Abstract
Background
The international consensus guidelines for the management of intraductal papillary mucinous neoplasm (IPMN) of the pancreas were revised in 2012 Tanaka (Pancreatology 12(3):183–197, 2012), making the indications for operation less aggressive. Therefore, the number of branch duct-type IPMN (BD-IPMN) patients requiring follow-up care is expected to increase in the future.
Methods
The aim of this study was to identify risk factors for malignancy in BD-IPMN patients during the follow-up period. This study included 47 BD-IPMN patients without a mural nodule (MN) at the time of initial diagnosis and who subsequently underwent resection after a follow-up period of more than 3 months. Data for the patients were reviewed retrospectively, and the clinicopathological factors were investigated.
Results
In a univariate analysis, age (≧65 years), an increase in the main pancreatic duct (MPD) diameter, the MPD diameter at resection (≧5 mm), and the occurrence of MN were significantly associated with malignancy. The occurrence of MN was the only significant factor in a multivariate analysis. In addition, 7 of the 17 patients (41.2 %) who only exhibited an increase in the cyst diameter during the follow-up period were diagnosed as having malignancies. All 6 patients who exhibited an increase in the cyst diameter of 100 % or more were diagnosed as having carcinoma.
Conclusions
During the follow-up period, the incidence of malignancy was higher among patients with BD-IPMNs and the occurrence of MN, an increase in the MPD diameter, or an increase ratio of 100 % or more in cyst diameter than the others; resection was recommended for these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The first case of intraductal papillary mucinous neoplasm (IPMN) was reported in the 1980s [2]. An increasing number of cases have since been reported all over the world. Branch duct IPMN (BD-IPMN) is the most common variant of this disease, has the lowest risk of malignancy, and is most often diagnosed incidentally [3]. The management of IPMN has been constantly evolving. In 2006, international consensus guidelines for the management of IPMN were proposed by a Working group of the International Association of Pancreatology (IAP) following the Congress of the IAP in Sendai, Japan [4]. The international consensus guidelines for the management of IPMN of the pancreas were subsequently revised in 2012 [1]. Only 3 high-risk stigmata of malignancy were considered to indicate a need for resection: (1) obstructive jaundice in a patient with a cystic lesion on the head of the pancreas, (2) an enhanced solid component within the cyst, and (3) a main pancreatic duct (MPD) >10 mm in size. In the 2006 guidelines, patients with a cyst diameter of more than 30 mm were recommended to undergo immediate resection; however, in the 2012 guidelines, those cases were excluded from the surgical indications. Therefore, the number of BD-IPMN patients requiring follow-up care is expected to increase in the future. However, few studies have discussed findings for the association of malignancy during follow-up periods, so it was unclear whether only patients with “high-risk stigmata” findings according to the 2012 IPMN guidelines should undergo resection [1]. The objective of this study was to identify risk factors for malignancy in BD-IPMNs during the follow-up period.
Patients & methods
Criteria for inclusion in the present study
From January 1994 to December 2012, 104 patients underwent resectional surgery for BD-IPMN according to the following criteria: the presence of MN, MPD diameter 6 mm or more, cyst diameter 30 mm or more, and severe symptom. Among these patients, the present retrospective study group consisted of patients with a follow-up duration of three months or more prior to undergoing surgery. The other inclusion criteria were as follows: (1) an initial diagnosis of BD-IPMN, excluding patients with a diagnosis of main duct IPMN or mixed-type IPMN; (2) patients without a mural nodule (MN) at the initial diagnosis; (3) patients who underwent strict follow-up examinations every 3–6 months; and (4) the availability of detailed imaging findings obtained during the follow-up period, if the patients had been referred from another hospital. Forty-seven patients were eligible for inclusion in the present study.
The greatest dimension of the evaluated lesion was measured at the initial visit and during the follow-up period. We evaluated the lesion at the same site using the same modality, if possible. The reasons for an operation after follow-up were the enlargement of the tumor (n = 37), the development/intensification of symptom (n = 7), or the wishes of the patients (n = 3) (Fig. 1). The definition of tumor enlargement was a 3 mm or more increase in cyst diameter, a 2 mm or more increase in the MPD diameter, or the occurrence of an MN. In consideration of measurement deviations, we defined an increase in the cyst diameter not exceeding 3 mm or an increase in the MPD diameter not exceeding 2 mm as “No change.” The clinicopathological factors of the 47 patients were analyzed retrospectively. The median follow-up period was 36 months (3–240 months). There were 30 men and 17 women, ranging in age from 47 to 77 years (mean, 66.2 years).
Histological classification
The pathologic findings were described according to the WHO Classification of Tumors of the Digestive System, Fourth Edition [5]. IPMNs are classified into two broad groups—those that are associated with an invasive cancer (IPMC) and those that are not associated with an invasive cancer. IPMNs without an associated invasive cancer can be further subcategorized into three groups: IPMN with low-grade dysplasia (LGD), IPMN with moderate-grade dysplasia (MGD), and IPMN with high-grade dysplasia (HGD). We diagnosed carcinoma in situ (CIS) with HGD as outlined in the recent WHO classification [5]. Whether CIS has a malignant potential is controversial. Based on the conventional opinion in Japan, we considered HGD and IPMC as malignancies in the present study. The staging/definition of the lymph node status was principally based on the UICC TNM classification of malignant tumors (7th edition, 2009) [6].
Statistical analysis
A P value of less than 0.05 was considered to indicate statistical significance. The comparison of continuous data for tumor size was analyzed using the Mann–Whitney U test. Risk factors for malignancy in the BD-IPMNs after the follow-up periods were analyzed using a χ 2 test. Only variables that were selected as being statistically significant using a univariate analysis (P < 0.05) were included in the multivariate analysis with logistic regression analysis. The statistical analysis was performed using the SPSS version 19.0 software (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics and clinicopathological features
The patient characteristics and clinicopathological features are shown in Table 1. The mean follow-up period was 36.3 months. The mean maximal cyst diameter at the time of surgical resection was 35.2 mm. Compared with the diameter at the initial diagnosis, the mean increase in the cyst diameter was 8.2 mm. The mean maximal MPD diameter was 6.7 mm. The mean increase in the MPD diameter was 2.3 mm. The average interval of time until an increase in the MPD (a diameter increase >2 mm) was 34.6 months. MN developed in 15 patients (31.9 %). The average interval of time until the occurrence of an MN was 34.1 months. Histopathologically, the tumors were classified as LGD-MGD in 25 patients (53.2 %), HGD in 10 patients (21.3 %), and IPMC in 12 patients (25.5 %). Malignant lesions (HGD, IPMC) accounted for about half of the lesions in all the patients (46.8 %).
Changes in cystic diameter, MPD diameter, and occurrence of MN in benign/malignant cases
There were no significant differences between the benign and malignant subgroups with regard to the cyst and MPD diameter at the initial diagnosis (Table 2). The mean cyst diameters at resection were 33.4 and 38.0 mm for the benign and malignant IPMNs, respectively, whereas the mean increases in the cyst diameter were 6.0 and 10.6 mm, respectively. The malignant IPMNs tended to be larger than the benign lesions, but no significant difference in the cyst diameters was observed. The mean MPD diameter at resection were 5.5 and 8.3 mm for the benign and malignant IPMNs, respectively, while the mean increases in the MPD diameter were 1.4 and 3.2 mm, respectively; the difference in the MPD diameter at resection was significant (P = 0.015), as was the increase in the cyst diameter during the follow-up period (P = 0.016). Among the patients with benign IPMNs, three patients developed an MN during the follow-up period (12.0 %, 3/25). On the other hand, MNs developed in several of the patients with malignant IPMNs (54.5 %, 12/22), resulting in a significant difference between the groups (P = 0.004).
Analysis of risk factors for malignancy
Age (>65 years), MPD diameter at resection (≧5 mm), an increase in the MPD, and the occurrence of MN were identified as significant factors of the presence of malignancy using univariate analyses (Table 3). In a multivariate analysis, only the occurrence of MN was identified as a significant factor (P = 0.005, HR8.400). No significant differences according to cystic diameter were observed.
Incidence of resected malignancy BD-IPMNs with and without enlargement
Figure 1 shows the incidence of malignancy among the 47 patients who underwent resection after follow-up. Of the 47 BD-IPMNs, 25 (53.2 %) were histologically diagnosed as benign (LGD or MGD) and 22 (46.8 %) were diagnosed as malignant (HGD in 10 and invasive IPMC in 12). The incidence of malignancy among patients without enlargement was 0 % (0/10). On the other hand, the incidence of malignancy in patients with enlargement was 59.5 % (22/37). The patients with MN had a high probability (80 %; 12/15) of malignancy. Among the patients without MN, only the patients with an increase in the MPD diameter had a high probability (75 %; 3/4) of malignancy.
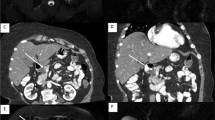
Among patients with an increase in the cyst diameter only, scatter diagrams of the malignant lesions depended on cyst diameter at the time of operation, increase in size, speed of increase, and increased ratio
The incidence of malignancy among patients with only an increase in the cyst diameter and without the occurrence of MN, and an increase in the MPD diameter was not very high (41.2 %; 7/17), so the surgical indications for such patients were thought to be a significant clinical problem. Therefore, we examined these patients (n = 17) separately. Only one patient had invasive IPMC, and the other six patients had HGD. Figure 2a–d shows a scatter diagram of malignant lesions according to cyst diameter at the time of operation, the increase in the cyst diameter, the speed of the increase in the cyst diameter (increase speed), and the increase in the ratio of the cyst diameter (increase ratio). We defined the “increase speed” as the increase in the cyst diameter (mm) divided by the follow-up period (in months), whereas the “increase ratio” was defined as the increase in the cyst diameter divided by the cyst diameter at the time of the initial diagnosis. The malignant potential was not correlated with the cyst diameter at the time of operation (Fig. 2a). However, the malignant potential seemed to be correlated with the increase ratio of the cyst diameter as well (Fig. 2d). All the patients with an increase in the ratio of the cyst diameter of 100 % or more had malignant lesions. The average interval of time for the development of a cyst size of more than 100 % was 55.1 months. Six of the 7 (85.7 %) malignant lesions had an increase ratio of the cyst diameter of more than 100 %. All ten benign lesions had values of less than 100 % for this parameter.
Scatter diagrams of the malignant lesions according to increase size, increase speed, and increase ratio in patients with an enlargement of the cyst diameter only. Increase speed in cyst diameter* = increase in cyst diameter/follow-up periods (mm/month), increase ratio of cyst diameter** = increase in cyst diameter/cyst diameter at the initial diagnosis X 100 (%).LGD-MGD, low/moderate-grade dysplasia (n = 10); HGD, high-grade dysplasia (n = 6); Invasive Ca, invasive carcinoma (n = 1)
Discussion
Several reports have discussed the follow-up of BD-IPMN patients [7–9]; however, few patients requiring resection after follow-up have been mentioned. We have experienced a relatively large number of BD-IPMN patients requiring resection after follow-up, so we examined the risk factors for malignancy among these patients. Because the main focus of this study was to identify risk factors for malignancy, we excluded patients with follow-up but without resection from this study.
In several follow-up studies of BD-IPMNs [8, 10, 11], the incidence of malignancy among patients without tumor enlargement was 0 % or very low. Similarly, the present study showed that all 10 patients without tumor enlargement had benign lesions (Fig. 1). For these patients, the surgical indications should be carefully evaluated in consideration of a balance between symptom and surgical stress.
Although the probability that a MN will occur during the follow-up period is very low [8, 11], the presence of MNs has been reported to be strongly suggestive of malignancy in patients with BD-IPMNs. The incidence of malignancy among BD-IPMN patients with MN is reportedly very high, ranging from 63.0 % to 82.6 % [12–14], and it was 80.0 % in the present series, consistent with previously reported values. In addition, in the present study, a multivariate analysis for risk factors of malignancy showed that MN was the only independent risk factor. Therefore, immediate surgical resection is recommended for such patients.
Several authors have reported that malignancy is associated with an increased MPD diameter during the follow-up period [8–10]. In our study, similarly, an increase in the MPD diameter and the MPD diameter at resection were larger for malignant BD-IPMNs than for benign BD-IPMNs. However, only 10 patients exhibited an increase in the MPD diameter during the follow-up period, so we could not report definitive data. Nevertheless, among the patients without the occurrence of an MN, three of the 5 BD-IPMN patients with an increase in the MPD diameter exhibited malignant lesions, and such patients should thus undergo resection.
In this study, there was a significant difference in age between patients with and without malignant lesions in a univariate analysis (P = 0.010); BD-IPMN developed into a malignancy more often in patients over 65 years of age. Although the reason for the difference is unclear, age-related tumor immunity may play an important role in the development and pathogenesis of BD-IPMN. Many reports have discussed age-related tumor immunity and its ability to militate against tumor progression [15–18].
The international consensus guidelines for the management of intraductal papillary mucinous neoplasm (IPMN) of the pancreas were revised in 2012 [1], and cystic diameter was excluded from the surgical indications. Therefore, in this study, we also analyzed the risk of malignancy among patients without MN occurrence and without an increase in the MPD diameter during the follow-up period, since we thought that such patients were likely to increase in number and to present problems with regard to surgical indications in the future. In our study, the cyst diameter at the time of operation was poorly correlated with malignancy (Table 2) and the incidence of malignant IPMN for cyst sizes of <4 and ≥4 cm were 37.5 and 44.4 %, respectively (data not shown). These data suggest that some small cysts have malignant potential, and that predicting malignancy based on cyst size is inadvisable. Furthermore, several authors have reported that an increase in cyst diameter associates malignancy [9, 10], but recent reports [19, 20] have suggested that an increase in cyst size alone is not a reliable factor of malignancy in the absence of other indications.
Our data showed that the “increase speed” in the cyst diameter was poorly correlated with malignancy (Fig. 2). Several studies [7, 21] have shown a correlation between the increase speed in the cyst diameter and malignancy. However, in clinical practice, we experienced several patients with IPMN that exhibited a rapid enlargement in the cyst diameter after a long follow-up period without tumor progression. The tumors in these cases likely acquired the ability to undergo mucus hyper-production through a biological change at some point in time. Thus, the speed of the increase in the cyst diameter should be precisely evaluated whenever such a tendency is observed.
We showed that all the cysts with an increase ratio of 100 % or more were malignant lesions, and that all ten benign lesions had an increase ratio of less than 100 % (Fig. 2). The increase ratio might also reflect the ability to undergo mucus hyper-production. The increase ratio, however, does not include a temporal element, allowing it to be used in a simple and practical manner.
Conclusion
During the follow-up period if an MN occurs in a patient with BD-IPMN, surgical resection should be immediately performed. The incidence of malignancy is higher in BD-IPMNs with an increase in the MPD diameter or an increase ratio of 100 % or more in the cyst diameter than the other cases, thus resection is also recommended for such cases.
References
Tanaka M, Fernandez-del Castillo C, Adsay V et al (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12(3):183–197 Epub 2012/06/13
Itai Y, Ohhashi K, Nagai H et al (1986) “Ductectatic” mucinous cystadenoma and cystadenocarcinoma of the pancreas. Radiology 161(3):697–700 Epub 1986/12/01
Brugge WR, Lauwers GY, Sahani D et al (2004) Cystic neoplasms of the pancreas. N Engl J Med 351(12):1218–1226 Epub 2004/09/17
Tanaka M, Chari S, Adsay V et al (2006) International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 6(1–2):17–32 Epub 2005/12/06
Bosman FT, Carneiro F, Hruban RH et al (eds) (2010) WHO classification of tumours of the digestive system, 4th edn. IARC Press, Lyon
Sobin LH, Wittekind C (eds) (2002) TNM classification of malignant tumours, 6th edn. Wiley, New York
Kang MJ, Jang JY, Kim SJ et al (2011) Cyst growth rate predicts malignancy in patients with branch duct intraductal papillary mucinous neoplasms. Clin Gastroenterol Hepatol 9(1):87–93 Epub 2010/09/21
Maguchi H, Tanno S, Mizuno N et al (2011) Natural history of branch duct intraductal papillary mucinous neoplasms of the pancreas: a multicenter study in Japan. Pancreas 40(3):364–370 Epub 2011/02/04
Yamaguchi T, Baba T, Ishihara T et al (2005) Long-term follow-up of intraductal papillary mucinous neoplasm of the pancreas with ultrasonography. Clin Gastroenterol Hepatol 3(11):1136–1143 Epub 2005/11/08
Irie H, Yoshimitsu K, Aibe H et al (2004) Natural history of pancreatic intraductal papillary mucinous tumor of branch duct type: follow-up study by magnetic resonance cholangiopancreatography. J Comput Assist Tomogr 28(1):117–122 Epub 2004/01/13
Rautou PE, Levy P, Vullierme MP et al (2008) Morphologic changes in branch duct intraductal papillary mucinous neoplasms of the pancreas: a midterm follow-up study. Clin Gastroenterol Hepatol 6(7):807–814 Epub 2008/02/29
Rodriguez JR, Salvia R, Crippa S et al (2007) Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology 133(1):72–79 quiz 309–10. Epub 2007/07/17
Schnelldorfer T, Sarr MG, Nagorney DM et al (2008) Experience with 208 resections for intraductal papillary mucinous neoplasm of the pancreas. Arch Surg 143(7):639–646 discussion 46. Epub 2008/07/23
Sugiyama M, Izumisato Y, Abe N et al (2003) Predictive factors for malignancy in intraductal papillary-mucinous tumours of the pancreas. Br J Surg 90(10):1244–1249 Epub 2003/09/30
Provinciali M, Smorlesi A (2005) Immunoprevention and immunotherapy of cancer in ageing. Cancer Immunol Immunother 54(2):93–106 Epub 2004/11/24
Burns EA, Leventhal EA (2000) Aging, immunity, and cancer. Cancer Control 7(6):513–522 Epub 2000/11/23
Fessler J, Ficjan A, Duftner C et al (2013) The impact of aging on regulatory T-cells. Front Immunol 4:231 Epub 2013/08/22
Vadasz Z, Haj T, Kessel A et al (2013) Age-related autoimmunity. BMC Med 11:94 Epub 2013/04/06
Tanno S, Nakano Y, Koizumi K et al (2010) Pancreatic ductal adenocarcinomas in long-term follow-up patients with branch duct intraductal papillary mucinous neoplasms. Pancreas 39(1):36–40 Epub 2009/09/12
Woo SM, Ryu JK, Lee SH et al (2009) Branch duct intraductal papillary mucinous neoplasms in a retrospective series of 190 patients. Br J Surg 96(4):405–411 Epub 2009/03/14
Yamaguchi K, Kanemitsu S, Hatori T et al (2011) Pancreatic ductal adenocarcinoma derived from IPMN and pancreatic ductal adenocarcinoma concomitant with IPMN. Pancreas 40(4):571–580 Epub 2011/04/19
Acknowledgments
None.
Source of financial support
None.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kato, Y., Takahashi, S., Gotohda, N. et al. Risk Factors for Malignancy in Branched-Type Intraductal Papillary Mucinous Neoplasms of the Pancreas During the Follow-Up Period. World J Surg 39, 244–250 (2015). https://doi.org/10.1007/s00268-014-2789-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-014-2789-3