1007/s00535-010-0343-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0343-0