Abstract
Purpose
The objectives of this study were to describe the distribution and the clinicopathological features of the most common causes for dental treatment needs during the hospitalization of cancer patients.
Methods
A retrospective cohort study of 2664 hospitalized cancer patients that analyzed the main dental treatment needs and dental procedures performed from January 2010 to December 2017.
Results
A total of 2664 medical patients were included in this study. Non-Hodgkin lymphoma (17.2%) was the most common cancer type, followed by leukemia (14.8%), and oral and oropharyngeal squamous cell carcinoma (10.5%). The most common reasons for patients’ hospitalization were chemotherapy protocols (18.8%), monitoring head and neck surgeries (9.7%), and febrile neutropenia (9.6%). The main motivation for the medical team to request dental evaluation was oral mucositis (22.8%) followed by oral pain or toothache (10.8%) and fungal, viral oral infections or traumatic oral lesions (9.9%). The dental treatment needs most observed were pain due to oral mucositis (17%), dental treatment prior to radiotherapy (RT), chemotherapy (CT) or bisphosphonate therapy (BP) (10.8%), teeth extractions (6.5%), and prophylactic photobiomodulation therapy (6.3%), whereas the most common dental treatments performed were oral hygiene protocols (30.2%), photobiomodulation therapy (prophylactic and curative) (21.7%), and dental treatment prior to cancer treatment initiation (RT, CT, and BP) (9.5%).
Conclusion
This study can be considered original in the oncologic context, providing new information about the most frequent dental treatment needs among a large population of hospitalized cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2018, the GLOBOCAN database presented an estimate of 18.1 million new cancer cases diagnosed worldwide and 9.6 million cancer-related deaths. In this scenario, malignant tumors of the lung, breast, prostate, skin, and oral cavity, as well as hematologic and lymphatic tumors are the most frequent cancer types [1, 2].
Cancer patients are often treated by surgery (SG), chemotherapy (CT), radiotherapy (RT), bone marrow transplantation, molecular targeted therapy, or a combination of these methods. The main causes of hospitalizations among cancer patients are symptoms related to disease progression or by toxicities (side effects) of oncologic treatment. In this context, impaired dental hygiene and oral lesions may lead to high rates of local (odontogenic infections) and systemic infections, such as respiratory diseases (ventilator-associated pneumonia), which have the potential to cause delays in, or interruptions to cancer treatment, as well as a decrease in the quality of life of patients. These oral complications secondary to cancer progression or related to oncologic treatment may also increase the overall treatment cost, due to the need for special diet (feeding tubes), analgesia with opioids, and prolonged hospitalization [3,4,5,6,7,8,9]. However, most of the previously published studies in this field focused on describing systemic complications in hospitalized cancer patients [8, 10, 11].
Although oral mucositis (OM), odontogenic (dental caries, abscesses, and periodontal disease), viral (herpes simplex virus) and fungal (oral candidosis) infections, and other soft tissue and jawbone lesions have been previously demonstrated as common oral complications among cancer patients in intensive care units [5, 8, 10,11,12,13], the patterns of oral complications and dental treatment needs among cancer inpatients are widely unknown.
Therefore, the aim of this study was to describe the distribution and the clinicopathological features of the most common causes of dental treatment needs among patients during the hospitalization period in infirmaries of a major cancer facility in Latin America.
Patients and methods
The present study was approved by the Ethics Committee of the School of Medicine of the University of Sao Paulo (Protocol no. 2.580.090), Sao Paulo, Brazil. This was a retrospective cohort study that analyzed the main dental treatment needs and dental procedures performed in hospitalized cancer patients treated at São Paulo State Cancer Institute (ICESP), Brazil, from January 2010 to December 2017. This study was performed following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [14].
Data collection
All patients included in this study were evaluated by the members of the Dental Oncology Service of ICESP during the hospitalization period following digital medical requests performed through the institutional electronic medical record system (Tasy, Java version; product #NOCTN306, Koninklijke Philips N.V., 2004–2017).
Patients’ epidemiologic and demographic data were retrieved and collected from the institutional electronic medical record system Tasy (Philips Clinical Informatics, Blumenau, Brazil), including gender, age, cancer diagnosis, clinical staging (according to the TNM Classification of Malignant Tumors (TNM); American Joint Committee on Cancer Staging System, 7th edition) [15], cancer treatment protocols, reasons for hospitalization, and medical specialties that requested a dental evaluation.
Clinicopathological aspects of the oral or dental complications that originated the medical requested as well as the patterns of dental treatment needs were also collected and further studied.
Anatomical sites of primary tumors of included patients were reported according to the International Classification of Diseases for Oncology (ICD–O–3, International Agency for Research on Cancer; see in https://www.iarc.fr).
Inclusion criteria
All hospitalized cancer patients presenting complete medical records who demanded dental assessment following medical requests in the study’s period were included.
Exclusion criteria
Subjects who refused oral evaluations or received medical discharge prior to oral examination were excluded from the study.
Statistical analysis
Data were analyzed with descriptive statistics (frequency and percent) using Microsoft Excel 2013 (Microsoft Corporation, Seattle, USA) and SPSS statistical package 17 for Windows (IBM, Chicago, USA) [16].
Results
Clinical features
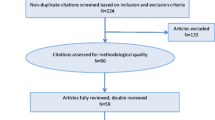
During the period of this retrospective cohort study, 137,279 patients were hospitalized at ICESP; of these, 3010 (2.20%) were evaluated by the Dental Oncology Service, following medical request. Three hundred and forty-six (11.5%) of these patients presented incomplete medical records or were patients who received medical discharge prior to oral examination, so they were excluded from the analyses. Hence, 2664 (1.95%) patients were included in this study.
Hospitalization
The mean time of hospitalization for studied patients was 3.2 days. Analysis by gender showed that 1513 (56.8%) patients were male, whereas 1151 (43.2%) were female. The patients’ ages ranged from 16 to 90 years and the mean age at hospitalization was 53.1 years. The most common cancer type was non-Hodgkin lymphoma (459 (17.2%)), followed by leukemia (395 (14.8%)), oral cavity, and oropharyngeal squamous cell carcinomas (280 (10.5%)) and multiple myeloma (174 (6.5%)). The patients were most frequently (1178; (44.2%)) diagnosed under a clinically advanced stage of diseases (III/IV). Patients undergoing or following CT protocols were those who more frequently demanded dental evaluation during the course of hospitalization (Table 1).
The most common medical reasons for patients’ hospitalization were CT protocols (especially hematological patients) (502; (18.8%)), hospitalizations for monitoring head and neck surgeries (258; (9.7%)), and febrile neutropenia (FN) (226; (8.5%)). Of the 226 patients with FN, 78 (34.5%) presented OM during the evaluation and 57 (25.2%) required dental procedures (tooth extraction due to abscesses or periodontal disease). Toothache was a “top five” cause for hospitalization (165; (6.2%)) among cancer patients.
Dental second opinion and treatment
The main motivation for the medical team to request dental evaluation were OM (607; (22.8%)) followed by oral pain or toothache (287; (10.8%)), fungal, viral oral infections, or traumatic oral lesions (263; (9.9%)) and prophylactic photobiomodulation therapy (241; (9%)). The medical specialties that requested dental assessment more frequently were clinical oncology (1080; (40.5%)), hematology (879; (33%)), intensive care (320; (12%)), and head and neck surgery (137; (5.2%)) (Table 2).
The most prevalent dental treatment needs observed in hospitalized cancer patients were pain due to OM (453; (17%)), dental treatment prior to the RT, CT, or bisphosphonates therapy (BP) (286; (10.8%)), teeth extractions (173; (6.5%)), and prophylactic photobiomodulation therapy (170; (6.3%)), whereas the most common dental treatments performed were oral hygiene protocols (806; (30.2%)), photobiomodulation therapy (prophylactic and curative) (577; (21.7%)), dental treatment prior to cancer treatment initiation (RT, CT, and BP) (254; (9.5%)), and teeth extraction (204; (7.7%)) (Table 3).
Discussion
This seems to be the first study in the English-language literature to analyze the patterns of dental needs in hospitalized oncologic patients from a Latin American population. This particular study was performed in the biggest public cancer hospital in Brazil, which provides medical assistance for patients of the entire country and, thus, may be considered a representative sample in oncologic terms as well as regarding the occurrence of oral complications in cancer inpatients. However, it is important to mention that the clinical demand reported in this study (1.95% of the hospital population) was based on patients who had a medical request for dental assistance/treatment. A prospective study with a proper sample size calculation will be necessary to confirm the results of this large cohort retrospective study.
The most recent report of GLOBOCAN [1] showed that the highest incidence of tumors in men was lung (14.5%) and prostate (13.5%) cancer, while in women it was breast (24.2%) and lung (8.4%) cancer. In the present study, the majority of hospitalized cancer patients evaluated were undergoing treatment for hematologic neoplasms (32%) and oral cavity and oropharyngeal cancer (15.3%), and this difference may result from the fact that oral toxicities are frequently more related to the cancer therapy performed than to the types of cancer. However, breast and lung cancers were also among the “top ten” malignant tumors of the population studied herein.
It is important to highlight that São Paulo State Cancer Institute is a quaternary cancer care center designed to assist highly complex cases in oncology. Thus, most of the patients (44.2%) included in this retrospective cohort study were undergoing treatment for advanced malignant tumors. Hence, the high demand for dental second opinions can be justified by the intense treatment protocols used in this inpatient service, such as aggressive surgeries combined with radiotherapy and chemotherapy.
Oncologic patients often require hospitalization not only for treating their malignant neoplasms (SG, CT, or RT) [2, 7, 8] but also due to toxicities resulting from cancer treatment [5, 12, 13, 17], or even for unpredictable needs that should preferably be managed in hospital facilities, such as opportunistic infections [11]. Approximately, 40% of CT-treated patients develop OM [10, 17]. The present study showed that the main reason for hospitalization was associated with complications of CT protocols (18.8%), in accordance with the findings reported by Gomes et al. (2018) [10], who described higher rates of hospitalization due to CT or toxicities related to the treatment.
Also, Numico et al. [11] performed a retrospective study with cancer patients and described that cancer treatment-related toxicities were the main reason (80.2%) for hospital admission. In our study, the main complications related to the oncological treatment were similar to those in Numico et al.’s [11] report, such as FN (9.6%), septic shock (8.9%), and OM (2.3%). In our sample, from 226 patients with FN, 78 (34.5%) had OM and 57 (25.2%) required dental procedures related to surgical and periodontal treatments (tooth extraction, draining of dental abscesses, or periodontal therapy, for example). The present study supports previous observations about the association of OM, periodontal diseases, and FN in hospitalized cancer patients [18,19,20].
As previously described in oncologic patients, OM is a common complication, which may result in severe pain, nutritional impairment, and increase the risk of local and systemic infections [21, 22]. Our results showed that OM was the most common oral alteration diagnosed in the evaluated population (17%), which was corroborated by the fact that it was also a leading (22.8%) reason for a dental evaluation request by the medical team. Remarkably, in this scenario, 577 (21.7%) patients demanded photobiomodulation therapy (prophylactic and curative) following institutional protocols previously published by our group [21].
The high rates of OM diagnosed among the patients included in this study were the consequence of the fact that most patients were undergoing systemic treatments for advanced cancer that were mostly based on cytotoxic CT protocols. This scenario may justify the high demand of medical requests performed by clinical oncology (1080; 40.5%) and hematology (879; 33%) medical teams.
It is relevant to mention that when it comes to the “top ten” cancers diagnosed in the current population, the frequency of hematological malignant tumors (38.5%) was similar to solid malignant tumors (29.6%). However, there was a broader distribution of entities in the scope of clinical oncology (oral carcinoma, oropharyngeal carcinoma, breast cancer, lung cancer, rectum cancer, laryngeal carcinoma, and nasopharyngeal carcinomas) than in the hematolymphoid context (non-Hodgkin lymphoma, leukemia, and multiple myeloma). In addition, most of the cancer diagnoses out of the “top ten” category and listed as “others” represent solid tumors in the treatment context of clinical oncology. In fact, as observed in the cohort of the study patients, the most commonly admitted cancer patients during cancer treatment or at the initiation of the treatments are those with hematological malignancies or aggressive solid tumors because oral toxicities are often more closely related to the cancer therapy performed than to the type of cancer.
Oral and oropharyngeal cancer (15.3%) were listed in the “top three” malignant tumors among the hospitalized population in this study, and this might explain why the Head and Neck Surgery team was the fourth specialty that requested dental evaluation more frequently. The treatment of oral and oropharyngeal cancer can involve SG, CT, and head and neck RT (HNRT) or a combination of these methods. However, although effective in tumor control, these treatments are associated with surgical sequelae, oral toxicities, and a consequent reduction in the quality of life of cancer populations [23, 24]. In this context, multidisciplinary teams are core to supporting these patients. The present study showed that the main dental treatment performed included oral hygiene protocols (30.2%), photobiomodulation therapy (prophylactic and curative) (21.7%), dental treatment prior to oncologic treatment (9.5%), and confection of obturator prosthesis (1.6%).
Fungal and virus infections in the oral cavity are common in immunocompromised patients [10, 25, 26]. Similarly, our results showed a prevalence of 5.6 and 5.1% for oral candidiasis and oral herpes simplex, respectively; while in previously published retrospective studies evaluating oncologic inpatients, the incidences ranged from 16.6 to 39.1% [3, 9,10,11]. This difference may be attributed to the evaluation of hospitalized patients with several cancer diagnoses as well as the variety of reasons that lead to their hospitalizations.
In conclusion, this study suggests that patients with hematological malignancies and head and neck cancer present higher dental treatment needs during the period of hospitalization, mainly because of oral pain due to OM, dental conditioning prior to cancer therapy, teeth extractions, and prophylactic photobiomodulation therapy, whereas the most common dental treatments performed were oral hygiene protocols, photobiomodulation therapy (prophylactic and curative), dental treatment prior to cancer treatment initiation, and teeth extraction.
Although this large cohort study originally reported the patterns of dental treatment needs in hospitalized cancer patients, generating results with the potential to clarify inpatients’ dental necessities and also to support managers in organizing dental teams in similar hospital settings, there are limitations to be considered, such as its retrospective nature, the lack of sample size calculation, and the fact that most diagnoses were mainly based on physician evaluation.
References
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144(8):1941–1953. https://doi.org/10.1002/ijc.31937
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386. https://doi.org/10.1002/ijc.29210
Silva AP, Caruso P, Jaguar GC, Carvalho PA, Alves FA (2014) Oral evaluation and procedures performed by dentists in patients admitted to the intensive care unit of a cancer center. Support Care Cancer 22(10):2645–2650. https://doi.org/10.1007/s00520-014-2233-0
Davies AN, Brailsford SR, Beighton D (2006) Oral candidosis in patients with advanced cancer. Oral Oncol 42(7):698–702. https://doi.org/10.1016/j.oraloncology.2005.11.010
Tai E, Guy GP, Dunbar A, Richardson LC (2017) Cost of cancer-related neutropenia or fever hospitalizations, United States, 2012. J Oncol Pract 13(6):e552–e561. https://doi.org/10.1200/JOP.2016.019588
Fischer DJ, Epstein JB, Yao Y, Wilkie DJ (2014) Oral health conditions affect functional and social activities of terminally ill cancer patients. Support Care Cancer 22(3):803–810
Lee MK, Dodson TB, Nalliah RP, Karimbux NY, Allareddy V (2014) Nine-year trend analysis of hospitalizations attributed to oral and oropharyngeal cancers in the United States. Oral Surg Oral Med Oral Pathol Oral Radiol 118(1):47–67. https://doi.org/10.1016/j.oooo.2013.01.019
Lee MK, Nalliah RP, Kim MK, Elangovan S, Allareddy V, Kumar-Gajendrareddy P, Allareddy V (2011) Prevalence and impact of complications on outcomes in patients hospitalized for oral and oropharyngeal cancer treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 112(5):581–591. https://doi.org/10.1016/j.tripleo.2011.06.032
Lev A, Aied AS, Arshed S (2015) The effect of different oral hygiene treatments on the occurrence of ventilator associated pneumonia (VAP) in ventilated patients. J Infect Prev 16(2):76–81. https://doi.org/10.1177/1757177414560252
Gomes AOF, Silva Junior A, Noce CW, Ferreira M, Maiolino A, Torres SR (2018) The frequency of oral conditions detected in hematology inpatients. Hematol Transfus Cell Ther 40(3):240–244. https://doi.org/10.1016/j.htct.2018.02.006
Numico G, Cristofano A, Mozzicafreddo A, Cursio OE, Franco P, Courthod G, Trogu A, Malossi A, Cucchi M, Sirotovà Z, Alvaro MR, Stella A, Grasso F, Spinazzé S, Silvestris N (2015) Hospital admission of cancer patients: avoidable practice or necessary care? PLoS One 10(3):e0120827. https://doi.org/10.1371/journal.pone.0120827
Boers-Doets CB, Epstein JB, Raber-Durlacher JE, Ouwerkerk J, Logan RM, Brakenhoff JA, Lacouture ME, Gelderblom H (2012) Oral adverse events associated with tyrosine kinase and mammalian target of rapamycin inhibitors in renal cell carcinoma: a structured literature review. Oncologist 17(1):135–144. https://doi.org/10.1634/theoncologist.2011-0111
Terezakis E, Needleman I, Kumar N, Moles D, Agudo E (2011) The impact of hospitalization on oral health: a systematic review. J Clin Periodontol 38(7):628–636. https://doi.org/10.1111/j.1600-051X.2011.01727.x
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative STROBE (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474
Stephen BH, Steven RC, Thomas BN (2011) Designing cross-sectional and cohort studies. In: Smith J (ed) Designing clinical research, 4rth edn. Lippincott Williams & Wilkins, Philadelphia, pp 85–96
de Lacerda Vidal CF, Vidal AK, Monteiro JG Jr, Cavalcanti A, Henriques APC, Oliveira M, Godoy M, Coutinho M, Sobral PD, Vilela CÂ, Gomes B, Leandro MA, Montarroyos U, Ximenes RA, Lacerda HR (2017) Impact of oral hygiene involving toothbrushing versus chlorhexidine in the prevention of ventilator-associated pneumonia: a randomized study. BMC Infect Dis 17(1):112. https://doi.org/10.1186/s12879-017-2188-0
Basile D, Di Nardo P, Corvaja C, Garattini SK, Pelizzari G, Lisanti C, Bortot L, Da Ros L, Bartoletti M, Borghi M, Gerratana L, Lombardi D, Puglisi F (2019) Mucosal injury during anti-cancer treatment: from pathobiology to bedside. Cancers (Basel) 11(6):857. https://doi.org/10.3390/cancers11060857
Fernandes LL, Torres SR, Garnica M, de Souza GL, Junior AS, de Vasconcellos ÁC, Cavalcanti W, Maiolino A, de Barros Torres MC (2014) Oral status of patients submitted to autologous hematopoietic stem cell transplantation. Support Care Cancer 22(1):15–21. https://doi.org/10.1007/s00520-013-1940-2
Djuric M, Hillier-Kolarov V, Belic A, Jankovic L (2006) Mucositis prevention by improved dental care in acute leukemia patients. Support Care Cancer 14(2):137–146
Zecha JAEM, Raber-Durlacher JE, Laheij AMGA, Westermann AM, Epstein JB, de Lange J, Smeele LE (2019) The impact of the oral cavity in febrile neutropenia and infectious complications in patients treated with myelosuppressive chemotherapy. Support Care Cancer 27(10):3667–3679. https://doi.org/10.1007/s00520-019-04925-8
Brandão TB, Morais-Faria K, Ribeiro ACP, Rivera C, Salvajoli JV, Lopes MA, Epstein JB, Arany PR, de Castro G Jr, Migliorati CA, Santos-Silva AR (2018) Locally advanced oral squamous cell carcinoma patients treated with photobiomodulation for prevention of oral mucositis: retrospective outcomes and safety analyses. Support Care Cancer 26(7):2417–2423. https://doi.org/10.1007/s00520-018-4046-z
Lalla RV, Saunders DP, Peterson DE (2014) Chemotherapy or radiation-induced oral mucositis. Dent Clin N Am 58(2):341–349. https://doi.org/10.1016/j.cden.2013.12.005
Brandão TB, Vechiato Filho AJ, Batista VE, de Oliveira MC (2016) Santos-Silva AR (2016) Obturator prostheses versus free tissue transfers: a systematic review of the optimal approach to improving the quality of life for patients with maxillary defects. J Prosthet Dent 115(2):247–253
Reyes-Gibby CC, Melkonian SC, Hanna EY, Yeung SJ, Lu C, Chambers MS, Banala SR, Gunn GB, Shete SS (2017) Cohort study of oncologic emergencies in patients with head and neck cancer. Head Neck 39(6):1195–1204
Chen YK, Hou HA, Chow JM, Chen YC, Hsueh PR, Tien HF (2011) The impact of oral herpes simplex virus infection and candidiasis on chemotherapy-induced oral mucositis among patients with hematological malignancies. Eur J Clin Microbiol Infect Dis 30(6):753–759
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The present study was approved by the Ethics Committee of the School of Medicine of the University of Sao Paulo (Protocol no. 2.580.090), Sao Paulo, Brazil.
Control of the Data
The authors have full control of all primary data and agree to allow the journal to review our data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Oliveira, M.C.Q., Lebre Martins, B.N.F., Santos-Silva, A.R. et al. Dental treatment needs in hospitalized cancer patients: a retrospective cohort study. Support Care Cancer 28, 3451–3457 (2020). https://doi.org/10.1007/s00520-019-05202-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05202-4