Abstract
Purpose
Several studies have analyzed late complications associated with totally implantable venous access ports (TIVAP) implantation via the internal jugular vein (IJV); however, the reported results are inconclusive. The aim of the study is to elucidate the characteristics and risk factors of late complications associated with TIVAP implantation via the IJV.
Methods
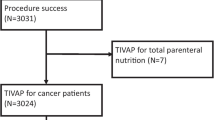
The study included 482 patients who underwent TIVAP implantation for long-term chemotherapy and/or nutritional support between April 2012 and December 2017. Most patients (95.2%) had malignant diseases. Events requiring TIVAP removal were defined as TIVAP-related complications.
Results
The median TIVAP and global follow-ups were 319 days (IQR 152–661) and 218,971 catheter days, respectively. The 3-year cumulative TIVAP availability rate was 70%. There were 44 complications (incidence of 9.1%; 0.201 complications/1000 catheter days). Infectious, catheter-related, and port-related complications occurred in 21, 14, and 9 patients, respectively with infectious complications occurring earlier and more frequently than catheter- and port-related complications. Multivariate analysis revealed that age < 65 years and presence of non-gastrointestinal diseases were significant unfavorable factors for TIVAP-related complications. Patients with 1 and 2 of these factors had an elevated risk (2.2 and 5.4 times, respectively) compared with those without.
Conclusions
Among the late complications associated with TIVAP implantation via the IJV, infectious complications occur earlier and more frequently than catheter- and port-related complications. Patients with an age < 65 years and having non-gastrointestinal diseases have a significantly high risk of TIVAP-related complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Totally implantable venous access ports (TIVAP) have been widely used as a simple and safe means to access the vascular system for intravenous administration of chemotherapeutic drugs and nutritional supportive care of patients with malignancies or insufficient gastrointestinal function [1,2,3]. A secure venous access is required for long-term chemotherapy and nutritional support. A TIVAP can be implanted via the basilic vein, subclavian vein, or external or internal jugular vein (IJV). Puncturing of the subclavian vein is associated with serious complications including pneumothorax, hemothorax, and catheter pinch-off in the costoclavicular space [2,3,4]. A TIVAP via the basilic vein is associated with a higher risk of major complications in patients with breast cancer [5]. On the other hand, implantation of a TIVAP via the IJV can be performed safely [6, 7]; therefore, the IJV has been routinely selected as the insertion vein for TIVAP since 2012 in our institute.
Late complications associated with the TIVAP include infection, thrombosis, occlusion, rupture, dislocation, catheter kinking, rotation and flip of the port, and skin ulceration around the catheter or port [8]. There have been several studies on the late complications of a TIVAP via the IJV; however, they were inconclusive due to several factors including small number of cases, inconsistent definition of TIVAP-related complications, and insufficient analysis [9,10,11,12]. Therefore, the aim of this study was to analyze the characteristics and risk factors of late complications of TIVAP via IJV.
Patients and methods
We retrospectively reviewed a database of patients who had undergone subcutaneous implantation of TIVAP via the IJV at the Japanese Red Cross Nagoya First Hospital between April 2012 and December 2017. Four hundred eighty-two patients were identified and included in the study. They included 38 patients (7.9%) requiring re-implantation. Patient demographics are shown in Table 1. The mean age was 65 ± 11 years (range, 20–91 years), with men comprising 52.0%. The mean body mass index (BMI) was 21.7 ± 4.0 (range, 11.0–36.8). TIVAP had been done for long-term chemotherapy (more than 6 months) and/or nutritional supplementation. Most patients (95.2%) had suffered from malignancies including colorectal cancer (56.2%), gastric cancer (8.3%), breast cancer (8.1%), hematologic malignancy (5.8%), hepatobiliary-pancreatic cancer (4.4%), urinary cancer (2.7%), esophageal cancer (2.3%), gynecological cancer (2.3%), head and neck cancer (1.0%), and other malignancies (2.3%). Twenty-three patients (4.8%) had non-malignant diseases including short bowel syndrome, malnutrition due to severe liver disease, and cerebrovascular disease causing dysphagia.
All procedures were performed by surgeons with sufficient experience and were guided by ultrasonography (US) under local anesthesia equipped with mobile X-ray fluoroscopy (Supplementary Figure 1). We used the MicroNeedle Port (Covidien, Tokyo) consisting of a 22 × 28 × 12 mm port and an 8 Fr catheter. Nurses in our inpatient and ambulant chemotherapy departments followed the same procedures. The right IJV was favored to the left IJV, which was frequently selected after the removal of TIVAP via the right IJV. A larger number of TIVAPs were introduced from the right IJV (88.2%) than the left IJV (11.8%). The indications for the TIVAP placement were systemic chemotherapy (81.7%), nutritional supplementation (14.9%), and both (3.3%). There was no patient with TIVAP for neoadjuvant chemotherapy.
In this study, situations requiring TIVAP removal were defined as TIVAP-related complications. All the reasons for TIVAP removal were obtained from the patients’ medical records. Patient follow-up information was compiled through March 2018. The TIVAPs were left for death (n = 227, 47.1%), on used (n = 163, 33.8%) and removed for the end of chemotherapy and/or nutritional supplementation (n = 48, 9.9%) or TIVAP-related complication (n = 44, 9.1%). The TIVAP-related complications were classified as infection (catheter infection and/or septicemia), catheter-related, and port-related complications. The removed catheters were cultured in case of suspected blood stream infection. Catheter infection was confirmed by positive blood cultures, and signs and symptoms of infection such as fever, elevated C-reactive protein, and leukocytosis in the absence of obvious foci other than the TIVAP; or by a positive culture of the removed catheter. The causative microorganisms were identified by blood or catheter culture. Venous thrombosis was confirmed by enhanced computed tomography (CT), magnetic resonance imaging (MRI), or US, although we did not have screening program for deep vein thrombosis. Catheter obstruction was defined as failure to flush the contents via a TIVAP. Catheter disruption and dislocation were identified by plain X-ray radiograph or CT. Fluid leakage from a port or catheter was visually identified in a removed TIVAP.
The risk of TIVAP-related complications was evaluated in terms of patient age, gender, BMI, background diseases, side of insertion, purpose of TIVAP (chemotherapy/nutritional support), and years of TIVAP implantation (2012–2014/2015–2017).
We analyzed types, incidence, and risk factors of late complications associated with TIVAP insertion via the IJV. This study was conducted in accordance with the Helsinki Declaration. The study protocol was approved by the ethics committee of our hospital, which waived the need for informed consent due to the retrospective nature of the study (2018-113).
Statistical analysis
Continuous variables were expressed as mean ± SD or median (IQR) and were compared using the Student t test. The incidence of complications associated with TIVAP was defined in percent and per 1000 catheter days. The Kaplan-Meier analysis was used to estimate the cumulative TIVAP availability rates or complication rates, and the log-rank test was used to analyze differences between groups. Patient death and scheduled port removal without any TIVAP-related complications were categorized as censored cases. Factors with p values of < 0.05 in the univariate analysis were included in a multivariate analysis using a Cox proportional hazards model. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated with the multivariate analysis. Statistical analyses were performed using the JMP version 10.0 for Windows (SAS Institute Inc., Cary, NC, USA) at a significance level of p < 0.05.
Results
The median follow-up duration for the TIVAPs was 319 days (range 1–2016, IQR 152–661), and global follow-up was 218,971 catheter days. The cumulative TIVAP availability rates were 91%, 87%, and 70% at 1, 2, and 3 years, respectively. There were 44 recorded complications (Table 2): an incidence of 9.1% and 0.201 complications/1000 catheter days. Infection, catheter-related, and port-related complications occurred in 21, 14, and 9 patients, respectively. The incidences were 4.4%, 0.096 infections/1000 catheter days; 2.9%, 0.064 catheter-related complications/1000 catheter days; and 1.9%, 0.041 port-related complications/1000 catheter days; respectively.
Twenty-one patients had infectious complications and the causative microorganisms were methicillin-susceptible Staphylococcus aureus (n = 6), methicillin-resistant Staphylococcus aureus (n = 4), methicillin-resistant Staphylococcus epidermidis (n = 4), E. coli (n = 2), and others (n = 5). They included some patients with evident infectious foci such as subcutaneous phlegmon, urinary tract infection, and pneumonia. Fourteen patients had catheter-related complications due to venous thrombosis around the catheter (n = 4) without symptom, catheter obstruction (n = 3), disruption (n = 3), skin ulcer around the catheter (n = 2), and catheter dislocation (n = 2). No case of symptomatic pulmonary embolism attributable to catheter-related thrombosis was recorded. Nine port-related complications were documented: skin ulcer around the port (n = 7), port flip (n = 1), and fluid leakage (n = 1). The cumulative TIVAP-related complication rates according to three complication types are shown in Fig. 1. Infectious complications occurred earlier and more frequently as compared to catheter-related and port-related complications.
The univariate analysis showed that patient age, background diseases, and purpose of the TIVAP were significantly correlated with TIVAP-related complication rates (Table 3, Fig. 2, and Supplementary Figure 2). Subsequent multivariate analysis showed that age < 65 and non-gastrointestinal diseases were significant independent unfavorable risk factors for TIVAP-related complications. Patients with 1 and 2 of these factors had an elevated risk (2.2 and 5.4 times, respectively) of complications.
To analyze the reasons for a relationship between age < 65, non-gastrointestinal diseases, and higher TIVAP-related complication rates, additional analyses were performed (Supplementary Table 1). The mean age of patients with non-gastrointestinal diseases was significantly lower than those with gastrointestinal disease; especially, those of patients with gynecological, hematological, and breast malignancy (54, 56, and 62 years) were less than those with gastrointestinal diseases. The 1-year cumulative TIVAP availability rates were lower in patients with gynecological and hematological malignancy (70% and 86%, respectively) than in those with other diseases. The follow-up durations of patients with age < 65 and ≧ 65 were 447 and 460 days, respectively (p = 0.7401), while the follow-up durations of patients with gastrointestinal diseases and non-gastrointestinal diseases were 496 and 340 days, respectively (p = 0.0003).
Discussion
In this study, the incidence of late complications of TIVAP via the IJV was 9.1% and 0.201 cases per 1000 catheter days. Infectious complications occurred earlier and more frequently as compared to catheter-related and port-related complications. Univariate and multivariate analysis of the risk of developing TIVAP-related complications showed that age < 65 and non-gastrointestinal diseases were significant independent unfavorable factors.
The incidence of TIVAP-related complication of published reports was between 5.4–19.2% and 0.11–0.41 cases per 1000 catheter days depending on definition of complications, age, background diseases, venous access routes, purpose of TIVAP, frequency of TIVAP handling, and study duration [13,14,15,16,17,18,19,20]. The incidence in our study was comparable to the results of previous studies, and relatively lower. The reason for the low incidence in our study can be attributable to safe surgical techniques and standardized management with patient education for chemotherapy and parenteral nutrition in our inpatient and ambulant chemotherapy departments. Results of published data on the late complications of TIVAP via the IJV are summarized in Table 4 [9,10,11,12]. The current study is the second largest with the highest incidence of total complications among five studies probably due to the longer follow-up.
Previous studies have recorded TIVAP-related infection incidences between 1.3 and 30% and between 0.10 and 2.2 cases per 1000 catheter days [3, 21, 22]. Most guidelines recommend 0.3 infections/1000 catheter days as an appropriate upper threshold for the insertion of a subcutaneous venous access device [23]. The incidence recorded in our study (4.4%, 0.096 cases per 1000 catheter days) was relatively low, as compared to previous studies. In the present study, microorganisms identified on blood and/or catheter cultures were Staphylococcus aureus, Staphylococcus epidermidis, and E. coli, which was similar to results from previous studies which identified Staphylococcus epidermidis, Staphylococcus aureus, Enterobacteriaceae, E. coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Candida albicans as the bacteria responsible for the TIVAP-related infections [18, 22, 24, 25]. These organisms can be from the patient’s skin and environment, gastrointestinal tract, and the urinary system. Compared with catheter- and port-related complications, the TIVAP-related infection rate rapidly increased after TIVAP implantation. Intensive sterile technique for surgery, proper management protocol for keeping the TIVAP clean, synbiotics to reduce bacterial translocation [26], and patient education to avert of infections are important. In addition, empiric antibiotic treatment for sensitive microorganisms is recommended when patients with TIVAP have a sign of infectious diseases.
In this study, the incidence of catheter-related complication was 2.9% and 0.064 cases per 1000 catheter days. Specifically, the incidence of venous thrombosis around the catheter was 0.8% and 0.018 cases per 1000 catheter days. The incidence was relatively low compared to the results of previous studies (0–3.2% and 0–0.11 thrombosis per 1000 catheter days) [1, 15, 27], even though specific management excluding a flush after drug administration was not performed in our hospital. Venous thrombosis in 4 cases was diagnosed by a poor fluid drip rate or an incidental computed tomography finding. The relatively low incidence may be due to the small number of patients with palliative nutritional support with TIVAP and patients with hypercoagulopathy due to disseminated malignancies [28]. Catheter disruption and dislocation were found in 3 and 2 patients, respectively. The reasons may be catheter movement along with the patient’s neck or upper arm motion, chronic mechanical stress (e.g., backpack strap), and catheter fatigue. Compared to infection and port-related complication rates, the catheter-related complication rate gradually increased after TIVAP implantation. Wang et al. defined the optimal catheter tip positions to be the distal one-third of the superior vena cava (SVC), the SVC-right atrial junction, and the upper half of the right atrium, and reported that a suboptimal tip position correlated with symptomatic TIVAP occlusion [29]. Scheduled checks for catheter shape and tip location by plain X-ray radiography or CT are important to avoid major events caused by catheter disruption and dislocation.
In this study, the incidence of port-related complications was 1.9%, 0.041 cases per 1000 catheter days. Skin ulcers around the port were common. Proper technique for a sufficient port space, careful handling of the TIVAP, and nutritional support will decrease the complication rate.
The univariate and multivariate analysis of the risk of TIVAP-related complications showed that age < 65 and non-gastrointestinal diseases were significant unfavorable risk factors, although the follow-up durations of patients with gastrointestinal diseases and non-gastrointestinal diseases were significantly different probably due to characteristics of the diseases including disease mortality. Obesity was reported to be a risk factor of TIVAP-related complications [5, 30, 31], and our univariate analysis supported this hypothesis (Table 3). Previous studies reported that risk factors for TIVAP-related infection were hematological malignancy [29, 32,33,34,35], upper gastrointestinal cancer [29], younger age [32, 33], chemotherapy in metastasis [35], hospitalized patients [36], use of parenteral nutrition [37], palliative use [12], and steroid administration [37]. Additionally, risk factors for catheter- and port-related complications were suboptimal position of the TIVAP [29, 38, 39], flushing a port with high pressure [40], inadequate pocket creation for a port, and early administration of bevacizumab after TIVAP implantation [41]. The reasons for increased risk in patients aged < 65 and non-gastrointestinal diseases were indefinite. As the 1 year cumulative TIVAP availability rates and mean age were lower in patients with gynecological, hematological, and breast carcinoma than those of other diseases, we hypothesized that the correlation might be due to disease and treatment specificity. The incidence of gynecological, hematological, and breast malignancy are frequent in younger patients compared with those with other malignancy in Japan [42]. In addition, intensive inpatient chemotherapy is often performed for these malignancies.
We acknowledge that the present study has several limitations. First, despite detailed analysis, it was a retrospective study in a single institute. Unknown background factors relating TIVAP complications may lead to a selection bias. A prospective multicenter study with planned systematic survey is necessary to determine the factors associated with of late complications of a TIVAP via the IJV. Second, the reasons for increased risk in patients with age < 65 and non-gastrointestinal diseases were not fully identified. Further studies investigating several factors including purpose of chemotherapy (adjuvant/metastatic setting), patient’s performance status, nutritional status, length of hospital stay for chemotherapy, and steroid administration are needed. Third, the relationship between patient body motions and catheter movement was not analyzed. This will be necessary to fully understand the causes of catheter disruption and dislocation.
In conclusion, the incidence of late complications of TIVAP via the IJV was acceptable when compared to previous published reports. Infectious complications occurred earlier and more frequently as compared to catheter-related and port-related complications. Age < 65 and non-gastrointestinal diseases were significant independent unfavorable risk factors for TIVAP-related complications. Patients with 1 and 2 of these factors had a 2.2- and 5.4-times higher risk, respectively, of complication compared with those without.
References
Koch HJ, Pietsch M, Krause U et al (1998) Implantable vascular access systems: experience in 1500 patients with totally implanted central venous port systems. World J Surg 22(1):12–16
Vescia S, Baumgärtner AK, Jacobs VR et al (2008) Management of venous port systems in oncology: a review of current evidence. Ann Oncol 19:9–15
Expert Panel on Interventional Radiology, Shaw CM, Shah S, Kapoor BS et al (2017) ACR Appropriateness Criteria® Radiologic Management of Central Venous Access. J Am Coll Radiol 14(11S):S506–S529
Kurul S, Saip P, Aydin T (2002) Totally implantable venous-access ports: local problems and extravasation injury. Lancet Oncol 3:684–692
Lefebvre L, Noyon E, Georgescu D et al (2016) Port catheter versus peripherally inserted central catheter for postoperative chemotherapy in early breast cancer: a retrospective analysis of 448 patients. Support Care Cancer 24(3):1397–1403
Matsushima H, Adachi T, Iwata T, Hamada T, Moriuchi H, Yamashita M, Kitajima T, Okubo H, Eguchi S (2017) Analysis of the outcomes in central venous access port implantation performed by residents via the internal jugular vein and subclavian vein. J Surg Educ 74(3):443–449
Teichgräber UK, Kausche S, Nagel SN, Gebauer B (2011) Outcome analysis in 3,160 implantations of radiologically guided placements of totally implantable central venous port systems. Eur Radiol 21(6):1224–1232
Kim JT, Oh TY, Chang WH, Jeong YK (2012) Clinical review and analysis of complications of totally implantable venous access devices for chemotherapy. Med Oncol 29(2):1361–1364
Yip D, Funaki B (2002) Subcutaneous chest ports via the internal jugular vein. A retrospective study of 117 oncology patients. Acta Radiol 43(4):371–375
Charvát J, Linke Z, Horáèková M, Prausová J (2006) Implantation of central venous ports with catheter insertion via the right internal jugular vein in oncology patients: single center experience. Support Care Cancer 14(11):1162–1165
Zhou J, Qian S, He W et al (2014) Implanting totally implantable venous access port via the internal jugular vein guided by ultrasonography is feasible and safe in patients with breast cancer. World J Surg Oncol 12:378
Nagasawa Y, Shimizu T, Sonoda H, Mekata E, Wakabayashi M, Ohta H, Murata S, Mori T, Naka S, Tani T (2014) A comparison of outcomes and complications of totally implantable access port through the internal jugular in versus the subclavian vein. Int Surg 99(2):182–188
Gebauer B, El-Sheik M, Vogt M et al (2009) Combined ultrasound and fluoroscopy guided port catheter implantation—high success and low complication rate. Eur J Radiol 69(3):517–522
Torramade JR, Cienfuegos JA, Hernández JL et al (1993) The complications of central venous access systems: a study of 218 patients. Eur J Surg 159(6-7):323–327
Biffi R, de Braud F, Orsi F et al (1998) Totally implantable central venous access ports for long-term chemotherapy. A prospective study analyzing complications and costs of 333 devices with a minimum follow-up of 180 days. Ann Oncol 9(7):767–773
Takehara K, Tanakaya K, Morihiro T et al (2011) Analysis of infecting organism and risk factors for infections related to totally implantable central venous access devices. J Jpn Soc Surg Infect 8(6):699–703 (in Japanese with English abstract)
Fagnani D, Bertolini A, Catena L, Tomirotti M, Visini M, Alatri A, de Paoli A, Aondio GM, Milani M, Arpaia G, Cimminiello C, POLONORD Group, Franchi R, Porta C, Pugliese P, Borgonovo K, Duro M, Ardizzoia A, Filipazzi V, Isa L, Vergani C, Carpenedo M, Viale P (2009) The impact of antithrombotic prophylaxis on infectious complications in cancer patients with central venous catheters: an observational study. Blood Coagul Fibrinolysis 20(1):35–40
Chang L, Tsai JS, Huang SJ, Shih CC (2003) Evaluation of infectious complications of the implantable venous access system in a general oncologic population. Am J Infect Control 31(1):34–39
Yamaguchi K, Ogata Y, Gotanda U et al (2011) The durability of subcutaneously implantable central venous catheter ports in cancer patients––the relation between parenteral nutrition and catheter related blood stream infection. J Surg Metab Nutr 45(6):185–190 (in Japanese with English abstract)
Bassi KK, Giri AK, Pattanayak M, Abraham SW, Pandey KK (2012) Totally implantable venous access ports: retrospective review of long-term complications in 81 patients. Indian J Cancer 49:114–118
Biffi R, Pozzi S, Agazzi A, Pace U, Floridi A, Cenciarelli S, Peveri V, Cocquio A, Andreoni B, Martinelli G (2004) Use of totally implantable central venous access ports for high-dose chemotherapy and peripheral blood stem cell transplantation: results of a monocentre series of 376 patients. Ann Oncol 15(2):296–300
Lebeaux D, Larroque B, Gellen-Dautremer J, Leflon-Guibout V, Dreyer C, Bialek S, Froissart A, Hentic O, Tessier C, Ruimy R, Pelletier AL, Crestani B, Fournier M, Papo T, Barry B, Zarrouk V, Fantin B (2012) Clinical outcome after a totally implantable venous access port-related infection in cancer patients: a prospective study and review of the literature. Medicine (Baltimore) 91(6):309–318
Walser EM (2012) Venous access ports: indications, implantation technique, follow-up, and complications. Cardiovasc Intervent Radiol 35(4):751–764
Adler A, Yaniv I, Steinberg R et al (2006) Infectious complications of implantable ports and Hickman catheters in paediatric haematology-oncology patients. J Hosp Infect 62(3):358–365
Vidal M, Genillon JP, Forestier E et al (2016) Outcome of totally implantable venous-access port-related infections. Med Mal Infect 46(1):32–38
Manzanares W, Hardy G (2008) The role of prebiotics and synbiotics in critically ill patients. Curr Opin Clin Nutr Metab Care 11(6):782–789
Mori Y, Nagayama S, Kawamura J, Hasegawa S, Tanaka E, Okabe H, Takeuchi M, Sonobe M, Matsumoto S, Kanai M, Muto M, Chiba T, Sakai Y (2016) A retrospective analysis on the utility and complications of upper arm ports in 433 cases at a single institute. Int J Clin Oncol 21(3):474–482
Ikushima S, Ono R, Fukuda K, Sakayori M, Awano N, Kondo K (2016) Trousseau’s syndrome: cancer-associated thrombosis. Jpn J Clin Oncol 46(3):204–208
Wang YC, Lin PL, Chou WH et al (2017) Long-term outcomes of totally implantable venous access devices. Support Care Cancer 25(7):2049–2054
Ignatov A, Hoffman O, Smith B, Fahlke J, Peters B, Bischoff J, Costa SD (2009) An 11-year retrospective study of totally implanted central venous access ports: complications and patient satisfaction. Eur J Surg Oncol 35(3):241–246
Wyschkon S, Löschmann JP, Scheurig-Münkler C, Nagel S, Hamm B, Elgeti T (2016) Apparent migration of implantable port devices: normal variations in consideration of BMI. J Vasc Access 17(2):155–161
Ji L, Yang J, Miao J et al (2015) Infections related to totally implantable venous-access ports: long-term experience in one center. Cell Biochem Biophys 72(1):235–240
Samaras P, Dold S, Braun J, Kestenholz P, Breitenstein S, Imhof A, Renner C, Stenner-Liewen F, Pestalozzi BC (2008) Infectious port complications are more frequent in younger patients with hematologic malignancies than in solid tumor patients. Oncology. 74(3-4):237–244
Kim HJ, Yun J, Kim HJ et al (2010) Safety and effectiveness of central venous catheterization in patients with cancer: prospective observational study. J Korean Med Sci 25(12):1748–1753
Wang TY, Lee KD, Chen PT, Chen MC, Chen YY, Huang CE, Kuan FC, Chen CC, Lu CH (2015) Incidence and risk factors for central venous access port-related infection in Chinese cancer patients. J Formos Med Assoc 114(11):1055–1060
Pandey N, Chittams JL, Trerotola SO (2013) Outpatient placement of subcutaneous venous access ports reduces the rate of infection and dehiscence compared with inpatient placement. J Vasc Interv Radiol 24(6):849–854
Okada S, Shiraishi A, Yamashiro Y, Inoue T, Tsuge D, Aida M, Kuwatsuru R (2015) A retrospective statistical analysis of the late complications associated with central venous port placements. Jpn J Radiol 33(1):21–25
Caers J, Fontaine C, Vinh-Hung V, de Mey J, Ponnet G, Oost C, Lamote J, de Greve J, van Camp B, Lacor P (2005) Catheter tip position as a risk factor for thrombosis associated with the use of subcutaneous infusion ports. Support Care Cancer 13(5):325–331
Wu CY, Hu HC, Ko PJ, Fu JY, Wu CF, Liu YH, Li HJ, Kao TC, Kao KC, Yu SY, Chang CJ, Hsieh HC (2012) Risk factors and possible mechanisms of superior vena cava intravenous port malfunction. Ann Surg 255(5):971–975
Xiao SP, Xiong B, Chu J et al (2015) Fracture and migration of implantable venous access port catheters: cause analysis and management of 4 cases. J Huazhong Univ Sci Technolog Med Sci 35(5):763–765
Zawacki WJ, Walker TG, DeVasher E et al (2009) Wound dehiscence or failure to heal following venous access port placement in patients receiving bevacizumab therapy. Vasc Interv Radiol 20(5):624–627
National Cancer Center Research Institute. Recent Cancer Statistics. https://ganjoho.jp/reg_stat/statistics/stat/summary.html
Funding
This work is supported by Japanese Red Cross Nagoya First Hospital Research Grant. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsuruta, S., Goto, Y., Miyake, H. et al. Late complications associated with totally implantable venous access port implantation via the internal jugular vein. Support Care Cancer 28, 2761–2768 (2020). https://doi.org/10.1007/s00520-019-05122-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05122-3