Abstract
Purpose
The well-established clinical efficacy of photobiomodulation (PBM) therapy in management of oral mucositis (OM) is leading to increasing use in oncology care. This protection and enhanced repair of damage to mucosal tissue have led to the question of the potential effects of PBM therapy on pre-malignant and malignant cells. The purpose of this study was to examine the outcome of cancer therapy and incidence of tumor recurrence in locally advanced oral squamous cell carcinoma (OSCC) patients treated with PBM therapy for OM.
Methods
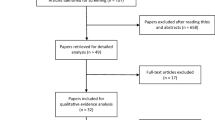
A retrospective clinical analysis of 152 advanced OSCC patients treated with prophylactic PBM therapy for radiotherapy-induced OM from January 2009 to December 2014 was conducted.
Results
Of the 152 OSCC patients treated with PBM therapy in this study, 19 (12.5%) had stage III and 133 (87.5%) had stage IV tumors. Of these, 52 (34.2%) received initial treatment with surgery followed by adjuvant radiotherapy, 94 (61.8%) with exclusive chemoradiation, and 6 (4%) with induction chemotherapy followed by surgery and radiotherapy. After a mean follow-up of 40.84 (± 11.71) months, the overall survival and disease-free survival rates were 46.7 and 51.8%, respectively. Forty-five (29.6%) patients developed local-regional recurrence, 10 (6.57%) patients developed distant relapse, and 19 (12.5%) developed new (second) primary tumors.
Conclusions
Clinicopathological features and survival outcomes in the PBM-treated patients were similar to previously published data for conventional treatments in patients with advanced OSCC. In this study, prophylactic use of PBM therapy did not impact treatment outcomes of the primary cancer, recurrence or new primary tumors, or survival in advanced OSCC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Photobiomodulation (PBM), previously known as low-level light/laser therapy (LLLT), has been used for many years to treat patients with a variety of diseases and conditions. Due to its stimulatory biological effects, the potential of PBM to promote malignant transformation or tumor cell proliferation has been questioned. With the growing popularity of this therapy, this appears to be a key unresolved question [1]. The wavelengths used in PBM therapy (visible and near-infrared) have non-ionizing characteristics, and their low dose has been shown to be incapable of inducing mutagenesis or genotoxicity in vitro [2]. However, concern regarding the potential for PBM therapy to stimulate malignant cell proliferation in vivo remains to be investigated in the clinical context.
Most of the PBM studies on tumor cells have been performed in laboratory settings, and their results remain equivocal [3,4,5,6,7,8,9]. In addition, in vitro cell culture-based studies do not account for effects of the tumor microenvironment and immune system that play critical roles in vivo, making it difficult to extrapolate laboratory experimental results to human outcomes. Interestingly, a few animal studies have noted tumor-suppressing effects of PBM therapy suggesting there maybe indirect, synergistic effects on tumor cells or the host immunosurveillance system [3,4,5,6,7,8,9].
Oral mucositis (OM) is a severe complication of high-dose radiation therapy and chemotherapy for head and neck tumors that generates intense pain, interferes with nutrition (need for parenteral nutritional support), increases risk for local and systemic infections, result in increased utilization of analgesics including opioids, may lead to hospital admission, and affects overall prognosis of cancer therapy [10]. The Multinational Association of Supportive Care in Cancer (MASCC) and International Society of Supportive Care in Cancer (ISOO) have developed comprehensive evidence-based mucositis management guidelines. In its most recent update, PBM therapy is recommended as an effective adjunctive treatment in managing OM. This group recommended that PBM be used to prevent OM in patients receiving hematopoietic stem cell transplant conditioned with high-dose chemotherapy, with or without total body irradiation. The guidelines also suggest the use of PBM to prevent OM in patients undergoing head and neck radiotherapy [11]. Because of these recommendations and the potential for broader use of PBM treatment, it is imperative clinical safety of PBM therapy be documented.
Although PBM therapy has been used for many years to prevent and treat OM in head and neck cancer populations, there has been no attempt, to our knowledge, examining its effects on clinical incidences of oral cancer recurrences or new oral cavity primary tumors. The present study examined a single-center database retrospectively to examine clinicopathological features, treatment, and survival outcomes in locally advanced oral squamous cell carcinoma (OSCC) patients treated with radiotherapy, with or without chemotherapy that used PBM therapy to prevent OM.
Methods
Study protocol
This study was approved by the Ethics Committee of the School of Medicine of the University of Sao Paulo, Sao Paulo, Brazil (Protocol# 1.897.352) and was conducted in accordance with the Declaration of Helsinki. This retrospective, observational clinical study examined clinicopathological features, treatments, and survival outcomes of locally advanced (stage III and IV, M0) OSCC patients. The data collection followed the guideline for reporting observational studies as per Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [12]. The study included data from a single institution (Sao Paulo State Cancer Institute, ICESP, Brazil), from January 2009 to December 2014.
Inclusion criteria
All subjects included in this study were treated with post-surgical or cisplatin chemotherapy with concomitant radiotherapy using a 6MV linear accelerator (Synergy Platform, Elekta AB, Stockholm, Sweden). All included subjects received the current institutional standard-of-care PBM protocol (details below) for prevention of OM.
Exclusion criteria
Subjects who missed one or more radiotherapy sessions, chemotherapy cycles, or PBM sessions were considered to have received incomplete treatment and were excluded from the study.
Clinical parameters and follow-up
The institutional electronic medical record system was reviewed, and the following data were abstracted: age, gender, tumor topography, alcohol consumption and smoking habit, clinical cancer stage classification (American Joint Committee on Cancer Staging System, 7th edition), and treatment modalities used in cancer treatment, including total radiation dose prescribed to the primary tumor volume (Gy). Patients were evaluated clinically every 3 months and with imaging using computed tomography and ultrasonography 12 months after completing therapy. The outcomes of therapy were recorded, as well as any clinical evidence of new potentially malignant or malignant lesions in the oral cavity or regional sites. The time that patients were followed post-radiation therapy was recorded. Overall survival (OS) rate, disease-free survival (DFS) rate, the incidence of recurrences (local-regional and distant relapse rates), or new (second) primary tumors were used as primary outcome measures.
Photobiomodulation protocol
PBM therapy is the standard of care for OM prevention at the study center, and all patients subjected to radiotherapy for oral cavity cancers receive PBM treatment prophylactically. All patients underwent full oral examination and comprehensive dental treatment before beginning radiotherapy. Trained dentists administered PBM therapy on an outpatient basis and treatment consisted of daily applications for 5 consecutive days (Monday to Friday) throughout radiation therapy, immediately before each radiotherapy session. All patients were treated by a Twin Flex (MMOptics, São Carlos, Brazil) PBM device. Details of PBM parameters used are described in Table 1. During each intraoral PBM session, the treatment probe was turned on when positioned perpendicular to several points of seven different oral mucosa sites, 10 s per point (Fig. 1). These sites included the oral commissures (1 point for each commissure), lips mucosae (3 points for each lip), buccal mucosae (3 points for each side), lateral borders of the tongue (3 points for each side), ventral tongue (2 points), anterior floor of the mouth (2 points), and soft palate (2 points). PBM therapy was never delivered over an active tumor site. When tumors were surgically removed prior to radiation, the laser probe was activated over the entire surgical site.
Clinical images demonstrating intraoral photobiomodulation therapy protocol at our center. The laser probe is represented by the red circles at seven distinct sites on the oral mucosa including oral commissures (a), labial mucosae (b, c), lateral borders of the tongue (d, e), ventral tongue (f), anterior floor of the mouth (f), buccal mucosae (g, H), and soft palate (i). PBM therapy was not delivered over active tumor area (e)
Oral mucositis assessments
Participants were assessed for OM at baseline (first day of radiotherapy), then daily (excluding weekends) until the last day of therapy. OM was graded using the Common Terminology Criteria for Adverse Events, National Cancer Institute (CTAE, Version 4.0, 2010). PBM sessions were documented daily in electronic medical records by dentists who performed full oral examinations and OM assessments.
Statistical analysis
Data obtained in the study were analyzed statistically with SAS software version 9.3 (SAS Institute Inc., Cary, N.C., USA) by using descriptive statistics. Results were expressed as mean values, standard deviation, and percentages. Clinicopathologic results, treatment outcomes, and survival data were compared with previously published randomized controlled trials including survival rates of advanced OSCC patients treated with multimodal therapy.
Results
From a total of 413 patients potentially eligible for the analysis, 152 (36.8%) cases of histologically confirmed OSCC patients who had received PBM therapy for OM prevention met the inclusion criteria and were included in this study. Clinicopathologic patient characteristics, treatment modalities, and survival outcomes are summarized in Table 2. The mean age was 59.2 years, and there were more men (74.3%) than women (25.7%). Most patients were diagnosed with primary lateral border of the tongue (46%) squamous cell carcinomas, followed by the floor of the mouth (17.1%) and retromolar area (9.9%). All patients presented with local-regionally advanced disease, of which 19 (12.5%) were classified as stage III and 133 (87.5%) as stage IV. Of these patients, 52 (34.2%) received initial treatment with surgery followed by adjuvant radiotherapy, 94 (61.8%) were treated with chemoradiation, and 6 (4%) with induction chemotherapy followed by surgery and radiotherapy.
All patients were subjected to clinical postoperative or cisplatin-associated radiation protocols. Radiation volumes encompassed the primary site and areas of lymph nodes at risk and received cumulative doses that ranged from 60 to 70 Gy (2 Gy/day; 5 days/week from Monday to Friday). Six patients (4%) received induction chemotherapy with paclitaxel 175 mg/m2 combined with cisplatin 75 mg/m2 intravenously repeating every 21 days (TP regimen); 94 (61.8%) patients received concomitant chemotherapy based on cisplatin 100 mg/m2 on days 1, 22, and 43 of radiotherapy (CDDP regimen), and 52 (34. 2%) patients received post-surgical radiotherapy.
Systematic examination of the oral mucosa was performed daily before each intraoral PBM session and failed to detect any evidence of new potentially malignant or malignant lesions in the oral cavity or regional sites during the PBM protocol (Fig. 2). After a mean follow-up of 40.8 (± 11.7) months, the OS and DFS rates were 46.7 and 51.8%, respectively. Forty-five (29. 6%) patients developed local-regional recurrence, 10 (6.6%) patients developed distant relapse, and 19 (12. 5%) patients developed new (second) primary tumors (Table 2). All patients experienced some grade of OM during the treatment period. The appearance of severe mucositis (grades 3/4) was delayed to the last 2 weeks of treatment. The incidence of grade 3 and grade 4 mucositis in the last week of radiotherapy was 23 and 1%, respectively.
Clinical images for the use of photobiomodulation therapy to prevent oral mucositis. The top images show the frontal (a) and lateral (b) views of a locally advanced tongue squamous cell carcinoma prior to beginning of chemoradiation. The bottom images show frontal (c) and lateral (d) views demonstrating complete clinical resolution of the primary tumor after the conclusion of last session of radiation treatment
Discussion
This was a retrospective, single-center study examining 152 patients with locally advanced OSCC patients treated with PBM to prevent OM. Despite aggressive cancer treatment protocols, after a mean follow-up time of 40.8 (± 11.7) months, OS and DFS rates in the current series were only 46.7 and 51.8%, respectively. The survival outcomes of the present study compare favorably with those reported in the literature where OS rates ranged from 42 to 73% and DFS rates ranged from 45 to 85% (Table 3) [17,18,19,20]. Similarly, recent reports described local-regional recurrence rates that ranged from 10 to 34% [21] as reported in this study as well (29.6%) and represented the most frequent cause of treatment failure. Distant failure rates (6.6%) were in accordance with previous randomized clinical trials in which the incidence of distant metastasis has ranged from 5 to 12.9% [20]. The incidence of new (second) primary tumors observed in the current series (12.5%) was also comparable with that of previous clinical studies, which found an approximate incidence of 15% in all stages of OSCC [18].
The demographic characteristics of the patients included in this study were also similar to those of other OSCC series and mainly composed of elderly male patients with a history of tobacco and alcohol consumption [14, 18, 19]. The treatment approaches used in this study were similar to those used at most major oncology centers that include surgery followed by radiotherapy and chemotherapy in case of high-risk pathological features or primary chemotherapy and radiation for patients whose tumors are technically or functionally unresectable [20]. All patients included in the present study were managed with postoperative radiotherapy or cisplatin-associated chemo-radiation protocols.
Multiple primary tumors can arise by “field cancerization” in which the oral and oropharyngeal mucosa have been preconditioned by long-term exposure to tobacco and alcohol-related carcinogens. As a consequence, multiple carcinomas may develop as a result of independent or additional mutations. Results of the present study suggest that PBM therapy is not capable of promoting mutagenesis in clonally related dormant tumor cells. Thus, PBM therapy does not appear to increase risk of recurrent or new primary tumors within the treatment field [1]. Despite the aggressive multi-modality therapy noted in this study, disease outcomes have remained poor as noted with high incidences (87.5%) of stage IV tumors. Long-term overall survival and tumor control rates still remain unsatisfactory in advanced OSCC and remain a challenging disease to treat effectively [21, 22]. A summary of results reported in the literature from randomized controlled trials on treatments and survival outcomes in patients with OSCC is presented in Table 3. These analyses showed treatment with multimodal therapy, and disease outcomes do not demonstrate a significant difference compared to results from the current series that had additional PBM therapy.
Our study failed to identify discrete relationship between the PBM protocol used for preventing OM and increased rates of local-regional recurrences, distant failures, new (second) primary tumors, and, finally reduced OS or DFS. Similarly, no evidence of malignant transformation of potentially malignant lesions, such as oral leukoplakia or erythroplakia, was identified in the oral cavity or regional sites during the PBM sessions. It should be noted that the current PBM protocol followed previous suggestions for higher dose administration for increased efficacy in reducing incidence of grade 3 (23%) and grade 4 (1%) mucositis compared to prior clinical studies [23]. A review of the current literature noted one prior controlled, human study with long-term follow-up of 94 patients with nasopharynx, oropharynx, and hypopharynx tumors [24]. The authors noted PBM therapy appeared to improve survival outcomes in head and neck cancer patients treated with chemoradiation. The authors attribute these to the improved quality of life enabling compliance with cancer treatment regimens as well as better overall general health likely leading to improved response to therapy.
The lack of deleterious effects of PBM therapy upon tumor recurrence rates or patient survival should be interpreted with caution given the small number of patients as well as the retrospective nature of this study. In addition, the current study did not include a concurrent control group as all OSCC patients are treated at our institution with PBM for prevention of OM as routine standard of care. We attempted to address this issue by comparing the results of this study with previously published, randomized controlled trials that included treatment and survival outcomes of patients with OSCC treated with multimodal therapy. Therefore, the present findings should be considered hypothesis-generating rather than concrete proof of PBM safety and can be used to design definitive clinical studies in the future.
In summary, this retrospective analysis examined treatment outcomes in advanced OSCC patients that were treated with PBM for prevention of OM. The results of this study noted PBM did not impact incidence of local-regional or distant control and survival outcomes in OSCC patients compared to conventional interventions alone. This study suggests that PBM therapy is a safe clinical modality for prevention of OM in OSCC patients. Future prospective, randomized controlled trials would be ideal to further validate these results.
References
Sonis ST, Hashemi S, Epstein JB, Nair RG, Raber-Durlacher JE (2016) Could the biological robustness of low level laser therapy (Photobiomodulation) impact its use in the management of mucositis in head and neck cancer patients. Oral Oncol 54:7–14. https://doi.org/10.1016/j.oraloncology.2016.01.005
Khan I, Tang E, Arany P (2015) Molecular pathway of near-infrared laser phototoxicity involves ATF-4 orchestrated ER stress. Sci Rep 5(1). https://doi.org/10.1038/srep10581
Myakishev-Rempel M, Stadler I, Brondon P, Axe DR, Friedman M, Nardia FB, Lanzafame R (2012) A preliminary study of the safety of red light phototherapy of tissues harboring cancer. Photomed Laser Surg 30(9):551–558. https://doi.org/10.1089/pho.2011.3186
de C Monteiro JS, de Oliveira SC, Reis Júnior JA, Gurgel CA, de Souza SC, Pinheiro AL, dos Santos JN (2013) Effects of imiquimod and low-intensity laser (lambda660 nm) in chemically induced oral carcinomas in hamster buccal pouch mucosa. Lasers Med Sci 28(3):1017–1024. https://doi.org/10.1007/s10103-012-1192-2
Sperandio FF, Giudice FS, Corrêa L, Pinto DS Jr, Hamblin MR, de Sousa SC (2013) Low-level laser therapy can produce increased aggressiveness of dysplastic and oral cancer cell lines by modulation of Akt/mTOR signaling pathway. J Biophotonics. https://doi.org/10.1002/jbio.201300015
Gomes Henriques ÁC, Ginani F, Oliveira RM, Keesen TS, Galvão Barboza CA, Oliveira Rocha HA, de Castro JF, Della Coletta R, de Almeida Freitas R (2014) Low-level laser therapy promotes proliferation and invasion of oral squamous cell carcinoma cells. Lasers Med Sci. https://doi.org/10.1007/s10103-014-1535-2
Ottaviani G, Martinelli V, Rupel K, Caronni N, Naseem A, Zandonà L, Perinetti G, Gobbo M, Di Lenarda R, Bussani R, Benvenuti F, Giacca M, Biasotto M, Zacchigna S (2016) Laser therapy inhibits tumor growth in mice by promoting immune surveillance and vessel normalization. EBioMedicine 11:165–172. https://doi.org/10.1016/j.ebiom.2016.07.028
Barasch A, Raber-Durlacher J, Epstein JB, Carroll J (2016) Effects of pre-radiation exposure to LLLT of normal and malignant cells. Support Care Cancer 24(6):2497–2501. https://doi.org/10.1007/s00520-015-3051-8
Frigo L, Luppi JS, Favero GM, Maria DA, Penna SC, Bjordal JM, Bensadoun RJ, Lopes-Martins RA (2009) The effect of low-level laser irradiation (in-Ga-al-AsP - 660 nm) on melanoma in vitro and in vivo. BMC Cancer 9(1). https://doi.org/10.1186/1471-2407-9-404
Villa A, Sonis ST (2015) Mucositis: pathobiology and management. Curr Opin Oncol 27(3):159–164. https://doi.org/10.1097/CCO.0000000000000180
Lalla RV, Bowen J, Barasch A, Elting L, Epstein J, Keefe DM, Mc Guire DB, Migliorati C, Nicolatou-Galitis O, Peterson DE, Raber-Durlacher JE, Sonis ST, Elad S, Mucositis Guidelines Leadership Group of the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO) (2014) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 120(10):1453–1461. https://doi.org/10.1002/cncr.28592
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiativem (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. https://doi.org/10.1016/S0140-6736(07)61602-X
Licitra L, Grandi C, Guzzo M, Mariani L, Lo Vullo S, Valvo F, Quattrone P, Valagussa P, Bonadonna G, Molinari R, Cantù G (2003) Primary chemotherapy in resectable oral cavity squamous cell cancer: a randomized controlled trial. J Clin Oncol 21(2):327–333. https://doi.org/10.1200/JCO.2003.06.146
Zhong LP, Zhang CP, Ren GX, Guo W, William WN Jr, Sun J, Zhu HG, Tu WY, Li J, Cai YL, Wang LZ, Fan XD, Wang ZH, Hu YJ, Ji T, Yang WJ, Ye WM, Li J, He Y, Wang YA, Xu LQ, Wang BS, Kies MS, Lee JJ, Myers JN, Zhang ZY (2013) Randomized phase III trial of induction chemotherapy with docetaxel, cisplatin, and fluorouracil followed by surgery versus up-front surgery in locally advanced resectable oral squamous cell carcinoma. J Clin Oncol 31(6):744–751. https://doi.org/10.1200/JCO.2012.43.8820
Bossi P, Lo Vullo S, Guzzo M, Mariani L, Granata R, Orlandi E, Locati L, Scaramellini G, Fallai C, Licitra L (2014) Preoperative chemotherapy in advanced resectable OCSCC: long-term results of a randomized phase III trial. Ann Oncol 25(2):462–466. https://doi.org/10.1093/annonc/mdt555
Zhong LP, Zhang CP, Ren GX, Guo W, William WN Jr, Hong CS, Sun J, Zhu HG, Tu WY, Li J, Cai YL, Yin QM, Wang LZ, Wang ZH, Hu YJ, Ji T, Yang WJ, Ye WM, Li J, He Y, Wang YA, Xu LQ, Zhuang Z, Lee JJ, Myers JN, Zhang ZY (2015) Long-term results of a randomized phase III trial of TPF induction chemotherapy followed by surgery and radiation in locally advanced oral squamous cell carcinoma. Oncotarget doi: https://doi.org/10.18632/oncotarget.4531, 6, 21, 18707, 18714
Ruggeri EM, Carlini P, Pollera CF, De Marco S, Ruscito P, Pinnarò P, Nardi M, Giannarelli D, Cognetti F (2005) Long-term survival in locally advanced oral cavity cancer: an analysis of patients treated with neoadjuvant cisplatinbased chemotherapy followed by surgery. Head Neck 27(6):452–458. https://doi.org/10.1002/hed.20190
Zhang H, Dziegielewski PT, Biron VL, Szudek J, Al-Qahatani KH, O'Connell DA, Harris JR, Seikaly H (2013) Survival outcomes of patients with advanced oral cavity squamous cell carcinoma treated with multimodal therapy: a multi-institutional analysis. J Otolaryngol Head Neck Surg 42(1):30. https://doi.org/10.1186/1916-0216-42-30
Hasegawa T, Yanamoto S, Otsuru M, Yamada SI, Minamikawa T, Shigeta T, Naruse T, Suzuki T, Sasaki M, Ota Y, Umeda M, Komori T (2017) Retrospective study of treatment outcomes after postoperative chemoradiotherapy in Japanese oral squamous cell carcinoma patients with risk factors of recurrence. Oral Surg Oral Med Oral Pathol Oral Radiol 123(5):524–530. https://doi.org/10.1016/j.oooo.2016.11.014
Goldstein DP, Bachar GY, Lea J, Shrime MG, Patel RS, Gullane PJ, Brown DH, Gilbert RW, Kim J, Waldron J, Perez-Ordonez B, Davis AM, Cheng L, Xu W, Irish JC (2013) Outcomes of squamous cell cancer of the oral tongue managed at the Princess Margaret hospital. Head Neck. 35(5):632–641. https://doi.org/10.1002/hed.23001
Blanchard P, Baujat B, Holostenco V, Bourredjem A, Baey C, Bourhis J, Pignon JP, MACH-CH Collaborative group (2011) Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): a comprehensive analysis by tumour site. Radiother Oncol 100(1):33–40. https://doi.org/10.1016/j.radonc.2011.05.036
Marta GN, Riera R, Bossi P, Zhong LP, Licitra L, Macedo CR, de Castro JG, Carvalho AL, William WN Jr, Kowalski LP (2015) Induction chemotherapy prior to surgery with or without postoperative radiotherapy for oral cavity cancer patients: systematic review and meta-analysis. Eur J Cancer 51(17):2596–2603. https://doi.org/10.1016/j.ejca.2015.08.007
Gouvêa de Lima A, Villar RC, de Castro G Jr, Antequera R, Gil E, Rosalmeida MC, Federico MH, Snitcovsky IM (2012) Oral mucositis prevention by low-level laser therapy in head-and-neck cancer patients undergoing concurrent chemoradiotherapy: a phase III randomized study. Int J Radiat Oncol Biol Phys 82(1):270–275. https://doi.org/10.1016/j.ijrobp.2010.10.012
Antunes HS, Herchenhorn D, Small IA, Araújo CMM, Viégas CMP, de Assis RG, Dias FL, Ferreira CG (2017) Long-term survival of a randomized phase III trial of head and neck cancer patients receiving concurrent chemoradiation therapy with or without low-level laser therapy (LLLT) to prevent oral mucositis. Oral Oncol 71:11–15. https://doi.org/10.1016/j.oraloncology.2017.05.018
Acknowledgments
The authors would like to gratefully acknowledge the financial support of the São Paulo Research Foundation (FAPESP) (process numbers 2013/00429-7; 2013/18402-8 and 2012/06138-1) as well as the National Council for Scientific and Technological Development—CNPq.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Thaís Bianca Brandão, Cesar Augusto Migliorati and Alan Roger Santos-Silva are shared senior authors
Rights and permissions
About this article
Cite this article
Brandão, T.B., Morais-Faria, K., Ribeiro, A.C.P. et al. Locally advanced oral squamous cell carcinoma patients treated with photobiomodulation for prevention of oral mucositis: retrospective outcomes and safety analyses. Support Care Cancer 26, 2417–2423 (2018). https://doi.org/10.1007/s00520-018-4046-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4046-z