Abstract
Background
Totally implantable venous access ports (TIVAP) have been widely used in cancer patients for many years. The early infection (within 30 days after TIVAP implantation) rate of TIVAP accounts for about one-third of all TIVAP infections, and early infection often causes port removal and affects subsequent cancer treatment. This study investigated the incidence and risk factors for early and late infection after TIVAP implantation.
Methods
From January 2013 to December 2018, all adult cancer patients who received TIVAP implantation in Taipei Medical University Shuang-Ho Hospital were reviewed. We evaluated the incidence of TIVAP-related infection, patient characteristics, and bacteriologic data. Univariable analysis and multiple logistic regression analysis were used to evaluate the risk factors of TIVAP-related infection.
Results
A total of 3001 TIVAPs were implanted in 2897 patients, and the median follow-up time was 424 days (range: 1–2492 days), achieving a combined total of 1,648,731 catheter days. Thirty-one patients (1.0%) had early infection and 167 (5.6%) patients had late infection. In multivariate analysis, TIVAP combined with other surgeries (p = 0.03) and inpatient setting (p < 0.001) was the risk factor of early infection, and TIVAP combined with other surgeries (p = 0.007), hematological cancer (p = 0.03), and inpatient setting (p < 0.001) was the risk factor of late infection.
Conclusion
Inpatient TIVAP implantation and TIVAP implantation combined with other surgeries are associated with high rates of TIVAP-related early and late infections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Totally implantable venous access port (TIVAP) was first reported by Niederhuber et al. in 1982 [1]. This device is convenient for chemotherapy administration for cancer patients and intravenous nutrition for patients who need total parenteral nutrition. The most complication in patients with TIVAP is TIVAP-related infection. The incidence of TIVAP-related infection is between 5.6 and 13%, with an infection rate ranging from 0.15 to 0.39/1000 catheter days in oncological patients [2, 3]. The port often needs to be removed after TIVAP-related infection has been diagnosed, thus affecting the subsequent chemotherapy. Moreover, approximately 46–54% patient mortality occurs within 3 months after TIVAP-related infection [3, 4].
TIVAP-related infections are divided into early and late infections depending on the time of infection occurrence. Early infection is defined as the port-related infection that occurs within 30 days after TIVAP implantation [5, 6]; it is also regarded as a surgical-related infection because infection occurs shortly after the operation. Early TIVAP-related infections usually prolong hospital stay and increase estimated hospital costs [7]. Previous studies showed that the incidence of early infection reaches 0.3–4.5% and accounts for 18–38% of all port-related infections [2, 5, 8, 9]. However, the risk factors associated with early infection and operation were not comprehensively analyzed, and the sample sizes in previous studies were small. We conducted this retrospective study to investigate and analyze the incidence and risk factors of early infection and also compared the results with those of late infection to determine the difference between the two kinds of infection.
Materials and methods
Patient population and follow-up
From January 2013 to December 2018, 3041 consecutive TIVAP implantations were performed in Taipei Medical University Shuang-Ho Hospital. The exclusion criteria included patients who underwent TIVAP implantation for total intravenous nutrition and patient younger than 20 years old. The patients’ basic and perioperative characteristics were reviewed from medical charts. This study was approved by the Taipei Medical University Institutional Review Board/Ethics Committee (approval number: N201801072). This research is a retrospective study, and thus, informed consent was not required for this study.
All TIVAP implantation procedures were performed in an operation room under local or general anesthesia. The right side or left side of catheter insertion and procedures, including cut-down and puncture methods, were selected mandatorily if a disease occurs on one side. But if no problems in both side, the dominant arm has to be considered the choice, and the opposite has to be chosen. Catheter insertion into the cephalic and external jugular veins by vessel dissection via an open wound was defined as “cut-down” method, and the procedure in which the catheter was inserted into the internal jugular, subclavian, and femoral veins by Seldinger procedure was defined as “puncture” method. After leaving the operation room, the position of the distal tip of the catheter was confirmed by chest roentgenography. The procedure of TIVAP implantation that was completed by the attending surgeon alone was defined by the operator as “attending surgeon” and that which was completed by residents assisted by the attending surgeon or resident alone was defined by the operator as “resident.”
The catheter lifespan or measurement of catheter day started from the TIVAP implantation until the death of patient; TIVAP removal; last follow-up; or October 31, 2019, whichever came first.
Identification of port-related infection
We retrospectively evaluated the TIVAP-related infections and bacteriologic data from medical records. TIVAP-related infections were divided into early and late infection. Early infection means that the infection signs or symptoms occurred within 30 days after TIVAP implantation, whereas late infection denotes that infection occurred more than 30 days after TIVAP implantation. A TIVAP-related infection was defined as a confirmed infection when the following criteria were observed:
-
1.
Local infection: port-pocket infection or catheter tunnel infection;
-
2.
Clinical sign of infection (fever, chills, and/or hypotension) with a positive culture of the catheter tip and/or the reservoir port;
-
3.
Clinical sign of infection with at least two positive cultures from peripheral vein with infection improvement after TIVAP removal;
-
4.
No bacterial documentation but infection improvement after TIVAP removal.
Statistical analysis
Data were analyzed using the Statistical Product and Service Solutions (SPSS) package (SPSS 13.0 for Macintosh; SPSS Inc., Chicago, USA). Data were presented as mean ± standard deviation. Comparisons were made using the χ2 test or one way analysis of variance for continuous or categorical variables, respectively. Simple logistic regression (univariate analysis) and multiple logistic regression (multivariate analysis) were performed to identify the risk factors for infection. A p value < 0.05 was considered statistically significant.
Results
Patient population
A total of 3041 consecutive TIVAP implantation procedures were reviewed. Ten patients experienced procedure failure of TIVAP implantation. Among these patients, two patients suffered from complications of pneumothorax, and the other eight patients experienced vessel variation. Seven patients with TIVAP implantation needed total parenteral nutrition, and 23 patients were lost to follow-up after TIVAP implantation. After excluding these patients, 3001 TIVAPs in 2897 patients were analyzed in this study (Fig. 1). Among the 2897 patients, 98 underwent TIVAP implantation twice, and 3 underwent TIVAP implantation thrice. In the 3001 TIVAPs, the median age at which patient received TIVAP implantation was 63 years (range: 20–99 years). The median follow-up time was 424 days (range: 1–2492 days) with a total of 1,648,731 catheter days.
Early and late complications
Sixty-eight (2.3%) TIVAPs had complications within 30 days after port implantation. The catheter tip malposition occurred in 62 patients within 30 days after TIVAP implantation, of whom 54 underwent port revision, and 8 needed port removal. Four patients had pneumothorax with TIVAP procedure completion, and all patients underwent subsequent chest tube or pigtail insertion due to complications. One patient had catheter occlusion and the other one patient had wound bleeding with subcutaneous hematoma and needed port revision. For late complications, 7 patients had catheter tip malposition. Among these patients, 2 patients needed port removal, and 5 patients needed port revision. Catheter occlusion occurred in 33 patients. A total of 26 and 7 patients needed port removal and port revision, respectively. Other complications included venous thrombosis (19 patients), broken catheter (9 patients), catheter kinking (2 patients), and skin necrosis (2 patients) (Table 1).
Analysis of infection incidence and risk factors
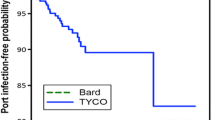
A total of 198 (6.6%) patients had TIVAP-related infection, with the incidence reaching 0.12/1000 catheter day. Among these patients, 31 (15.7%) patients had early infection, and 167 (84.3%) patients had late infection. In early-infection patients, the median time from TIVAP implantation to symptom onset was 17 days (range: 4–30 days). Two patients experienced port-pocket infection, and the remaining patients suffered from blood stream infection. Table 2 shows the infection rates and incidence in the subgroups based on the risk factors of all TIVAP-related infections. Patients with hematologic disease (p < 0.01), inpatient TIVAP implantation (p < 0.01), cut-down method (p = 0.02), TIVAP combined with other surgeries (p < 0.01), and male patients (p < 0.01) had high incidence of all TIVAP-related infection.
For early infection, the incidence of infection is high in TIVAP combined with other surgeries (p < 0.01) and inpatient TIVAP implantation (p < 0.01), as shown by the univariate analysis. In the multivariate analysis, only TIVAP combined with other surgeries (p < 0.01) and inpatient TIVAP implantation (p = 0.03) presented as risk factors for early infection (Table 3).
In late infection, the incidence of infection was higher in male patients (p < 0.01), hematologic disease (p < 0.01), inpatient TIVAP implantation (p < 0.01), TIVAP implantation by cut-down method (p = 0.046), and TIVAP combined with other surgeries (p < 0.01), as indicated by the univariate analysis. In the multivariate analysis, hematologic disease (p = 0.03), inpatient TIVAP implantation (p < 0.01), and TIVAP combined with other surgeries were the risk factors for late infection (Table 3).
A total of 94 TIVAP implantations were combined with other surgery, and the analysis of combined surgeries are listed in Table 4. Six patients had early infection, and the infection only occurred in patient with TIVAP implantations combined with gastrostomy (n = 2) and feeding jejunostomy (n = 4). Thirteen patients had late infections, and the infections occurred in patient with TIVAP implantations combined with gastrostomy (n = 5), feeding jejunostomy (n = 6), breast surgery (n = 1) and cystoscopy (n = 1).
Microbiological data
In early infections, microorganisms were isolated from 22 (71%) patients, and no microorganism was isolated in the other 9 (29%) early-infection cases. Twenty infections were monomicrobial, and two were polymicrobial. The most common isolated microorganism was Staphylococcus aureus (n = 8). In late infections, microorganism were isolated in 129 (77%) patients and no microorganism was noted in the other 38 (23%) patients. The most common three isolated microorganisms were Acinetobacter spp. (n = 23), yeast-like organism (n = 22), and Staphylococcus aureus. (n = 20) (Table 5).
Discussion
The present research is a large-scale retrospective study that analyzed the risk factors and incidence of early and late TIVAP-related infections. This study presented that inpatient TIVAP implantation and TIVAP implantation combined with other surgeries are risk factors for early infection, whereas inpatient TIVAP implantation, patient with hematologic disease, and TIVAP implantation combined with other surgeries are risk factors for late infection.
Table 6 showed the TIVAP-related early infection and its risk factors in previous studies. Inpatient TIVAP implantation is one of the risk factors that have been mentioned frequently in such studies. Inpatient TIVAP implantation increases the risk of early TIVAP infection because frequent access to ports during inpatient admission and periprocedural nosocomial environment causes increased risk of infection [10]. In addition, the port wound is accessed prematurely when the port is implanted during hospitalization, and chemotherapeutic agents will reduce angiogenesis and lead to wound dehiscence, which easily causes early infection [11]. Other factors, such as low white blood cell count and platelet cell count and hypoalbuminemia, are reported as the risk factors of early infection [5, 12, 13]. However, these risk factors are related to a patient’s own baseline nutrition, immunity, or general condition. As for the factors related to surgery, such as surgical method, the blood vessel used, and operative time, limited studies have analyzed the risk factors of early infection.
In addition to inpatient TIVAP implantation, we found that TIVAP implantation combined with other surgeries is also a risk factor of early and late infection. In general, TIVAP implantation is a simple and clean wound procedure, but cancer patients often need to receive TIVAP implantation combined with other surgery at the same time. Therefore, the operation time will be increased, and the number of bacterial colonies in the air will also increase significantly after opening the gastrointestinal tract [14, 15] if a combined gastrointestinal surgery is to be performed. Under this situation, TIVAP will be exposed to an environment that is susceptible to infection. In the present study, out of 94 patients with other combined surgeries, 19 had TIVAP-related infection (20.2%) compared with 6.2% of patients without combined surgery (Table 2). In early infection four out of the six patients received feeding jejunostomy, and the other two patients received gastrostomy (Table 4). In late infection, eleven out the thirteen patients received feeding jejunostomy or gastrostomy, the other two patients received cystoscopy and breast surgery. For this reason, we recommend that TIVAP implantation should not be performed in combination with other surgeries at the same time, especially gastrointestinal surgery.
Hematologic disease is considered to have great relevance for affecting TIVAP-related infection. Patients with hematologic disease usually have low blood cell count, receive strong chemotherapeutic agents, and need multiple blood product transfusion through the port. Therefore, patients with hematologic disease have higher risk of TIVAP-related infection than those with solid cancer as shown in previous studies [7, 16, 17]. The present study revealed that hematologic disease is not a risk factor of early infection but a risk factor for late infection. This explains that the most likely, route of early infection is the entry of bacteria from the surgical wound and early infection is not related to patient’s poor general condition caused by hematologic disease.
Attending surgeons are generally believed to possess rich experience in surgery and cause less complications, such as infection, than residents [18, 19]. TIVAP implantation is usually one of the first procedures that a surgical resident learns. Schreckenbach et al. reviewed 760 TIVAP implantations and found resident performing alone or resident performing with help could increase TIVAP-related early infection [20]. In our study, the early-infection risk showed no significant difference between TIVAP implantation performed by attending surgeons and residents. In addition, operation time featured a positive correlation with the risk of infection [21, 22]. This result occurs mainly because prolonged wound exposure to air will increase bacterial contact with the wound, and the infection risk will increase under long operative time. Although a long operative time has a high tendency to cause early infection, our study showed that operation time is not a risk factor of TIVAP early infection.
Cephalic vein or external jugular vein cut-down and subclavian or internal jugular vein puncture by Seldinger procedure are two main methods for TIVAP implantation. Nocito et al. have reported that venous puncture by Seldinger procedure is quicker and more effective than venous cut-down procedure [23]. However, the early infection rate showed no difference between the two surgical methods in a large-series retrospective study [5] and a randomized control research [24]; the early-infection rate also revealed no significant difference between the two surgical methods used in this study.
Staphylococcus aureus are the most commonly isolated organism from the patients with early infections; however, the most three isolated organisms are Acinetobacter spp., yeast, and Staphylococcus aureus. Gram-positive cocci including coagulase negative Staphylococcus and Staphylococcus aureus are known to colonize in the skin, so bacteria is mainly contaminated from the surgical wound in early infections. In late infections, the catheter infections are related to bacteremia caused by immunocompromised patients or port contaminated by skin flora via frequent skin puncture. For these infections, the port should be removed, and long-term antibiotics should be given based on culture sensitivity results [25]. If a patient presents with fever and a negative culture study, the decision for removing the port device presents difficulty. However, in our study, eight patients in early infection exhibited fever with negative results of microbiological studies, and they experienced symptom relief after TIVAP removal and empirical antibiotic administration.
The main limitation of this study is its retrospective nature. All data were documented from medical records, and bias is inevitable. Second, the incidence of infection rate could have been underestimated if the clinically undetected catheter-related bloodstream infection, the rapidly progressing catheter-related fatal bloodstream infection, or medically treated infections were eliminated successfully without port removal. Third, the effect of multicollinearity should also be considered in this study. Most of the TIVAP combined with other operations are hospitalization (92 out of 94 patients), and this effect will make some bias in the results of this study. In addition, all TIVAP implantations were performed by 17 attending surgeons in our institute, and the surgeon’s preference and patient characteristics presented considerable difference. All these biases may affect the observational results.
In conclusion, inpatient TIVAP implantation and TIVAP implantation combined with other surgeries are risk factors for TIVAP related in both early and late infections. For this reason, we recommend that TIVAP implantation be performed in an outpatient setting rather than in a hospitalization status and TIVAP implantation without other surgery combination could reduce the TIVAP-related early infection.
Data availability
The data that support the findings of this study are available from the corresponding author, Tung-Cheng Chang, upon reasonable request.
References
Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, Cozzi E (1982) Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery 92:706–712
Zerati AE, Figueredo TR, de Moraes RD, da Cruz AM, da Motta-Leal Filho JM, Freire MP et al (2016) Risk factors for infectious and noninfectious complications of totally implantable venous catheters in cancer patients. J Vasc Surg Venous Lymphat Disord 4:200–205
Lebeaux D, Larroque B, Gellen-Dautremer J, Leflon-Guibout V, Dreyer C, Bialek S et al (2012) Clinical outcome after a totally implantable venous access port-related infection in cancer patients: a prospective study and review of the literature. Medicine 9:309–318
Vidal M, Genillon JP, Forestier E, Trouiller S, Pereira B, Mrozek N et al (2016) Outcome of totally implantable venous-access port-related infections. Med Mal Infect 46:32–38
Tang L, Kim CY, Martin JG, Pabon-Ramos WM, Sag AA, Suhocki PV et al (2020) Length of stay predicts risk of early infection for hospitalized patients undergoing central venous port placement. J Vasc Interv Radiol 31:454–461
Voog E, Campion L, du Rusquec P, Bourgeois H, Domont J, Denis F et al (2018) Totally implantable venous access ports: a prospective long-term study of early and late complications in adult patients with cancer. Support Care Cancer 26:81–89
Penel N, Neu JC, Clisant S, Hoppe H, Devos P, Yazdanpanah Y (2007) Risk factors for early catheter-related infections in cancer patients. Cancer 110:1586–1592
Shim J, Seo TS, Song MG, Cha IH, Kim JS, Choi CW et al (2014) Incidence and risk factors of infectious complications related to implantable venous-access ports. Korean J Radiol 15:494–500
Heibl C, Trommet V, Burgstaller S, Mayrbaeurl B, Baldinger C, Koplmüller R et al (2010) Complications associated with the use of Port-a-Caths in patients with malignant or haematological disease: a single-centre prospective analysis. Eur J Cancer Care 19:676–681
Pandey N, Chittams JL, Trerotola SO (2013) Outpatient placement of subcutaneous venous access ports reduces the rate of infection and dehiscence compared with inpatient placement. J Vasc Interv Radiol 24:849–854
Erinjeri JP, Fong AJ, Kemeny NE, Brown KT, Getrajdman GI, Solomon SB (2011) Timing of administration of bevacizumab chemotherapy affects wound healing after chest wall port placement. Cancer 117:1296–1301
Bamba R, Lorenz JM, Lale AJ, Funaki BS, Zangan SM (2014) Clinical predictors of port infections within the first 30 days of placement. J Vasc Interv Radiol 25:419–423
Zhang S, Kobayashi K, Faridnia M, Skummer P, Zhang D, Karmel MI (2018) Clinical predictors of port infections in adult patients with hematologic malignancies. J Vasc Interv Radiol 29:1148–1155
Stone AM, Tucci VJ, Isenberg HD, Wise L (1976) Wound infection: a prospective study of 7519 operations. Am Surg 42:849–852
Drake CT, Goldman E, Nichols RL, Piatriszka K, Nyhus LM (1977) Environmental air and airborne infections. Ann Surg 185:219–223
Hsieh CC, Weng HH, Huang WS, Wang WK, Kao CL, Lu MS et al (2009) Analysis of risk factors for central venous port failure in cancer patients. World J Gastroenterol 15:4709–4714
Crisinel M, Mahy S, Ortega-Debalon P, Buisson M, Favre JP, Chavanet P et al (2009) Incidence, prevalence and risk factors for a first infectious complication on a totally implantable venous-access port. Med Mal Infect 39:252–258
Doyon L, Moreno-Koehler A, Ricciardi R, Nepomnayshy D (2016) Resident participation in laparoscopic Roux-en-Y gastric bypass: a comparison of outcomes from the ACS-NSQIP database. Surg Endosc 30:3216–3224
Relles DM, Burkhart RA, Pucci MJ, Sendecki J, Tholey R, Drueding R et al (2014) Does resident experience affect outcomes in complex abdominal surgery? Pancreaticoduodenectomy as an example. J Gastrointest Surg 18:279–285
Schreckenbach T, Münch I, El Youzouri H, Bechstein WO, Habbe N (2019) The safety level of total central venous access port implantation performed by residents. J Surg Educ 76:182–192
Wang T, Wang H, Yang DL, Jiang LQ, Zhang LJ, Ding WY (2017) Factors predicting surgical site infection after posterior lumbar surgery: a multicenter retrospective study. Medicine (Baltimore) 96:e6042
Karim H, Chafik K, Karim K, Moez H, Makki AM, Adnen el-H et al (2000) Risk factors for surgical wound infection in digestive surgery. Retrospective study of 3,000 surgical wounds. Tunis Med 78:634–640
Nocito A, Wildi S, Rufibach K, Clavien PA, Weber M (2009) Randomized clinical trial comparing venous cutdown with the Seldinger technique for placement of implantable venous access ports. Br J Surg 96:1129–1134
Hüttner FJ, Bruckner T, Hackbusch M, Weitz J, Bork U, Kotschenreuther P et al (2020) Primary open versus closed implantation strategy for totally implantable venous access ports: the multicentre randomized controlled PORTAS-3 Trial (DRKS 00004900). Ann Surg. https://doi.org/10.1097/SLA.0000000000003705
Lebeaux D, Fernández-Hidalgo N, Chauhan A, Lee S, Ghigo JM, Almirante B et al (2014) Management of infections related to totally implantable venous-access ports: challenges and perspectives. Lancet Infect Dis 14:146–159
Author information
Authors and Affiliations
Contributions
Conception and design: Min-Hsuan Yen and Tung-Cheng Chang. Acquisition of data: Min-Hsuan Yen and Tung-Cheng Chang. Analysis and interpretation data: Min-Hsuan Yen, Kee-Thai Kiu and Tung-Cheng Chang. Writing, review, and revision of the manuscript: Tung-Cheng Chang.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the ethics committee of the Taipei Medical University (approval number: N201801072) and performed according to the declaration of Helsinki of 1964 and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not applicable due to the retrospective nature of this study.
Conflict of interest
The authors declare no competing of interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chang, TC., Yen, MH. & Kiu, KT. Incidence and risk factor for infection of totally implantable venous access port. Langenbecks Arch Surg 407, 343–351 (2022). https://doi.org/10.1007/s00423-021-02328-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02328-0