Abstract
Objectives
To provide an overview of costs associated with the treatment of breast cancer-related lymphoedema (BCRL) and its possible sequelae, borne by patients or by society.
Data sources
According to the PRISMA guideline, a systematic literature search was carried out in four electronic databases: PubMed, Web of Science, Cochrane Clinical Trials and EMBASE. Searches were performed on October 1, 2018.
Study selection
Eligibility criteria: (1) expenses of adults (age > 18 years), (2) concerning patients with BCRL, (3) overview of (in)direct costs associated with BCRL, (4) expenses in which at least one type of conservative treatment modality for lymphoedema is included and/or costs for hospital admissions due to infections. Reviews and meta-analyses were excluded.
Data extraction
After assessing the risk of bias and level of evidence, quantitative data on (in)direct costs for BCRL treatment during a well-mentioned timeframe were extracted.
Data synthesis
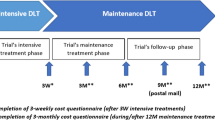
Eight studies were included. Three studies reported on patient-borne costs related to BCRL. Mean direct costs per year borne by patients ranged between USD$2306 and USD$2574. Indirect costs borne by patients ranged between USD$3325 and USD$5545 per year. Five studies estimated society-borne costs related to BCRL from claims data, billing prices and providers’ services during 12 to 24 months of follow-up. Mean direct treatment costs after 1 year of decongestive lymphatic therapy (DLT) ranged between €799 (= USD$1126.60) and USD$3165.
Conclusion
This systematic review revealed that BCRL imposes a substantial economic burden on patients and society. However, more standardized high-quality health economic analyses among this field are required. Recent economic analyses related to BCRL treatment in Europe, Asia, Africa and South America are lacking. Worldwide, further scrutiny of the economic impact of DLT for BCRL in clinical settings is needed.
Clinical trial registration number
The review makes part of a double-blind, multi-center, randomized controlled trial (EFforT-BCRL trial), which is registered in clinicaltrials.gov (NCT02609724). CME reference S58689, EudraCT Number 2015-004822-33.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Worldwide, breast cancer is the most common cancer in women [1]. Although breast cancer-related lymphoedema (BCRL) is not the most prevalent complication after treatment for breast cancer [2], it is internationally recognized as one of the most dreaded morbidities. Since the introduction of more effective treatment modalities [3,4,5,6] increases the number of breast cancer survivors, the amount of patients dealing with long-term side effects, such as lymphoedema, rises likewise [7]. BCRL is caused by a decreased lymphatic transport capacity and/or increased lymphatic load after which fluid accumulates in the extracellular spaces of soft tissues, resulting in swelling [8]. Today, pooled data reveals a BCRL incidence rate of 16.6% [9].
Besides an impact on functional and psychosocial well-being [10], there can be an additional deleterious effect of lymphoedema on patients in terms of financial costs [11, 12]. Daily living can be affected by copayments for the increase in medical and therapeutic consultations, as well as by other direct costs for compression garments and other (in)direct therapy-related expenses [11]. Moreover, financial burdensome can be emphasized through the impact of (advanced) lymphoedema on career and employment [12]. This happens for instance when a transition from fulltime to part-time employment is required in order to spend more time on complex care [12]. Besides the lymphoedema which requires appropriate treatment, complications secondary to BCRL, such as repeated infections, may arise as well [13]. These episodes need early antibiotic therapy and may require hospitalization, increasing the costs of care even more [14].
According to the recommendations of the International Society of Lymphology (ISL), BCRL needs to be treated with decongestive lymphatic therapy (DLT) [15]. This is a two-stage treatment program, consisting of different conservative treatment modalities. During the first or intensive phase, lymphoedema is maximally reduced. This phase consists of skin care, manual lymph drainage (MLD), multi-layer bandaging and exercise therapy. The second or maintenance phase aims to conserve and optimize the results obtained in the first phase. It consists of skin care, compression by a low-stretch compression sleeve, exercises and MLD [16]. Although DLT is recognized as the gold standard for conservative treatment of lymphoedema [15, 17], reimbursement for DLT has been hampered by a lack of rigorous research evidence [8]. Additionally, current literature on the financial burden of BCRL treatment is extremely limited. An overview between patient-borne and society-borne costs within this financial burden is missing. However, this is essential to estimate the actual economic impact of BCRL for patients as for society.
Therefore, the aim of this review was to make an overview of the currently available literature on direct and indirect patient-borne as well as society-borne costs associated with the treatment of BCRL and its sequelae.
Methods
Literature search and inclusion criteria
According to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [18] (www.prisma-statement.org), a systematic review of the literature was performed. This review has been registered on PROSPERO (https://www.crd.york.ac.uk/PROSPERO) with registration number CRD42018114649. In order to identify eligible studies, four electronic databases were screened on October 1, 2018: PubMed, Web of Science, EMBASE and Cochrane Clinical Trials. A PICOS search strategy was built up, resulting in a Boolean search where following indexing terms (i.e. MeSH for Pubmed and Cochrane, Emtree for EMBASE) and keywords were combined: ‘breast cancer(P)’, ‘lymphoedema(P)’, ‘decongestive lymphatic therapy(I)’, ‘treatment(I)’, ‘economic analysis(O)’, ‘economic evaluation(O)’ and ‘costs(O)’. A comparison was not defined (not applicable). Equivalent searches were executed in all four databases, although modifications in keywords were included due to differences in usage of indexing terms. When using Web of Science, an additional restriction was added to the search with the filter ‘document type: Article’, and in EMBASE, the search was limited to ‘Articles’ or ‘Articles in press’ and studies based on ‘Humans’. In Appendix, an overview of the applied search strategies for the different databases is presented.
The screening for eligible articles was twofold and performed by two raters (T.D.V. and N.G.). The first screening upon title and abstract was achieved for all references in each database, in order to assess which articles were relevant for further scrutiny. Thereafter, a second screening on the full texts of the selected articles was performed. Both screenings were based upon predetermined inclusion and exclusion criteria, reported in Table 1. In case of disagreement between the reviewers regarding the in- or exclusion of studies, consensus was reached during a meeting.
Methodological quality assessment and data extraction
To assess the methodological quality of the selected full texts, the 19-item NICE checklist for (partial) economic evaluations provided by the National Institute for Health and Care Excellence (NICE) [19] (https://www.nice.org.uk/process/pmg20/chapter/incorporating-economic-evaluation) was used. Full texts were evaluated by both reviewers (T.D.V. and N.G.). As the NICE checklist initially is designed for the UK, some minor adjustments in questions were necessary to generalize the feasibility of the questions to all countries [19]. An item was scored ‘1’ if adequate information was provided and bias was unlikely. An item was scored ‘0’ if the criterion was not met. An item was scored ‘?’ if the required information was lacking. Afterwards, the total methodological quality was expressed as the sum of all items receiving score ‘1’ (Table 2). In case disagreement occurred between reviewers regarding assigning a score to an item, consensus was sought during a meeting. Additionally, according to the Dutch Cochrane Centre guidelines, levels of evidence were determined for all selected studies (http://netherlands.cochrane.org).
Data on study design, research question, study region, number of participants, inclusion and exclusion criteria, timespan, applied treatment for BCRL, cost- (and other) related outcome measures and cost-related main results were extracted and summarized from the included full texts in Table 3. If studies reported both quantitative and qualitative data concerning the economic burden of BCRL, only quantitative data was extracted. If studies compared treatment costs for patients with and without BCRL, or compared (so-called) standard treatment costs and an experimental/model-based treatment cost, only the BCRL treatment costs and standard treatment costs were mentioned. To increase the interpretability of the amount of costs in the different currencies, we converted the costs that are reported in Euros, Australian Dollars or British Pounds in the ‘Results’ and/or ‘Discussion’ sections, into the USD$ currency and added them in parentheses next to the original currency. This currency exchange is based on the actual exchange rate at the time of the online publication of the article (month, year): €1=USD$1.41 (August 2009) [20] and USD$1.18 (October 2017) [21]; 1A$=USD$0.85 (December 2014) [22] and USD$0.76 (August 2016) [12]; £1=USD$1.43 (February 2018) [23].
Results
Study selection
At first, the search yielded 387 references, including duplicates. After the first screening upon title and abstract for each selected database, 28 full texts were retrieved for further scrutiny. After a second screening upon eligibility criteria (Table 1), duplicates (n = 14) were removed. Finally, eight studies were included for the ‘Results’ section of this review: 4 cohort studies [14, 22, 24, 25] and 4 cross-sectional studies [12, 20, 26, 27] respectively. Figure 1 provides a detailed flowchart of the search strategy and selection procedure.
Methodological quality
An overview of the risk of bias and level of evidence of the included studies is presented in Table 2. Regarding study quality, scores for the (partly) economic evaluations in both cohort and cross-sectional studies ranged between 6/11 and 8/11. A question that frequently scored negative or of which information was lacking, was the following: ‘Are all important parameters whose values are uncertain subjected to appropriate sensitivity analysis?’, because in most cases, the aim of the studies was to provide an overview of costs, rather than to make a cost-effectiveness evaluation. According to the Dutch Cochrane Centre guidelines, levels of evidence ranged between A2 [14, 22, 25] and B [12, 20, 24, 26, 27].
Characteristics of the included studies
Altogether, costs were analyzed of 2421 patients with BCRL from 6 out of 8 included studies which were all women [12, 14, 22, 24, 25, 27]. Two studies did not report the amount of patients upon which their cost-related outcomes were based, nor did they specify the gender of the included patients [20, 26]. Mean age of the included patients ranged between 49 [14] and 63 years [25]. One study did not define mean age [12], and in one study, this was not mentioned since results were based on a hypothetical decision model [27]. Study regions comprised the USA [14, 24,25,26,27], Australia [12, 22] and Finland [20].
Costs related to BCRL
The timespan in which costs were estimated in the different studies ranged between 12 months [20, 22, 25, 27] and 24 months [14, 24]. Either, these costs were retrieved from a convenience sample of patients with BCRL during an arbitrary follow-up of 12 months [20, 25], during the first 12 months after surgery for breast cancer [27], between 6 and 18 months after surgery [22] or during the first 24 months after surgery [14, 24].
Three studies [12, 22, 25] investigated patient-borne costs related to BCRL. Of these, two studies made a distinction between direct (i.e. costs directly related to the treatment for BCRL such as costs for therapeutic measures, physician fees, drugs, compression therapy/garment) and indirect (i.e. productivity losses; values of lost income, unpaid help and lost unpaid work) patient-borne costs [22, 25]. Mean direct costs per patient per year ranged between USD$2306 [25] and USD$2574 [22]. Indirect costs ranged between USD$3325 [25] and USD $5545 [22] costs per year. In the article by Boyages et al., the overall mean patient-borne costs for BCRL per patient per year were provided, resulting in an average of A$977 (= USD$742.52) per year [12]. Hereby, no distinction between direct and indirect costs was made.
The five remaining studies [14, 20, 24, 26, 27] discussed medical costs from a societal perspective. These included costs collected from claims data from (national) insurers [14, 20], physician Medicare fees [26, 27], hospitalization charges [24, 27] and/or manufacturer’s and service providers’ prices [20]. In these studies, no separate overview of out-of-pocket costs borne by patients was provided. One study showed that the average of non-cancer-related medical costs for BCRL was estimated on USD$45,896 per patient during 2 years (USD$22,948 per patient per year), of which USD$1083 per patient was charged for physical therapy and supplies [14]. In Bilir et al., the total 1-year economic impact with direct and indirect costs was USD$1,984,529 for standard assessment and lymphoedema treatment in 627 patients (USD$3165 per patient per year) [27]. Three studies provided an overview of solely direct costs [20, 24, 26]. Direct BCRL-related healthcare charges due to hospitalization (e.g. for systemic infections) were estimated on USD$58,088 per patient during 2 years (USD$29,044 per patient per year) [24]. Direct treatment costs after 1 year of DLT per patient were estimated on USD$3125 [26]. In Finland, total direct costs per patient treated with DLT were €799 (= USD$1126.60) per year [20]. An overview of the extracted data is shown in Table 3.
Discussion
The purpose of this systematic review was to provide an overview of the direct and indirect patient-borne as well as society-borne costs associated with the treatment of BCRL and its sequelae (Table 3 ‘main findings: costs’).
Three out of eight of the included studies were prospective cohort studies with sufficient sample size and follow-up. These studies were graded with a level of evidence A2 [14, 22, 25]. However, scores on methodological quality in terms of risk of bias of the included studies were relatively similar to each other.
This review reveals that BCRL imposes a substantial economic burden on patients and society. When solely direct costs are taken into account, in most cases, a significant proportion of costs is spent on physical therapy sessions and materials (e.g. compression garment), medication and hospital admissions in case of infections. During a 2-year post-operative period, patients with BCRL required significantly more hospitalizations and nearly seven times higher healthcare charge per patient compared to patients without BCRL (USD$141,388 vs. USD$21,141 per patient, respectively) [24]. If productivity losses were taken into account as well, the financial burden increased even more.
In the article by Stout et al., direct treatment costs associated with a traditional model of DLT were compared with costs associated with a prospective surveillance model [26]. In the USA, the cost to manage early-stage BCRL per patient per year using a prospective surveillance model was USD$636. In contrast, the costs associated with DLT using the traditional model was USD$3125 [26], highlighting the importance of an early treatment onset in favor of less invasive treatment expenses due to fewer treatment sessions and less material required.
This review comprised only one study that investigated the treatment cost for DLT in a European country, whereby results showed an average cost of €799 (= USD$1126.60) per patient per year [20]. However, more information is available concerning treatment costs for lower limb lymphoedema in European settings. Recently, Gutknecht et al. performed in Germany an observational cross-sectional study in patients with chronic lymphoedema or lipolymphoedema in order to analyze all the direct and indirect costs for patients, health insurance and society [21]. The average total cost for each patient per year was €5784 (= USD$6825.12), of which €4445 (= USD$5245.1) (76%) were direct costs and €1338 (= USD$1578.84) (24%) were indirect costs. Patient-borne costs were €648 (= USD$764.64) on average per year, wherein the highest costs were for MLD and disability costs (e.g. prescription fees including private costs for remedies and aids, payments for physician visits, hospitalization and rehabilitation, skin care products) [21]. Each year, a mean cost of €2510 (= USD$2961.80) per patient is spent on MLD, which was considered the main cost factor for statutory health insurances [21]. However, as this study relies on costs regarding the treatment for lower limb oedema, it was not included in our review. Likewise, in another recently published study of Moffatt et al., the aim was to develop and evaluate health service and patient outcomes using an appropriate model of care within a London-based primary care trust [23]. Patients with chronic swelling of the arm(s) or leg(s) were recruited and treated for a period of 6 months. Results of this study showed the benefits of a service model for chronic oedema, with clinical improvements due to a reduction in limb volume and reduced complications. Recourses moved from the acute care setting to lower-cost interventions in community: overall costs reduced from £50,171 (= USD$71,744.53) before implementation, to £27,352 = USD$39,113.96) within the first 6 months and subsequently £17,618 (= USD$25,193.74) between 6 months and 1 year [23].
Several limitations of the included studies of this review need to be discussed. First and foremost, studies investigating the financial costs related to BCRL by making use of claims data [14, 24, 27] are likely to underestimate the real cost rates [28]. Because claims data are designed for billing purposes, they only offer information of patients who are insured. Thus, they only provide an estimation of the costs related to BCRL as they do not yield information about patients with BCRL without health insurance [29]. Furthermore, one should notice that, in case only direct costs related to hospitalizations are taken into account [24], an important underestimation of the complete (direct) costs of BCRL occurs. Evaluation of resource utilization and charges associated with outpatient care would provide a more complete assessment of the impact related to BCRL [24].
Difficulties are being experienced regarding the comparability, transferability and generalizability of the present study results. Transferability is defined as the extent to which the results of a study hold true for a different population or setting [19, 30]. Since different continents, even different states/countries within the same country/continent, are subjected to different healthcare insurance policies and reimbursement procedures, it is difficult to transfer the amount of healthcare costs derived in the USA [14, 24,25,26,27] or Australia [12, 22] to European countries and vice-versa. Besides that, differences in money currencies between countries make the amount of costs derived in the different studies hard to compare. Generalizability is defined as the extent to which the results of a study can be generalized to the population from which the sample size was drawn [19, 30]. As stated by Dean et al., even findings derived from studies conducted solely in the USA are difficult to compare over time, since some of these investigations [14] conducted in the past are predate the 2010 Affordable Care Act that expanded coverage for cancer-related care [25]. Another example is the following: in Shih et al., the study sample was limited to working-age women (mean age 48.8 years); therefore, their findings regarding medical costs may not be generalizable to elderly with BCRL [14].
Limitations and strengths
In this review, literature searches were limited to mainly (bio)medical databases. The NHS Economic Evaluation Database (NHS EED) focusses primarily on the economic evaluation of healthcare interventions [31]. As a result, combining databases such as PubMed and NHS EED should have been an optimal search strategy for economic evaluations [31, 32]. Therefore, a post hoc search was performed on the NHS EED database on October 19, 2018 (https://www.crd.york.ac.uk/CRDWeb). However, this search yielded no additional eligible records.
The present systematic review contains several strengths. Firstly, it has compliance with the PRISMA guideline [18]. Furthermore, to our knowledge, this is the first overview of reported direct and indirect patient-borne as well as society-borne costs specifically associated with the treatment of BCRL, in literature. Lastly, the screening and data extraction process was performed by two blinded researchers.
Knowledge of costs related to BCRL not only improves the understanding of the economic burden of this morbidity but also launches a baseline of comparison for future cost-analytic or cost-effectiveness studies [14]. Therefore, future studies on the effectiveness of treatment modalities for BCRL should consider defining health economic analyses a priori in order to be able to withdraw proper high-quality conclusions based on cost-effectiveness outcomes such as the Incremental Cost-Effectiveness Ratio (ICER) and/or quality-adjusted life-years (QUALI). An appropriate time-horizon (≥ 12 months) should be defined and both incremental (direct and indirect) cost elements from a patient and societal perspective should be considered and collected prospectively. Additionally, it is recommended to include a generic health-related quality of life questionnaires such as the EQ-5D-5L and utility instrument to allow comparisons across interventions and populations.
Conclusion
This review reveals that BCRL imposes a substantial economic burden on patients and society. In the USA, patient-borne direct costs related to BCRL range between USD$2306 and USD$2574 per patient per year. Patient-borne indirect costs range between USD$3325 and USD$5545 per patient per year. Mean direct treatment costs after 1 year of DLT ranged between €799 (= USD$1126.60) and USD$3165. However, these conclusions are based on limited research data and due to the differences in (public) insurance protocols and currencies, it is difficult to compare costs between countries. Therefore, more standardized high-quality health economic analyses among this field are required. Additionally, recent economic analyses related to BCRL treatment in Europe, Asia, Africa and South America are lacking. Worldwide, further scrutiny of the economic impact of DLT for BCRL in clinical settings is needed.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386
Devoogdt N, Van Kampen M, Christiaens MR et al (2011) Short- and long-term recovery of upper limb function after axillary lymph node dissection. Eur J Cancer Care 20(1):77–86
Kast K, Schoffer O, Link T, Forberger A, Petzold A, Niedostatek A, Werner C, Klug SJ, Werner A, Gatzweiler A, Richter B, Baretton G, Wimberger P (2017) Trastuzumab and survival of patients with metastatic breast cancer. Arch Gynecol Obstet 296(2):303–312
Eggemann H, Altmann U, Costa SD, Ignatov A (2018) Survival benefit of tamoxifen and aromatase inhibitor in male and female breast cancer. J Cancer Res Clin Oncol 144(2):337–341
Christiansen P, Carstensen SL, Ejlertsen B et al (2018) Breast conserving surgery versus mastectomy: overall and relative survival-a population based study by the Danish Breast Cancer Cooperative Group (DBCG). Acta Oncol 57(1):19–25
Yoon TI, Hwang UK, Kim ET, Lee S, Sohn G, Ko BS, Lee JW, Son BH, Kim S, Ahn SH, Kim HJ (2017) Survival improvement in hormone-responsive young breast cancer patients with endocrine therapy. Breast Cancer Res Treat 165(2):311–320
Beckjord EB, Reynolds KA, van Londen GJ, Burns R, Singh R, Arvey SR, Nutt SA, Rechis R (2014) Population-level trends in posttreatment cancer survivors’ concerns and associated receipt of care: results from the 2006 and 2010 LIVESTRONG surveys. J Psychosoc Oncol 32(2):125–151
Lasinski BB, McKillip Thrift K, Squire D, Austin MK, Smith KM, Wanchai A, Green JM, Stewart BR, Cormier JN, Armer JM (2012) A systematic review of the evidence for complete decongestive therapy in the treatment of lymphedema from 2004 to 2011. PM R 4(8):580–601
DiSipio T, Rye S, Newman B et al (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515
Fu MR, Ridner SH, Hu SH, Stewart BR, Cormier JN, Armer JM (2013) Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psycho-oncology 22(7):1466–1484
Morgan CL, Lee BB (2008) Classification and staging of lymphedema. In Lymphedema. Springer, USA, pp 21–30
Boyages J, Xu Y, Kalfa S, Koelmeyer L, Parkinson B, Mackie H, Viveros H, Gollan P, Taksa L (2017) Financial cost of lymphedema borne by women with breast cancer. Psycho-oncology. 26(6):849–855
Armer JM, Radina ME, Porock D, Culbertson SD (2003) Predicting breast cancer-related lymphedema using self-reported symptoms. Nurs Res 52(6):370–379
Shih YC, Xu Y, Cormier JN, Giordano S, Ridner SH, Buchholz TA, Perkins GH, Elting LS (2009) Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol 27(12):2007–2014
(2013) The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology. Lymphology 46(1):1–11
Gebruers N, Verbelen H, De Vrieze T et al (2017) Current and future perspectives on the evaluation, prevention and conservative management of breast cancer related lymphoedema: a best practice guideline. Eur J Obstet Gynecol Reprod Biol 216:245–253
(2006) International Lymphoedema Framework I. Best Practice for the Management of Lymphoedema: International Consensus
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–e34
Wijnen B, Van Mastrigt G, Redekop WK et al (2016) How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: data extraction, risk of bias, and transferability (part 3/3). Expert Rev Pharmacoecon Outcomes Res 16(6):723–732
Karki A, Anttila H, Tasmuth T et al (2009) Lymphoedema therapy in breast cancer patients: a systematic review on effectiveness and a survey of current practices and costs in Finland. Acta Oncol 48(6):850–859
Gutknecht M, Herberger K, Klose K et al (2017) Cost-of-illness of patients with lymphoedema. J Eur Acad Dermatol Venereol 31(11):1930–1935
Schmitz KH, DiSipio T, Gordon LG et al (2015) Adverse breast cancer treatment effects: the economic case for making rehabilitative programs standard of care. Support Care Cancer 23(6):1807–1817
Moffatt CJ, Doherty DC, Franks PJ, Mortimer PS (2018) Community-based treatment for chronic edema: an effective service model. Lymphat Res Biol 16(1):92–99
Basta MN, Fox JP, Kanchwala SK, Wu LC, Serletti JM, Kovach SJ, Fosnot J, Fischer JP (2016) Complicated breast cancer-related lymphedema: evaluating health care resource utilization and associated costs of management. Am J Surg 211(1):133–141
Dean LT, Moss SL, Ransome Y et al (2018) “It still affects our economic situation”: long-term economic burden of breast cancer and lymphedema. Support Care Cancer
Stout NL, Pfalzer LA, Springer B, Levy E, McGarvey C, Danoff JV, Gerber LH, Soballe PW (2012) Breast cancer-related lymphedema: comparing direct costs of a prospective surveillance model and a traditional model of care. Phys Ther 92(1):152–163
Bilir SP, DeKoven MP, Munakata J (2012) Economic benefits of BIS-aided assessment of post-BC lymphedema in the United States. Am J Manag Care 18(5):234–241
Stout NL, Weiss R, Feldman JL, Stewart BR, Armer JM, Cormier JN, Shih YC (2013) A systematic review of care delivery models and economic analyses in lymphedema: health policy impact (2004-2011). Lymphology 46(1):27–41
Brayton KM, Hirsch AT, Brien OPJ et al (2014) Lymphedema prevalence and treatment benefits in cancer: impact of a therapeutic intervention on health outcomes and costs. PLoS One 9(12):e114597
Knies S, Ament AJ, Evers SM, Severens JL (2009) The transferability of economic evaluations:testing the model of Welte. Value Health 12(5):730–738
Evers SM, Hiligsmann M, Adarkwah CC (2015) Risk of bias in trial-based economic evaluations: identification of sources and bias-reducing strategies. Psychol Health 30(1):52–71
Alton V, Eckerlund I, Norlund A (2006) Health economic evaluations: how to find them. Int J Technol Assess Health Care 22(4):512–517
Acknowledgements
All authors critically revised the manuscript for important intellectual content and approved the final manuscript.
Funding
This review is financed by the Agency for Innovation by Science and Technology, applied Biomedical Research (IWT 150178). In order to arrange such financing, a separate collaboration agreement has been signed by the KU Leuven and the beneficiaries.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Support statement: ADG is a post-doctoral research fellow of the FWO-Flanders.
Appendix. Overview of the Boolean search strategies used in the different databases
Appendix. Overview of the Boolean search strategies used in the different databases
PubMed 1-10-2018 (‘Health Care Costs’[Mesh] OR ‘Health Care Costs’[All Fields] OR ‘Costs and Cost Analysis’[Mesh] OR ‘health care economics’[All Fields] OR ‘Costs and Cost Analysis’[All Fields] OR ‘Cost-Benefit Analysis’[Mesh] OR ‘Cost-Benefit Analysis’[All Fields] OR ‘Cost of Illness’[Mesh] OR ‘Cost of Illness’[All Fields] OR ‘Cost-of-illness’[All Fields] OR ‘Hospital Costs’[Mesh] OR ‘Hospital Costs’[All Fields] OR ‘Health Expenditures’[Mesh] OR ‘Health Expenditures’[All Fields] OR ‘Cost’[All Fields] OR ‘cost evaluation’[All Fields] OR ‘economic evaluation’[All Fields] OR ‘cost analysis’[All Fields] OR ‘economic analysis’[All Fields] OR ‘cost effectiveness’[All Fields]) AND (‘lymphedema’[MeSH Terms] OR ‘lymphoedema’[All Fields] OR ‘lymphedema’[All Fields]) AND (‘breast neoplasms’[All Fields] OR ‘breast neoplasms’[MeSH] OR ‘breast cancer’[All Fields] OR ‘costs’[All Fields] OR ‘breast cancer treatment’[All Fields] OR ‘direct costs’[All Fields] OR ‘health outcomes’[All Fields] OR ‘upper limb’[All Fields]) | |
Web of Science 1-10-2018 (TS=((‘Health Care Costs’ OR (‘Health’ AND ‘Care’ AND ‘Costs’) OR ‘Cost Analysis’ OR (‘costs’ AND ‘analysis’) OR ‘health care economics’ OR (‘health’ AND ‘care’ AND ‘economics’) OR ‘Cost-Benefit Analysis’ OR (‘cost-benefit’ AND ‘analysis’) OR ‘Cost of Illness’ OR (‘cost’ AND ‘illness’) OR ‘Hospital Costs’ OR (‘Hospital’ AND ‘Costs’) OR ‘Health Expenditures’ OR (‘Health’ AND ‘Expenditures’) OR ‘Cost’ OR ‘cost evaluation’ OR (‘cost’ AND ‘evaluation’) OR ‘economic evaluation’ OR (‘economic’ AND ‘evaluation’) OR ‘direct costs’ OR (‘direct’ AND ‘costs’) OR ‘health outcomes’ OR (‘health’ AND ‘outcomes’) OR ‘economic analysis’ OR (‘economic’ AND ‘analysis’) OR ‘cost effectiveness’ OR (‘cost’ AND ‘effectiveness’)) AND (‘lymphedema’ OR ‘lymphoedema’) AND (‘breast neoplasms’ OR (‘breast’ AND ‘neoplasms’) OR ‘breast cancer’ OR (‘breast’ AND ‘cancer’) OR ‘lymphedema treatment’ OR (‘lymphedema’ AND ‘treatment’) OR ‘upper limb’ OR (‘upper’ AND ‘limb’)))) AND DOCUMENT TYPES: (Article) | |
Cochrane Clinical Trials 1-10-2018 ((‘Health Care Costs’ OR ‘Costs and Cost Analysis’ OR ‘health care economics’ OR ‘Cost-Benefit Analysis’ OR ‘Cost of Illness’ OR ‘Cost-of-illness’ OR ‘Hospital Costs’ OR ‘Health Expenditures’ OR ‘Cost’ OR ‘cost evaluation’ OR ‘economic evaluation’ OR ‘cost analysis’ OR ‘economic analysis’ OR ‘cost effectiveness’ OR ‘direct costs’ OR ‘health outcomes’) AND (‘lymphedema’ OR ‘lymphoedema’) AND (‘breast neoplasms’ OR ‘breast cancer’ OR ‘lymphedema treatment’ OR ‘upper limb’)) in Title Abstract Keyword | |
EMBASE 1-10-2018 (‘health care cost’/exp OR ‘health care cost’ OR ‘cost analysis’/exp OR ‘cost analysis’ OR ‘costs’ OR ‘health care economics’/exp OR ‘health care economics’ OR ‘cost-benefit analysis’/exp OR ‘cost-benefit analysis’ OR ‘cost of illness’/exp OR ‘cost of illness’ OR ‘hospital costs’/exp OR ‘hospital costs’ OR ‘health expenditures’/exp OR ‘health expenditures’ OR ‘cost evaluation’ OR ‘economic evaluation’/exp OR ‘economic evaluation’ OR ‘direct costs’ OR ‘health outcomes’/exp OR ‘health outcomes’ OR ‘economic analysis’ OR ‘cost effectiveness’/exp OR ‘cost effectiveness’) AND (‘lymphedema’/exp OR ‘lymphedema’ OR ‘lymphoedema’/exp OR ‘lymphoedema’) AND (‘breast neoplasms’/exp OR ‘breast neoplasms’ OR ‘breast cancer’/exp OR ‘breast cancer’ OR ‘lymphedema treatment’ OR ‘upper limb’/exp OR ‘upper limb’) AND ([article]/lim OR [article in press]/lim) AND [humans]/lim |
Rights and permissions
About this article
Cite this article
De Vrieze, T., Nevelsteen, I., Thomis, S. et al. What are the economic burden and costs associated with the treatment of breast cancer-related lymphoedema? A systematic review. Support Care Cancer 28, 439–449 (2020). https://doi.org/10.1007/s00520-019-05101-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-05101-8