Abstract
Purpose
Multi-modality therapy has resulted in improved survival for childhood malignancies. The Children’s Oncology Group Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers provide practitioners with exposure- and risk-based recommendations for the surveillance and management of asymptomatic survivors who are at least 2 years from completion of therapy. This review outlines the pathophysiology and risks for oral and dental late effects in pediatric cancer survivors and the rationale for oral and dental screening recommended by the Children’s Oncology Group.
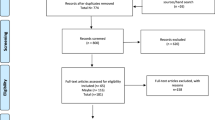
Methods
An English literature search for oral and dental complications of childhood cancer treatment was undertaken via MEDLINE and encompassed January 1975 to January 2013. Proposed guideline content based on the literature review was approved by a multi-disciplinary panel of survivorship experts and scored according to a modified version of the National Comprehensive Cancer Network “Categories of Consensus” system.
Results
The Children’s Oncology Group oral-dental panel selected 85 relevant citations. Childhood cancer therapy may impact tooth development, salivary function, craniofacial development, and temporomandibular joint function placing some childhood cancer survivors at an increased risk for poor oral and dental health. Additionally, head and neck radiation and hematopoietic stem cell transplantation increase the risk of subsequent malignant neoplasms in the oral cavity. Survivors require routine dental care to evaluate for potential side effects and initiate early treatment.
Conclusions
Certain childhood cancer survivors are at an increased risk for poor oral and dental health. Early identification of oral and dental morbidity and early interventions can optimize health and quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With contemporary multi-modality therapy, the 5-year survival rate for pediatric malignancies exceeds 80 % [1]. This success has produced 379,000 childhood cancer survivors in the USA [1]. As many as 60 to 90 % of these long-term survivors experience adverse health consequences related to cancer or its treatment, which may not manifest until years after therapy completion [2–6]. Among treatment-related sequelae, oral and dental complications are common but often overlooked sources of morbidity and impaired health-related quality of life.
This manuscript reviews the pathophysiology and risks for oral and dental late effects in childhood cancer survivors and the rationale and importance of screening recommended in the Children’s Oncology Group (COG) Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers (COG Guidelines; www.survivorshipguidelines.org) [7, 8]. Since routine dental care is not universally accessible in the USA, primary care providers (PCPs), to whom survivors return for care, play key roles in screening and early detection, hygiene recommendations, and referral for preventive and corrective dental interventions. To avoid potential complications of otherwise routine dental and orthodontic procedures, providers need to recognize late effects impacting tooth development, salivary function, and temporomandibular joint (TMJ) function and risk factors necessitating antibiotic prophylaxis prior to dental intervention. Additionally, PCPs need to be aware of the risk and presentation of oral subsequent malignant neoplasms (SMNs).
Methods
The COG Guidelines represent recommendations for risk-based screening and management of late effects that arise in asymptomatic survivors who are at least 2 years from therapy completion for pediatric and adolescent malignancies [7]. Organ-specific, multi-disciplinary panels within the COG Late Effects Committee ensure that the guidelines reflect current evidence-based research by undertaking biennial reviews of the literature. The COG panel on oral and dental complications includes expertise in pediatric and radiation oncology, pediatric radiology, oral and dental medicine, pediatric oncology nursing, and pediatric hematopoietic stem cell transplantation (HSCT).
The English literature search for oral and dental complications of cancer treatment was undertaken via MEDLINE (National Library of Medicine, Bethesda, MD, USA) and encompassed January 1975 to January 2013. Key search words included “oral health,” “dental,” “dental abnormalities,” “dental development,” “trismus,” “xerostomia,” “osteoradionecrosis,” “graft-versus-host and oral complications,” “prosthodontic chemotherapy,” “oral malignancies,” “dental antibacterial prophylaxis,” “childhood cancer,” “complications,” and “late effects.” Search criteria were then expanded using references cited in the bibliographies of selected articles. A multi-disciplinary panel of survivorship experts qualitatively evaluated each result. Structured criteria for exclusion were not applied due to the paucity of literature on this topic. Proposed guideline content based on the literature review was reviewed and approved by the panel of experts. It was scored according to a modified version of the National Comprehensive Cancer Network “Categories of Consensus” system [9]. “High-level evidence” was derived from high quality case-control or cohort studies, while “lower-level evidence” was derived from non-analytic studies, case reports, case series, and clinical experience. This review presents “Category 1” recommendations and reflects uniform consensus among the oral-dental panel that (1) there is high-level evidence linking the late effect with the therapeutic exposure and (2) the screening recommendation is appropriate based on the collective experience of panel members. The COG Guidelines and their accompanying patient education materials (“Health Links”) are available at http://www.survivorshipguidelines.org.
Results
Due to the lack of randomized controlled trials, results are derived largely from observational studies. The COG oral-dental panel selected 85 citations that were the most current and relevant from the several hundred retrieved via MEDLINE. These include a large retrospective cohort of 5-year childhood cancer survivors with longitudinal follow-up (Childhood Cancer Survivor Study [CCSS]), cross-sectional studies that evaluated survivors with and without controls, retrospective cohort studies, review articles, and clinical guidelines. Case series were included for completeness, although considered as anecdotal. Literature regarding late effects in adult cancer survivors was incorporated to extrapolate experiences, since there are few high-level evidence pediatric investigations on oral and dental late effects. The quality of current evidence is sometimes constrained by the use of convenience cohorts; retrospective data collection; small sample size; and heterogeneity in treatment approach, time since treatment, and method of ascertaining late effects.
Oral cavity development
Dental development is a complex process influenced by intense genetic signaling and controlled by a network of activators and inhibitors [10]. Primary central incisors develop as early as 6 months with most children having complete primary dentition by 3 years. Formation and eruption of permanent dentition occurs from approximately 6 to 12 years [11]. The temporal disruption or modifications of this network by cancer therapy administered during stages of tooth development can cause dental anomalies [12, 13] (Figs. 1, 2, and 3).
Hypodontia (yellow stars) and root malformation (red arrows) in a 5-year old treated for sinus rhabdomyosarcoma with chemotherapy and radiation at age 2 years with recurrence 1 year later. Dental caries (blue arrows) are on non-occlusal surfaces, which is rare in healthy individuals. (Photograph courtesy of Dr. Kaste)
Multiple dental caries (requiring crowns) with granuloma formation (blue arrows) and root malformation (red arrows) in a 14-year old treated for right infratemporal sinus rhabdomyosarcoma with surgery, chemotherapy, and radiation at age 8 years. The patient required tooth extraction and was edentulous 2 years later. (Photograph courtesy of Dr. Kaste)
Dental caries (yellow arrows) secondary to enamel hypoplasia and xerostomia in a 20-year old treated with chemotherapy and mantle radiation for Hodgkin lymphoma stage IIIb at age 8 years. Multiple periapical lucencies (blue arrows) indicate granuloma formation after prolonged infection. (Photograph courtesy of Dr. Kaste)
Impact of cancer therapy on tooth development
Structural anomalies of teeth, including hypodontia, microdontia, enamel hypoplasia, and root malformation, are increasingly recognized after childhood cancer treatment [12, 13]. The prevalence of hypodontia, which may alter craniofacial development and lead to malocclusion [14, 15], has ranged from 8.5 to 50 % depending on age at diagnosis, treatment modality, and study ascertainment methods [16–18]. In a CCSS report, childhood cancer survivors self-reported enamel hypoplasia more than twice as often as sibling controls (11.7 % versus 5.3 %) and were at higher risk for reporting root anomalies than siblings (odds ratio [OR] = 3.0 [2.2–4.0]) [19]. A retrospective evaluation of dental records and panoramic radiographs in 52 neuroblastoma survivors with a median age of 1.5 years at treatment reported hypodontia in 17 %, microdontia in 38 %, enamel hypoplasia in 17 %, and root stunting in 17 %. All of these patients received chemotherapy, and eight patients received head and neck radiation [17].
Several therapeutic exposures have been associated with dental anomalies due to the disruption of ameloblast and odontoblast activity early in life [12] (Table 1). Risk increases with treatment age younger than 5 years and higher doses of alkylating agents, especially cyclophosphamide [19–22]. Radiation involving the oral cavity also increases the risk of dental anomalies since ameloblasts can be permanently damaged by doses as low as 10 Gy [12, 19]. HSCT conditioning regimens, especially those containing total body irradiation (TBI), are cytotoxic and may lead to tooth agenesis and root anomalies [23–27]. In a study of long-term childhood cancer survivors treated before age 10 years, children who underwent HSCT with TBI had smaller root areas compared to children treated with other modalities [28].
Complications associated with dental anomalies can influence quality of life. Many childhood cancer survivors have white/cream-colored and yellow/brown opacities in the enamel and develop grooves or pits [29]. Survivors with enamel hypoplasia may have colonization with Streptococcus mutans and other bacteria, leading to an increased rate of caries formation [30, 31] (Figs. 1, 2, and 3). A population-based study from Denmark, which has universal childhood dental care, reported that caries were increased in 12-year-old children diagnosed with cancer at 5 or 6 years of age, but not in older teenage survivors [32]. This underscores the importance of routine care with biannual dental exams and yearly oral exams to ensure early intervention and treatment (Table 1). Root development should be evaluated with panoramic radiographs prior to any dental or orthodontic procedure in order to prevent complications. In a case series, five of eight orthodontists modified their treatment choice in pediatric HSCT survivors due to the extent of dental disturbances [33]. Additionally, PCPs should encourage good oral hygiene with brushing, use of fluoride toothpaste, flossing, and limitation of sweets [34].
Impact of cancer therapy on salivary gland function
Xerostomia, the subjective sensation of dry mouth, is a potential side effect following head and neck radiation or HSCT (Table 1) that can severely impact quality of life [35]. Consequences of decreased salivary secretion include increased caries (Figs. 1, 2, and 3), susceptibility to oral infections, sleep disturbances, and difficulties with chewing, swallowing, and speaking [35].
The prevalence of salivary gland dysfunction after cancer treatment varies based on measurement techniques (patient report versus stimulated or unstimulated salivary secretion rates) [36]. A review of 79 studies reported an 83.5 % prevalence of self-reported xerostomia 2 years after radiation for head and neck cancer in adults [35]. However, a study of childhood rhabdomyosarcoma survivors who received head and neck radiation showed a prevalence of only 12 % at a median follow-up of 7 years [37]. In a CCSS study, the prevalence of self-reported xerostomia in survivors was 2.8 % compared to 0.3 % in siblings, with an increased risk in survivors older than 30 years of age [19]. The discordance in xerostomia reporting between adults and children may be due to the higher doses of radiation used in adult head and neck cancers, increased co-morbidities in adult patients, or underreporting of symptoms by children [38].
The largest risk factor for xerostomia is exposure to radiation. Unlike most non-dividing tissues, salivary glands are exquisitely radiosensitive [39]. Due to their location, the salivary glands are often included in the radiation field for head and neck malignancies, i.e., nasopharyngeal carcinoma, rhabdomyosarcoma, and Hodgkin lymphoma [40]. Adult oncology data suggest that long-term severe xerostomia can usually be avoided if one parotid gland is spared to a mean dose less than 20 Gy or both glands are spared to a mean dose less than 25 Gy [41]. Additionally, risk is reduced if submandibular glands are spared [41]. Development of intensity-modulated radiotherapy (IMRT) has allowed dosimetric sparing of the parotid gland, with a hope of improved salivary function [42]. The long-term outcomes of these new modalities remain to be determined.
The association of chemotherapy alone with xerostomia is controversial [35]. One study of pediatric patients treated for a variety of tumors showed that cyclophosphamide was associated with an excess risk (OR = 12.32 [2.1–74.4]) of decreased stimulated saliva flow rates; however, no increased dental caries were noted, and patient-reported xerostomia was not evaluated [21].
In HSCT recipients, salivary gland dysfunction occurs as a result of toxicity from conditioning regimens or can be an early symptom of chronic graft-versus-host disease (cGVHD) [43, 44]. In a study of pediatric HSCT survivors, 60 % of those exposed to a conditioning regimen with cyclophosphamide and 10-Gy single-dose TBI had decreased salivary secretion rates compared to 26 % in those who received cyclophosphamide and busulfan [45]. However, another study reported no difference in the percentage of long-term survivors with decreased salivary secretion based on conditioning regimen (single-dose TBI 47 %, fractionated TBI 47 %, busulfan 42 %) [46].
In order to assess for xerostomia and determine if further testing or intervention is warranted, PCPs should ask survivors about trouble eating dry foods, problems swallowing, or the need to drink water frequently. Treatment focuses on relieving xerostomia symptoms. Pilocarpine is approved for radiation-induced xerostomia in adults and is effective in increasing salivary secretion rates as well as improving symptoms [47]. Acupuncture and saliva substitutes may also provide temporary relief. Many individuals prefer frequent sips of water to these treatments [47]. There have been no intervention trials for xerostomia in children.
Craniofacial abnormalities associated with radiation
Craniofacial abnormalities, which may impact the oral cavity, occur in 35 to 90 % of children who receive high-dose radiotherapy to the head and neck [20, 37, 48–50]. Such abnormalities are often associated with oral cavity sequelae such as dental anomalies, xerostomia, and trismus [50]. Cosmetic deformities and the requirement for multiple surgical reconstructions can deeply impact quality of life in long-term survivors [50]. Younger age at treatment and increased radiotherapy volume and dose (≥30 Gy) contribute to the extent and severity of bone and soft-tissue deformity [50] (Table 1). Since craniofacial reconstruction techniques have flourished in the last decade, cases are best managed in an individualized manner by a multi-specialty team with extensive pre-operative planning [51]. Resources for survivors with craniofacial abnormalities include FACES: The National Craniofacial Association (www.faces-cranio.org).
Radiation-induced trismus
Trismus is associated with radiotherapy effects on the TMJ, mandible, or muscles of mastication. Its prevalence ranges from 7 to 27 % in childhood nasopharyngeal carcinoma survivors [52–54]. Functional sequelae include compromised oral hygiene, poor nutrition, impaired dental care, and difficulties with speech [55–57]. Additionally, chronic pain with mouth opening can impair quality of life. While no studies in children have evaluated the radiation dose associated with trismus, an adult series reported that for each 10 Gy over 40 Gy of radiation to the pterygoid muscle, the probability of trismus increased by 24 % [58]. Adult survivors who received head and neck radiation greater than 50 Gy have the highest risk of trismus [59], and children with nasopharyngeal carcinoma typically receive doses greater than 50 Gy [52–54]. Involvement of the muscles of mastication by head and neck tumors can also increase the risk due to late fibrosis. Early intervention with prophylactic jaw-stretching exercises is crucial for patients receiving radiotherapy to the head and neck to prevent progressive fibrosis [60]. Survivors may benefit from jaw motion devices, such as TheraBite®, or trismus-release surgery [54, 61, 62].
Osteoradionecrosis (ORN) of facial bones
Oral cavity ORN is defined by the breakdown of the overlying oral mucosa for a minimum of 6 months resulting in the exposure of necrotic bone, usually the mandible, and ultimate mechanical failure of the TMJ [63]. While cohorts treated in the 1950s had ORN rates as high as 37 % [64], the incidence in adults with head and neck malignancies treated with contemporary radiation techniques is 3 to 7 % [63, 65]. ORN typically occurs within 1 to 5 years after head and neck radiation [66]; however, there are reports decades after exposure [67].
There is a paucity of ORN literature in children. In adults, ORN has been associated with radiation exposures of 40 to 50 Gy [68–70] and higher [63, 66, 71]. Increased risk due to concurrent radiation and chemotherapy [63] or radiation fractionation schedule is controversial [72, 73]. Poor pre-radiotherapy dental and periodontal status increases ORN risk [70]. Invasive dental therapy, such as the extraction of teeth included in the radiation field or periodontal surgical procedures that involve the manipulation of bone, is a potential contributing factor [65].
The use of newer radiation techniques, such as IMRT or proton beam, to reduce the mandibular dose may decrease the risk of ORN [68]. Additionally, improving pre-treatment dental hygiene is thought to enhance outcomes [71]. If oral cavity surgery is necessary after radiation, dentists and radiation oncologists should discuss the risk of ORN based on the dose and fields of radiation. Prophylactic hyperbaric oxygen therapy (HBO) before dental surgery [74, 75] and the use of prophylactic antibiotics remain controversial and have not proven to be effective in adults [63, 65]. Treatment of ORN depends on stage, with lower-grade disease being amenable to conservative measures and HBO, while advanced disease requires surgical intervention [69, 75–77].
Oral graft-versus-host disease (GVHD)
GVHD is a serious condition limited to survivors of allogeneic HSCT [43]. cGVHD typically presents 100 days or more after HSCT. Most cases manifest by 1 year, and almost all begin within 2 to 3 years [43, 78]. While the oral cavity is the second most commonly affected organ by cGVHD in adults, 9 to 45 % of children are affected [43, 79–81]. Oral cGVHD may be the primary or only indicator of cGVHD in HSCT survivors.
Signs and symptoms of oral cGVHD are similar to autoimmune disorders such as scleroderma and Sjögren syndrome [78]. They include pain, food sensitivities, taste alteration, xerostomia, and restricted mobility of the tongue or mouth [43]. Children are less likely to report these symptoms; therefore, asking directed questions is necessary. Trismus may result from skin fibrosis or musculoskeletal involvement with cGVHD. According to the National Institute of Health consensus criteria guidelines, diagnostic signs of oral cGVHD include lichenoid changes, leukoplakia, and oral range of motion difficulties [82]. Distinctive signs include mucosal ulceration or atrophy, multiple mucoceles (rare in children), pseudomembrane formation, and xerostomia or salivary gland dysfunction [82]. Gingivitis and mucosal erythema may also be seen [43, 78, 82]. Additionally, oral cGVHD can result in dental caries, difficulty in maintaining oral hygiene, or opportunistic infections [78]. Severe manifestations may impair oral intake or speech. Malignant transformation is a long-term concern [83].
Treatment of cGVHD is often challenging and typically takes months to years to control, with up to 40 % of cases unresponsive to intervention [78, 84]. Physicians should biopsy suspicious oral lesions, particularly if no other manifestations of cGVHD are present. Testing for infection should include herpes simplex virus and candida, which can co-occur with cGVHD. Erythematous and ulcerative oral lesions typically require therapy, while reticular lesions often do not. Treatment directed specifically towards oral cGVHD usually involves oral steroid rinses such as budesonide or dexamethasone [78]. Topical calcineurin inhibitors, such as cyclosporine and tacrolimus, and phototherapy have been used less commonly either individually or in combination with steroids. Topical anesthetics may be of benefit if symptoms are severe. A mouth-opening device for physical therapy may be required in the setting of trismus. Systemic immunosuppression is often required if other organs are affected [84]. When oral cGVHD is suspected or has been diagnosed, follow-up with a dental professional with experience in oral medicine every 4 to 6 months is advised [34].
SMNs associated with HSCT and radiation
Oral SMNs are well-recognized treatment-related sequelae [85]. While mucoepidermoid carcinoma of the parotid gland and oral carcinomas are uncommon in childhood, they develop at increased rates in survivors of childhood cancer, particularly after radiotherapy and HSCT [86–88]. Squamous cell carcinoma accounts for approximately one-third of solid SMNs after HSCT, with 50 % occurring in the oral cavity [89]. The CCSS reported childhood cancer survivors had a significantly higher risk of head and neck carcinoma compared to the general population (standardized incidence ratio [SIR] 13.6 [8.9–20.9]) with a prevalence of 0.2 % [87]. Like other solid SMNs, these tumors typically develop 5 to 20 years after treatment [83, 85, 87–90].
Survivors of acute lymphoblastic leukemia, neuroblastoma, soft tissue sarcomas, and Hodgkin lymphoma are at an increased risk for oral SMNs, which are usually associated with head and neck radiotherapy [87, 88]. CCSS participants who received radiation had an increased risk of head and neck SMNs compared to those who did not (SIR 18.5 versus 2.3), and 17 of 20 participants who received radiation and developed an oral SMN developed the carcinoma in a previous radiation field [87]. In HSCT survivors, conditioning regimens including TBI or limited field radiation are associated with an increased risk for oral carcinomas, with higher radiation doses (≥10 Gy single-dose or ≥ 13 Gy fractioned TBI) portending the largest risk [85, 86, 90, 91]. Additionally, survivors with cGVHD are at an increased risk for developing oral SMNs [85, 90]. Oral cGVHD was present in 23 of 26 individuals aged 14 to 67 years with oral epithelial dysplasia or squamous cell carcinoma following HSCT [89]. Host risk factors associated with an increased risk of oral cancer include younger age at HSCT and underlying cancer predisposition syndromes, such as Fanconi anemia and dyskeratosis congenita [85, 87, 88, 92, 93]. Alcohol or tobacco use also increases the risk of oral SMNs [83, 87].
PCPs and dentists should monitor survivors who received head or neck radiation therapy or HSCT annually for oral SMNs. Masses, atypical plaques, chronic ulcerations, and induration of the mucosa should be evaluated with adequate lighting. Due to the concurrent and sometimes difficult distinction between cGVHD and oral SMNs, practitioners should have a low threshold for performing a biopsy on suspicious lesions [78]. There is no evidence to support tissue autofluorescence or screening biopsies in the absence of clinical signs or symptoms [93]. Survivors should be counseled to avoid carcinogenic exposures such as tobacco use, excessive alcohol, and excessive sun exposure, which increase the risk of oral and lip cancers [94] (Table 1).
Dental antibacterial prophylaxis
Normal oral flora may enter the bloodstream with chewing, toothbrushing, and dental procedures [95]. Regular dental exams are a key element of maintaining good oral hygiene; however, transient bacteremia places some survivors at risk for serious infections. Discussion between oncologists and dentists is important to determine when antibacterial prophylaxis is necessary prior to dental procedures.
The American Heart Association (AHA), American Dental Association (ADA), and American Academy of Pediatric Dentistry (AAPD) have developed guidelines for the use of prophylactic antibiotics prior to dental procedures in certain high-risk individuals. For survivors with a history of infective endocarditis, cardiac transplant with valvulopathy, or prosthetic heart valves, antibiotics are recommended prior to procedures that involve the perforation of the mucosa or manipulation of gingival tissue or periapical region of the teeth [96]. Brain tumor survivors with ventriculoartrial, ventriculocardiac, or ventriculovenous shunts for hydrocephalus also require prophylaxis; however, it is not recommended for those with ventriculoperitoneal shunts or non-valvular devices [97]. There are no evidence-based guidelines for antibiotic prophylaxis prior to dental procedures in asplenic individuals, those with cGVHD, or other immunosuppressed survivors; hence, current use is based on individual physician practice [98, 99].
The ADA and American Academy of Orthopedic Surgeons (AAOS) published a joint evidence-based guideline in 2012 on the prevention of orthopedic implant infections in those undergoing dental procedures. The review found no clear evidence of prosthetic infections due to bacteremia after dental procedures, leading to the new limited recommendation that prophylactic antibiotics prior to dental procedures are not needed for those with hip or knee implants [100]. This may apply to survivors with various orthopedic appliances. Since this is a limited guideline, dentists, orthopedic surgeons, and PCPs should discuss risks associated with procedures on an individual basis. These updated recommendations will be reflected in the next version of the COG Guidelines.
Discussion
As the population of childhood cancer survivors expands and ages, it is important for PCPs to be aware of oral and dental treatment-related sequelae in order to facilitate early detection and interventions to optimize health and quality of life. Ideally, oral and dental health should be evaluated at initial cancer diagnosis to anticipate the potential impact of planned cancer treatment on acute and chronic problems and to stabilize existing dental disease. Maintenance of oral hygiene throughout treatment and survivorship is key. Oral and dental disturbances following childhood cancer therapy can be associated with oral infections, speech delay, poor nutrition, sleep disturbances, or facial cosmetic concerns with resultant poor quality of life.
Childhood cancer survivors are at an increased risk for oral and dental complications due to the disruption of dental developmental networks, especially when treated at a younger age. Table 1 outlines the recommendations for screening and dental care in childhood cancer survivors. PCPs should educate survivors in good general dental care, including brushing, use of fluoride toothpaste, flossing, limitation of sweets, and avoidance of tobacco products [34, 101]. Survivors should also undergo routine biannual dental exams with yearly oral exams and be referred to specialists based on the specific risks outlined herein. Life-long screening for oral SMNs is crucial in those who received head and neck radiation or underwent HSCT. Baseline panoramic radiographs should be performed prior to any dental or orthodontic care in survivors to evaluate root development. Fluoride applications are important for enamel mineralization to prevent dental caries. PCPs should monitor for xerostomia and consider saliva substitutes or moistening agents to relieve symptoms. Survivors with health conditions predisposing to bacterial endocarditis should receive antibiotic prophylaxis prior to any dental procedure as outlined above.
While these recommended dental examinations are congruent with good healthcare for all individuals, childhood cancer survivors are at a high risk for unmet oral care needs. Despite childhood cancer survivors’ risk of oral and dental sequelae, Kaste et al. reported that 28.3 % of survivors had not visited the dentist and 32.6 % had not received a dental cleaning in the previous year [19]. Lower rates of dental care are reported in uninsured and publicly insured survivors compared to those with private insurance [102]. Current lack of universal dental coverage in the USA is one reason many survivors neglect their oral health needs. However, those with dental insurance may also have difficulty finding providers equipped to treat high-risk populations. PCPs play key roles in facilitating referrals and may benefit from collaboration with local dental schools.
Additionally, survivors may be unaware of their oral and dental risks and depend on PCPs for education. Therefore, communication between PCPs, radiation oncologists, oncologists, and dentists is crucial to ensure proper care of these patients. Both PCPs and dentists benefit from having a cancer treatment summary and understanding the therapies imparting dental risk received by survivors prior to delivering care.
Oral and dental health is important for proper nutrition and quality of life; however, it is an area in which many providers receive little training. Compounding limited training, few prospective studies or randomized trials of dental intervention have been reported in childhood cancer survivors. Most knowledge of oral late effects is extrapolated from adult data, especially the epidemiology of trismus and osteoradionecrosis. Additionally, most of the literature focuses on survivors treated in the 1960s to 1990s, limiting the generalizability to survivors managed with contemporary treatment approaches. In the future, large, prospective trials evaluating oral and dental late effects and preventative or ameliorating interventions are needed to fully evaluate the risks in this population.
References
Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) (2012) SEER Cancer Statistics Review, 1975–2009 (Vintage 2009 Populations). National Cancer Institute. http://seer.cancer.gov/csr/1975_2009_pops09/. Accessed 15 September 2012
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, Friedman DL, Marina N, Hobbie W, Kadan-Lottick NS, Schwartz CL, Leisenring W, Robison LL, Childhood Cancer Survivor Study (2006) Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355:1572–1582
Armenian SH, Sun CL, Kawashima T, Arora M, Leisenring W, Sklar CA, Baker KS, Francisco L, Teh JB, Mills G, Wong FL, Rosenthal J, Diller LR, Hudson MM, Oeffinger KC, Forman SJ, Robison LL, Bhatia S (2011) Long-term health-related outcomes in survivors of childhood cancer treated with HSCT versus conventional therapy: a report from the Bone Marrow Transplant Survivor Study (BMTSS) and Childhood Cancer Survivor Study (CCSS). Blood 118:1413–1420
Blaauwbroek R, Groenier KH, Kamps WA, Meyboom-de Jong B, Postma A (2007) Late effects in adult survivors of childhood cancer: the need for life-long follow-up. Ann Oncol 18:1898–1902
Casagranda L, Trombert-Paviot B, Faure-Conter C, Bertrand Y, Plantaz D, Berger C (2013) Self-reported and record-collected late effects in long-term survivors of childhood cancer: a population-based cohort study of the Childhood Cancer Registry of the Rhone-Alpes Region (ARCERRA). Pediatr Hematol Oncol 30:195–207
Geenen MM, Cardous-Ubbink MC, Kremer LC, van den Bos C, van der Pal HJ, Heinen RC, Jaspers MW, Koning CC, Oldenburger F, Langeveld NE, Hart AA, Bakker PJ, Caron HN, van Leeuwen FE (2007) Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA 297:2705–2715
Landier W, Bhatia S, Eshelman DA, Forte KJ, Sweeney T, Hester AL, Darling J, Armstrong FD, Blatt J, Constine LS, Freeman CR, Friedman DL, Green DM, Marina N, Meadows AT, Neglia JP, Oeffinger KC, Robison LL, Ruccione KS, Sklar CA, Hudson MM (2004) Development of risk-based guidelines for pediatric cancer survivors: the children’s oncology group long-term follow-up guidelines from the children’s oncology group late effects committee and nursing discipline. J Clin Oncol 22:4979–4990
Children’s Oncology Group (2008) Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers: version 3.0. Children’s oncology group. http://www.survivorshipguidelines.org/pdf/LTFUGuidelines.pdf. Accessed 31 August 2012
Winn RJ, Botnick WZ (1997) The NCCN guideline program: a conceptual framework. Oncology (Williston Park) 11:25–32
Bei M (2009) Molecular genetics of tooth development. Curr Opin Genet Dev 19:504–510
ADA Division of Communication, Journal of the American Dental Association, ADA Council on Scientific Affairs (2005) For the dental patient. Tooth eruption: the primary teeth. J Am Dent Assoc 136(11):1619
Goho C (1993) Chemoradiation therapy: effect on dental development. Pediatr Dent 15:6–12
Cubukcu CE, Sevinir B, Ercan I (2012) Disturbed dental development of permanent teeth in children with solid tumors and lymphomas. Pediatr Blood Cancer 58:80–84
Kreczi A, Proff P, Reicheneder C, Faltermeier A (2011) Effects of hypodontia on craniofacial structures and mandibular growth pattern. Head Face Med 7:23
Suri S, Ross RB, Tompson BD (2006) Mandibular morphology and growth with and without hypodontia in subjects with Pierre Robin sequence. Am J Orthod Dentofacial Orthop 130:37–46
Kaste SC, Hopkins KP, Bowman LC (1995) Dental abnormalities in long-term survivors of head and neck rhabdomyosarcoma. Med Pediatr Oncol 25:96–101
Kaste SC, Hopkins KP, Bowman LC, Santana VM (1998) Dental abnormalities in children treated for neuroblastoma. Med Pediatr Oncol 30:22–27
Kaste SC, Hopkins KP, Jones D, Crom D, Greenwald CA, Santana VM (1997) Dental abnormalities in children treated for acute lymphoblastic leukemia. Leukemia 11:792–796
Kaste SC, Goodman P, Leisenring W, Stovall M, Hayashi RJ, Yeazel M, Beiraghi S, Hudson MM, Sklar CA, Robison LL, Baker KS (2009) Impact of radiation and chemotherapy on risk of dental abnormalities: a report from the Childhood Cancer Survivor Study. Cancer 115:5817–5827
Sonis AL, Tarbell N, Valachovic RW, Gelber R, Schwenn M, Sallan S (1990) Dentofacial development in long-term survivors of acute lymphoblastic leukemia. A comparison of three treatment modalities. Cancer 66:2645–2652
Hsieh SG, Hibbert S, Shaw P, Ahern V, Arora M (2011) Association of cyclophosphamide use with dental developmental defects and salivary gland dysfunction in recipients of childhood antineoplastic therapy. Cancer 117:2219–2227
Hutton A, Bradwell M, English M, Chapple I (2010) The oral health needs of children after treatment for a solid tumour or lymphoma. Int J Paediatr Dent 20:15–23
Holtta P, Alaluusua S, Saarinen-Pihkala UM, Peltola J, Hovi L (2005) Agenesis and microdontia of permanent teeth as late adverse effects after stem cell transplantation in young children. Cancer 103:181–190
Holtta P, Alaluusua S, Saarinen-Pihkala UM, Wolf J, Nystrom M, Hovi L (2002) Long-term adverse effects on dentition in children with poor-risk neuroblastoma treated with high-dose chemotherapy and autologous stem cell transplantation with or without total body irradiation. Bone Marrow Transplant 29:121–127
Holtta P, Hovi L, Saarinen-Pihkala UM, Peltola J, Alaluusua S (2005) Disturbed root development of permanent teeth after pediatric stem cell transplantation. Dental root development after SCT. Cancer 103:1484–1493
van der Pas-van Voskuilen IG, Veerkamp JS, Raber-Durlacher JE, Bresters D, van Wijk AJ, Barasch A, McNeal S, Gortzak RA (2009) Long-term adverse effects of hematopoietic stem cell transplantation on dental development in children. Support Care Cancer 17:1169–1175
Vaughan MD, Rowland CC, Tong X, Srivastava DK, Hale GA, Rochester R, Kaste SC (2005) Dental abnormalities after pediatric bone marrow transplantation. Bone Marrow Transplant 36:725–729
Duggal MS (2003) Root surface areas in long-term survivors of childhood cancer. Oral Oncol 39:178–183
Nasman M, Bjork O, Soderhall S, Ringden O, Dahllof G (1994) Disturbances in the oral cavity in pediatric long-term survivors after different forms of antineoplastic therapy. Pediatr Dent 16:217–223
Kohler B, Andreen I, Jonsson B (1988) The earlier the colonization by mutans streptococci, the higher the caries prevalence at 4 years of age. Oral Microbiol Immunol 3:14–17
Purdell-Lewis DJ, Stalman MS, Leeuw JA, Humphrey GB, Kalsbeek H (1988) Long term results of chemotherapy on the developing dentition: caries risk and developmental aspects. Community Dent Oral Epidemiol 16:68–71
Wogelius P, Dahllof G, Gorst-Rasmussen A, Sorensen HT, Rosthoj S, Poulsen S (2008) A population-based observational study of dental caries among survivors of childhood cancer. Pediatr Blood Cancer 50:1221–1226
Dahllof G, Jonsson A, Ulmner M, Huggare J (2001) Orthodontic treatment in long-term survivors after pediatric bone marrow transplantation. Am J Orthod Dentofacial Orthop 120:459–465
American Academy on Pediatric Dentistry Clinical Affairs C, American Academy on Pediatric Dentistry Council on Clinical A (2008) Guideline on dental management of pediatric patients receving chemotherapy, hematopoietic cell transplantation, and/or radiation. Pediatr Dent 30:219–225
Jensen SB, Pedersen AM, Vissink A, Andersen E, Brown CG, Davies AN, Dutilh J, Fulton JS, Jankovic L, Lopes NN, Mello AL, Muniz LV, Murdoch-Kinch CA, Nair RG, Napenas JJ, Nogueira-Rodrigues A, Saunders D, Stirling B, von Bultzingslowen I, Weikel DS, Elting LS, Spijkervet FK, Brennan MT, Salivary Gland Hypofunction/Xerostomia Section, Oral Care Study Group, Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) (2010) A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: prevalence, severity and impact on quality of life. Support Care Cancer 18(8):1039–1060
Garming Legert K, Remberger M, Ringden O, Heimdahl A, Dahllof G (2012) Salivary secretion in children after fractionated or single-dose TBI. Bone Marrow Transplant 47:404–410
Paulino AC, Simon JH, Zhen W, Wen BC (2000) Long-term effects in children treated with radiotherapy for head and neck rhabdomyosarcoma. Int J Radiat Oncol Biol Phys 48:1489–1495
Dahllof G (2008) Oral and dental late effects after pediatric stem cell transplantation. Biol Blood Marrow Transpl 14:81–83
Guchelaar HJ, Vermes A, Meerwaldt JH (1997) Radiation-induced xerostomia: pathophysiology, clinical course and supportive treatment. Support Care Cancer 5:281–288
Selo N, Bolling T, Ernst I, Pape H, Martini C, Rube C, Timmermann B, Fischedick K, Kortmann RD, Gerss J, Koch R, Willich N (2010) Acute toxicity profile of radiotherapy in 690 children and adolescents: RiSK data. Radiother Oncol 97:119–126
Deasy JO, Moiseenko V, Marks L, Chao KS, Nam J, Eisbruch A (2010) Radiotherapy dose-volume effects on salivary gland function. Int J Radiat Oncol Biol Phys 76:S58–S63
Kam MK, Leung SF, Zee B, Chau RM, Suen JJ, Mo F, Lai M, Ho R, Cheung KY, Yu BK, Chiu SK, Choi PH, Teo PM, Kwan WH, Chan AT (2007) Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol 25:4873–4879
Treister NS, Woo SB, O’Holleran EW, Lehmann LE, Parsons SK, Guinan EC (2005) Oral chronic graft-versus-host disease in pediatric patients after hematopoietic stem cell transplantation. Biol Blood Marrow Transpl 11:721–731
Imanguli MM, Atkinson JC, Mitchell SA, Avila DN, Bishop RJ, Cowen EW, Datiles MB, Hakim FT, Kleiner DE, Krumlauf MC, Pavletic SZ (2010) Salivary gland involvement in chronic graft-versus-host disease: prevalence, clinical significance, and recommendations for evaluation. Biol Blood Marrow Transpl 16:1362–1369
Dahllof G, Wondimu B, Barr-Agholme M, Garming-Legert K, Remberger M, Ringden O (2011) Xerostomia in children and adolescents after stem cell transplantation conditioned with total body irradiation or busulfan. Oral Oncol 47:915–919
Garming-Legert K, Remberger M, Ringden O, Hassan M, Dahllof G (2011) Long-term salivary function after conditioning with busulfan, fractionated or single-dose TBI. Oral Dis 17:670–676
Jensen SB, Pedersen AM, Vissink A, Andersen E, Brown CG, Davies AN, Dutilh J, Fulton JS, Jankovic L, Lopes NN, Mello AL, Muniz LV, Murdoch-Kinch CA, Nair RG, Napenas JJ, Nogueira-Rodrigues A, Saunders D, Stirling B, von Bultzingslowen I, Weikel DS, Elting LS, Spijkervet FK, Brennan MT, Salivary Gland Hypofunction/Xerostomia Section, Oral Care Study Group, Multinational Association of Supportive Care in Cancer (MASCC)/International Society of Oral Oncology (ISOO) (2010) A systematic review of salivary gland hypofunction and xerostomia induced by cancer therapies: management strategies and economic impact. Support Care Cancer 18(8):1061–1079
Denys D, Kaste SC, Kun LE, Chaudhary MA, Bowman LC, Robbins KT (1998) The effects of radiation on craniofacial skeletal growth: a quantitative study. Int J Pediatr Otorhinolaryngol 45:7–13
Raney RB, Asmar L, Vassilopoulou-Sellin R, Klein MJ, Donaldson SS, Green J, Heyn R, Wharam M, Glicksman AS, Gehan EA, Anderson J, Maurer HM (1999) Late complications of therapy in 213 children with localized, nonorbital soft-tissue sarcoma of the head and neck: a descriptive report from the Intergroup Rhabdomyosarcoma Studies (IRS)-II and -III. IRS Group of the Children’s Cancer Group and the Pediatric Oncology Group. Med Pediatr Oncol 33:362–371
Gevorgyan A, La Scala GC, Neligan PC, Pang CY, Forrest CR (2007) Radiation-induced craniofacial bone growth disturbances. J Craniofac Surg 18:1001–1007
Rohner D, Guijarro-Martinez R, Bucher P, Hammer B (2013) Importance of patient-specific intraoperative guides in complex maxillofacial reconstruction. J Craniomaxillofac Surg 41:382–390
Daoud J, Toumi N, Bouaziz M, Ghorbel A, Jlidi R, Drira MM, Frikha M (2003) Nasopharyngeal carcinoma in childhood and adolescence: analysis of a series of 32 patients treated with combined chemotherapy and radiotherapy. Eur J Cancer 39:2349–2354
Kupeli S, Varan A, Ozyar E, Atahan IL, Yalcin B, Kutluk T, Akyuz C, Buyukpamukcu M (2006) Treatment results of 84 patients with nasopharyngeal carcinoma in childhood. Pediatr Blood Cancer 46:454–458
Zubizarreta PA, D’Antonio G, Raslawski E, Gallo G, Preciado MV, Casak SJ, Scopinaro M, Morales G, Sackmann-Muriel F (2000) Nasopharyngeal carcinoma in childhood and adolescence: a single-institution experience with combined therapy. Cancer 89:690–695
Otmani N (2007) Oral and maxillofacial side effects of radiation therapy on children. J Can Dent Assoc 73:257–261
Goldstein M, Maxymiw WG, Cummings BJ, Wood RE (1999) The effects of antitumor irradiation on mandibular opening and mobility: a prospective study of 58 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:365–373
Louise Kent M, Brennan MT, Noll JL, Fox PC, Burri SH, Hunter JC, Lockhart PB (2008) Radiation-induced trismus in head and neck cancer patients. Support Care Cancer 16:305–309
Teguh DN, Levendag PC, Voet P, van der Est H, Noever I, de Kruijf W, van Rooij P, Schmitz PI, Heijmen BJ (2008) Trismus in patients with oropharyngeal cancer: relationship with dose in structures of mastication apparatus. Head Neck 30:622–630
Johnson J, van As-Brooks CJ, Fagerberg-Mohlin B, Finizia C (2010) Trismus in head and neck cancer patients in Sweden: incidence and risk factors. Med Sci Monit 16:CR278–CR282
Tang Y, Shen Q, Wang Y, Lu K, Wang Y, Peng Y (2011) A randomized prospective study of rehabilitation therapy in the treatment of radiation-induced dysphagia and trismus. Strahlenther Onkol 187:39–44
Ferri A, Bianchi B, Leporati M, Sesenna E (2011) Anterolateral thigh free flap for trismus release in pediatric oncology patients. Br J Oral Maxillofac Surg 49:e58–e60
Chen YY, Zhao C, Wang J, Ma HL, Lai SZ, Liu Y, Han F, Lu LX, Bao Y, Chen M (2011) Intensity-modulated radiation therapy reduces radiation-induced trismus in patients with nasopharyngeal carcinoma: a prospective study with >5 years of follow-up. Cancer 117:2910–2916
Nabil S, Samman N (2012) Risk factors for osteoradionecrosis after head and neck radiation: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol 113:54–69
Gaisford J, Rueckert F (1956) Osteoradionecrosis of the mandible. Plast Reconstr Surg 18(1946):436–447
Wahl MJ (2006) Osteoradionecrosis prevention myths. Int J Radiat Oncol Biol Phys 64:661–669
Curi MM, Dib LL (1997) Osteoradionecrosis of the jaws: a retrospective study of the background factors and treatment in 104 cases. J Oral Maxillofac Surg 55:540–544, discussion 545–546
Chrcanovic BR, Reher P, Sousa AA, Harris M (2010) Osteoradionecrosis of the jaws–a current overview–part 1: physiopathology and risk and predisposing factors. Oral Maxillofac Surg 14:3–16
Tsai CJ, Hofstede TM, Sturgis EM, Garden AS, Lindberg ME, Wei Q, Tucker SL, Dong L (2013) Osteoradionecrosis and radiation dose to the mandible in patients with oropharyngeal cancer. Int J Radiat Oncol Biol Phys 85:415–420
Ashamalla HL, Thom SR, Goldwein JW (1996) Hyperbaric oxygen therapy for the treatment of radiation-induced sequelae in children. The University of Pennsylvania experience. Cancer 77:2407–2412
Schuurhuis JM, Stokman MA, Roodenburg JL, Reintsema H, Langendijk JA, Vissink A, Spijkervet FK (2011) Efficacy of routine pre-radiation dental screening and dental follow-up in head and neck oncology patients on intermediate and late radiation effects. A retrospective evaluation. Radiother Oncol 101:403–409
Jereczek-Fossa BA, Orecchia R (2002) Radiotherapy-induced mandibular bone complications. Cancer Treat Rev 28:65–74
Dische S, Saunders M, Barrett A, Harvey A, Gibson D, Parmar M (1997) A randomised multicentre trial of CHART versus conventional radiotherapy in head and neck cancer. Radiother Oncol 44:123–136
Niewald M, Barbie O, Schnabel K, Engel M, Schedler M, Nieder C, Berberich W (1996) Risk factors and dose-effect relationship for osteoradionecrosis after hyperfractionated and conventionally fractionated radiotherapy for oral cancer. Br J Radiol 69:847–851
Chuang SK (2012) Limited evidence to demonstrate that the use of hyperbaric oxygen (HBO) therapy reduces the incidence of osteoradionecrosis in irradiated patients requiring tooth extraction. J Evid Based Dent Pract 12:248–250
David LA, Sandor GK, Evans AW, Brown DH (2001) Hyperbaric oxygen therapy and mandibular osteoradionecrosis: a retrospective study and analysis of treatment outcomes. J Can Dent Assoc 67:384
Mounsey RA, Brown DH, O’Dwyer TP, Gullane PJ, Koch GH (1993) Role of hyperbaric oxygen therapy in the management of mandibular osteoradionecrosis. Laryngoscope 103:605–608
Hirsch DL, Bell RB, Dierks EJ, Potter JK, Potter BE (2008) Analysis of microvascular free flaps for reconstruction of advanced mandibular osteoradionecrosis: a retrospective cohort study. J Oral Maxillofac Surg 66:2545–2556
Meier JK, Wolff D, Pavletic S, Greinix H, Gosau M, Bertz H, Lee SJ, Lawitschka A, Elad S, International Consensus Conference on Clinical Practice in cGVHD (2011) Oral chronic graft-versus-host disease: report from the International Consensus Conference on clinical practice in cGVHD. Clin Oral Investig 15(2):127–139
Flowers ME, Parker PM, Johnston LJ, Matos AV, Storer B, Bensinger WI, Storb R, Appelbaum FR, Forman SJ, Blume KG, Martin PJ (2002) Comparison of chronic graft-versus-host disease after transplantation of peripheral blood stem cells versus bone marrow in allogeneic recipients: long-term follow-up of a randomized trial. Blood 100:415–419
Nicolatou-Galitis O, Kitra V, Van Vliet-Constantinidou C, Peristeri J, Goussetis E, Petropoulos D, Grafakos S (2001) The oral manifestations of chronic graft-versus-host disease (cGVHD) in paediatric allogeneic bone marrow transplant recipients. J Oral Pathol Med 30:148–153
Mays JW, Fassil H, Edwards DA, Pavletic SZ, Bassim CW (2013) Oral chronic graft-versus-host disease: current pathogenesis, therapy, and research. Oral Dis 19:327–346
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, Martin P, Chien J, Przepiorka D, Couriel D, Cowen EW, Dinndorf P, Farrell A, Hartzman R, Henslee-Downey J, Jacobsohn D, McDonald G, Mittleman B, Rizzo JD, Robinson M, Schubert M, Schultz K, Shulman H, Turner M, Vogelsang G, Flowers MED (2005) National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant 11:945–956
Demarosi F, Lodi G, Carrassi A, Soligo D, Sardella A (2005) Oral malignancies following HSCT: graft versus host disease and other risk factors. Oral Oncol 41:865–877
Baird K, Cooke K, Schultz KR (2010) Chronic graft-versus-host disease (GVHD) in children. Pediatr Clin North Am 57:297–322
Curtis RE, Rowlings PA, Deeg HJ, Shriner DA, Socie G, Travis LB, Horowitz MM, Witherspoon RP, Hoover RN, Sobocinski KA, Fraumeni JF Jr, Boice JD Jr (1997) Solid cancers after bone marrow transplantation. N Engl J Med 336:897–904
Socie G, Curtis RE, Deeg HJ, Sobocinski KA, Filipovich AH, Travis LB, Sullivan KM, Rowlings PA, Kingma DW, Banks PM, Travis WD, Witherspoon RP, Sanders J, Jaffe ES, Horowitz MM (2000) New malignant diseases after allogeneic marrow transplantation for childhood acute leukemia. J Clin Oncol 18:348–357
Bassal M, Mertens AC, Taylor L, Neglia JP, Greffe BS, Hammond S, Ronckers CM, Friedman DL, Stovall M, Yasui YY, Robison LL, Meadows AT, Kadan-Lottick NS (2006) Risk of selected subsequent carcinomas in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 24:476–483
Inskip PD, Curtis RE (2007) New malignancies following childhood cancer in the United States, 1973–2002. Int J Cancer 121:2233–2240
Mawardi H, Elad S, Correa ME, Stevenson K, Woo SB, Almazrooa S, Haddad R, Antin JH, Soiffer R, Treister N (2011) Oral epithelial dysplasia and squamous cell carcinoma following allogeneic hematopoietic stem cell transplantation: clinical presentation and treatment outcomes. Bone Marrow Transplant 46:884–891
Rizzo JD, Curtis RE, Socie G, Sobocinski KA, Gilbert E, Landgren O, Travis LB, Travis WD, Flowers ME, Friedman DL, Horowitz MM, Wingard JR, Deeg HJ (2009) Solid cancers after allogeneic hematopoietic cell transplantation. Blood 113:1175–1183
Bhatia S, Louie AD, Bhatia R, O’Donnell MR, Fung H, Kashyap A, Krishnan A, Molina A, Nademanee A, Niland JC, Parker PA, Snyder DS, Spielberger R, Stein A, Forman SJ (2001) Solid cancers after bone marrow transplantation. J Clin Oncol 19:464–471
Baker KS, DeFor TE, Burns LJ, Ramsay NK, Neglia JP, Robison LL (2003) New malignancies after blood or marrow stem-cell transplantation in children and adults: incidence and risk factors. J Clin Oncol 21:1352–1358
Treister N, Duncan C, Cutler C, Lehmann L (2012) How we treat oral chronic graft-versus-host disease. Blood 120:3407–3418
Hudson MM, Hester A (2008) Health link: reducing the risk of second cancers, version 3.0. Chidren’s Oncology Group. http://www.survivorshipguidelines.org/pdf/ReducingSecondCancerRisk.pdf. Accessed 15 September 2012
Lockhart PB, Brennan MT, Sasser HC, Fox PC, Paster BJ, Bahrani-Mougeot FK (2008) Bacteremia associated with toothbrushing and dental extraction. Circulation 117:3118–3125
Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT, American Heart Association (2008) Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. J Am Dent Assoc 139(Suppl):3S–24S
American Academy on Pediatric Dentistry Clinical Affairs Committee, American Academy on Pediatric Dentistry Council on Clinical Affairs (2008) Guideline on antibiotic prophylaxis for dental patients at risk for infection. Pediatr Dent 30(7 Suppl):215–218
Tate AR, Norris CK, Minniti CP (2006) Antibiotic prophylaxis for children with sickle cell disease: a survey of pediatric dentistry residency program directors and pediatric hematologists. Pediatr Dent 28:332–335
Price VE, Blanchette VS, Ford-Jones EL (2007) The prevention and management of infections in children with asplenia or hyposplenia. Infect Dis Clin North Am 21:697–710, viii-ix
Watters W 3rd, Rethman MP, Hanson NB, Abt E, Anderson PA, Carroll KC, Futrell HC, Garvin K, Glenn SO, Hellstein J, Hewlett A, Kolessar D, Moucha C, O’Donnell RJ, O’Toole JE, Osmon DR, Evans RP, Rinella A, Steinberg MJ, Goldberg M, Ristic H, Boyer K, Sluka P, Martin WR 3rd, Cummins DS, Song S, Woznica A, Gross L (2013) Prevention of orthopaedic implant infection in patients undergoing dental procedures. J Am Acad Orthop Surg 21:180–189
(2002) For the dental patient: oral care for cancer patients. J Am Dent Assoc 133 (7):1014.
Casillas J, Castellino SM, Hudson MM, Mertens AC, Lima IS, Liu Q, Zeltzer LK, Yasui Y, Robison LL, Oeffinger KC (2011) Impact of insurance type on survivor-focused and general preventive health care utilization in adult survivors of childhood cancer: the Childhood Cancer Survivor Study (CCSS). Cancer 117:1966–1975
Acknowledgments
This research was supported by the Children’s Oncology Group Chair’s Grant U10 CA098543.
Disclosures
Dr. Migliorati is a consultant for Amgen Inc. and Colgate.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Effinger, K.E., Migliorati, C.A., Hudson, M.M. et al. Oral and dental late effects in survivors of childhood cancer: a Children’s Oncology Group report. Support Care Cancer 22, 2009–2019 (2014). https://doi.org/10.1007/s00520-014-2260-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-014-2260-x