Abstract
Introduction
The severity of anorexia correlates with the presence of early satiety. The sense of fullness limits nutritional intake. The symptom is poorly understood because most assessment questionnaires do not include early satiety.
Methods
Patients rarely volunteer early satiety. Central and peripheral mechanisms may be involved in the genesis of early satiety. These would include central sensory specific satiety, food aversions, diurnal changes in intake, gastric motility and accommodation and as gastrointestinal hormones.
Conclusions
Prokinetic medications, such as metoclopramide are used to treat early satiety. However, other medications which influence gastric accommodation such as clonidine, sumatriptan, or sildenafil, or diminish enteric afferent output such as kappa opioid receptor agonists, may favorably influence early satiety and should be subject to future research. Translational research is needed to understand the relationship of early satiety to gastric motility and accommodation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anorexia is one of the most common and important symptoms in advanced cancer. One of the main determinants of the severity of anorexia is the symptom of early satiety, yet most symptom questionnaires do not even include early satiety as a symptom, and most patients do not spontaneously report early satiety. Early satiety is sometimes used synonymously with chronic nausea, yet in our experience, early satiety is a distinctly different cancer symptom. As a result, early satiety is both poorly understood and underrecognized, and it can be characterized as an orphan cancer symptom. We wrote this article to draw attention to the importance of early satiety, emphasize its prevalence as a significant cancer symptom, discuss its pathophysiology, and consider the therapeutic implications.
Definition
Early satiety is the desire to eat associated with the subsequent inability to eat (except for small amounts) due to a sense of fullness [1, 2]. Early satiety can occur without anorexia [2, 3]. However, early satiety is experienced by most cancer patients with appetite loss [4]. Early satiety may also be associated with affective changes (unlike those with cancer anorexia but without early satiety) [4]. Most patients with early satiety complain of anorexia, yet when fasted, they become hungry like normal individuals [5]. Perception of satiety is based in part upon the amount eaten rather than the hunger experienced [5].
Prevalence
In a prospective study of symptoms in 1,000 advanced cancer patients referred to the Cleveland Clinic palliative medicine service, early satiety was among the top 10 common established symptoms. It was subsequently found to cluster with anorexia, weight loss, and taste changes, but not nausea or vomiting. (L. Rybicki, personal communication). In our own experience, early satiety occurs in many advanced cancer patients and is more prevalent than other well-identified symptoms, like nausea, vomiting, and depression [4, 6–9]. Early satiety is gender-related, being more common in females [4, 7, 10]. Prevalence does not appear related to primary site, nor is early satiety related to current chemotherapy or radiation. However, it would be of interest to know if patients with delayed nausea and vomiting from cancer chemotherapy have underlying early satiety (pre- or postchemotherapy) as a predisposing factor.
In a study of patient-volunteered vs systematically assessed symptoms, only 4 out of 97 patients with advanced cancer and early satiety volunteered it as a symptom without being formally asked [11]. It would be of interest to know why patients fail to report early satiety despite the apparent high prevalence and severity. Patients themselves may not have any insight into this symptom, and thus, they fail to volunteer it. Alternatively, if physicians do not specifically inquire about it, patients are unlikely to give it importance. Early satiety may be considered by some to be chronic nausea, and it may be miscategorized as such. This may also account for the variations in reported prevalence. Early satiety appears to be a major contributor to reduced food intake in cancer, increases in prevalence with disease progression, and is an independent prognostic indicator both in our studies and in those of other investigators [2–4].
Early satiety and symptom assessment tools
Although early satiety is prevalent, prognostic, and significantly related to anorexia, none of the validated general cancer symptom assessment tools include early satiety (J. Kirkova, personal communication). Only those instruments specifically designed for anorexia include any questions about early satiety; the Functional Assessment of Anorexia/Cachexia Therapy (FAACT), the Bristol-Myers Anorexia/Cachexia Recovery (BACRI) Instrument, and the Subjective Global Assessment tool for nutrition [12–14]. A gastroparesis symptom assessment tool, the Gastroparesis Cardinal Symptom Index (which has been validated), measures the severity of postprandial fullness/early satiety, nausea, vomiting, and bloating [15].
Early satiety and severity of anorexia
Retrospective analysis using nonparametric statistics (Spearman’s correlation) of two of our previous symptom studies revealed moderate association between anorexia and satiety [7] (Tables 1 and 2). We recently confirmed (Table 3) our previous observation on the relationship between the severity of anorexia and the presence of early satiety by using a symptom checklist and an anorexia severity grading by both a categorical and a numerical scale (T. Yavuzsen, personal communication). These analyses confirm a moderate correlation between the severity of anorexia and the presence and severity of early satiety. Supporting this, others have found food intake correlated directly with hunger ratings, but food intake correlated inversely with a sense of fullness [16].
Early satiety: pathophysiology
Evidence suggests early satiety has both central and peripheral etiologies. Central influences may be related to taste changes, food aversions, and diurnal variations in food intake. Peripheral changes may include lack of gastric accommodation, delayed gastric emptying, or altered enteric neuron sensory signals.
Central
There is vigorous control of energy intake and expenditures to maintain normal body weight by negative feedback controls [17]. Total food intake is a product of both meal size and frequency. As a meal progresses, signals are initiated that generate satiation [16] proportionate to the quantity and quality of food consumed. There is also synchrony of food with water intake such that anorexia may also predispose to dehydration [9, 17].
Food aversions contribute to satiation in cancer. Humans normally eat more when offered a variety of foods. Sensory-specific satiety relates to the pleasantness of a meal. Taste variety increases the volume consumed before satiation occurs [18]. Olfactory aversion governs the unpleasantness of food [19]. Taste and smell may both reduce food consumption and increase satiation. The medial orbitofrontal cortex (which generates signals that induce pleasure in a meal) can also cause satiation from unpleasant foods and food aversions, resulting in reduced energy intake and meal volume [18, 19]. Higher food temperatures worsen aversions in cancer and increase satiation, while lower temperatures minimize aversion [9].
Diurnal variations in food intake frequently accompany anorexia and early satiety. In animals, light input from the retina governs the rate of firing of appetite pacemaker cells and controls food intake with variations in light exposure. In humans, there is a 150% increase in food intake as the day progresses relative to the morning; larger portions are more frequent later in the day, and satiety (defined as meal interval divided by meal sizes) decreases during the day [20, 21]. However, in advanced cancer, we have found that approximately 60% have diurnal variation in appetite (T. Yavuzsen, personal communication); satiety is less in cancer patients in the morning. Altered hypothalamic function may lead to changes in diurnal feeding patterns in animals and man, loss of appetite, autonomic dysfunction, reduced meal size, and increased satiation [9, 22]. Corticotropin-releasing hormone (CRH) derived from the hypothalamus decreases gastric motility and may increase satiety under the stress of cancer [23]. Cannabinoids appear to down modulate CRH in the hypothalamus, which may be one of the mechanism by which energy intake is improved by drugs such as nabilone [24].
Peripheral
Gastric dysmotility
Satiety signals from the stomach reflect food and liquid volume and gastric distension rather than nutritional content. However, nutrient content does generate satiety signals from the small bowel [25]. Total vagotomy attenuates but does not eliminate satiation from gastric distention. In our study of autonomic dysfunction in advanced cancer, there was no association between the degree of dysfunction and early satiety [26]. Sensory afferents within splanchnic sympathetic nerves play a role [25]. Enteric afferents have kappa receptors, which send signals centrally through sympathetic neural pathways. Kappa receptor agonists, like asimadoline, reduce early satiety in the functional bowel syndrome [27, 28]. Food-related drinking is activated without cellular or extracellular fluid deficits but is inhibited by vagotomy and histamine blockade (H1 receptors) [29]. Early satiety may thus predispose to dehydration [29].
There is normally a correlation between rising gastric pressures, a sense of fullness and satiation, with an inverse relationship between gastric distention and appetite [19]. Lack of gastric accommodation likely produces early satiety and meal termination [30–33]. Methods of measuring gastric accommodation include gastric barostat distention, radioisotope mixed with food, paracetamol absorption, magnetic resonance imaging, and a satiety drinking test [32–35]. Reduced accommodation accounts for 40% of functional dyspepsia, but it is unknown if it occurs in advanced cancer. Cisapride and sumatriptan improve satiety by improving accommodation; erythromycin reduces accommodation, and so, it may paradoxically worsen early satiety. Clonidine, nitroglycerin, and sildenafil improve gastric accommodation [28, 36]. Those unresponsive to prokinetic agents may have reduced accommodation and might respond to these medications. This requires further research.
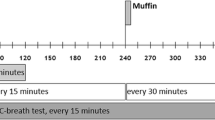
Gastric emptying can be measured by nuclear scintigraphy, ultrasound, real-time paramagnetic resonance imaging, the hydrogen breath test following lactulose ingestion, radio-labeled CO2 breath test, the 13C octanoic acid breath test, and acetaminophen absorption [36, 37]. Most cancer patients with severe early satiety have delayed upper gastrointestinal transit [39, 40]. Prokinetics remain the treatment of choice, but many fail to respond or develop side effects [38–41]. Prokinetics include domperidone, erythromycin, macrolides, metoclopramide, and muscarinic cholinergics, like bethanecol and tegaserod [42]. Finally, visceral hypersensitivity may lead to early satiety [33]. Asimadoline, a kappa opioid receptor agonist, does not cross the blood–brain barrier, but it reduces early satiety and bloating in functional dyspepsia (without changing motility) by altering enteric sensory afferent signals [27].
Gastric and small-bowel hormones
Little is known about the relationship of small-bowel hormones to early satiety in cancer. It is possible that cancer satiety may be associated with increased levels of these hormones, increased expression of their receptors, or resistance to ghrelin.
Ghrelin
Ghrelin is a growth hormone secretagogue expressed in the stomach that releases neuropeptide Y and stimulates gastric motility [43, 44]. Normally, levels peak before meals and fall within an hour. It increases appetite at normal physiologic concentrations in normal individuals (unlike corticosteroids). Ghrelin levels are inversely proportional to fat mass and leptin levels [45]. In advanced cancer, ghrelin levels increase and positively correlate with the severity of both anorexia and cachexia [46, 47]. There is a resistance to ghrelin-induced appetite in advanced cancer. Ghrelin infusions improve satisfaction with a meal and energy intake in cancer but without changing gastric emptying [45, 47, 48].
Cholecystokinin
Fat and protein intake releases cholecystokinin from the small bowel. Cholecystokinin produces satiety and reduces food intake by vagal or hypothalamic effects more by inducing satiety rather than reducing appetite [19]. Satiation from cholecystokinin is blocked by loxiglumide, a competitive cholecystokinin (CCK) antagonist.
Glucagon-like protein
Glucagon-like protein (GLP-1) is released from the ileum in response to fat and carbohydrate. The inhibition of spontaneous motor activity in the duodenum and antrum of the stomach by unabsorbed nutrients in the ileum is called the ileal break. GLP-1 is responsible for the ileal break in food transit and reduced gastric emptying [16, 41]. Pyloric pressures and gastric distention both increase with GLP-1 [19, 49]. GLP-1 infusions produce satiety and reduce caloric intake [19, 44].
Bombesin
Bombesin and its human analog gastrin inhibitory peptide reduce appetite [50]. Bombesin releases cholecystokinin and also inhibits gastric emptying in humans independent of cholecystokinin [17, 19].
Management
Effective management of early satiety will probably require treatment for both central (food aversion and anorexia) and peripheral (gastroparesis, lack of accommodation, and increased enteric neuronal afferent input) factors. Frequent small meals may help. Fat has a weaker satiety effect than protein or carbohydrate [51]. Increased dietary fat may reduce intrameal satiety. Colder food temperatures may reduce food aversion. Treatment with an appetite stimulant may theoretically worsen early satiety because increased food intake from the appetite stimulant conflicts with the physiological inability to process the food consumed. However, central causes of anorexia or early satiety may be treated with megestrol acetate (which improves the taste of food), with ghrelin to increase appetite, or with cannabinoids to reduce CRH. The peripheral causes may be treated with prokinetics such as domperidone and metoclopramide. Reduced gastric accommodation may improve with clonidine, nitroglycerin, sildenafil, or sumatriptan (although this is speculative). Hypersensitivity due to increased enteric afferent signals may be blocked by asimadoline.
Summary
Although early satiety is one of the most common symptoms in advanced cancer, we know little about its pathophysiology. All validated symptom scales (except those specifically for anorexia) ignore early satiety, although it is a common complaint in cancer. Early satiety is rarely volunteered, yet it is a significant contributing factor to the severity of anorexia. Patients frequently refer it to as anorexia despite the fact that appetite in those with early satiety improves with fasting. Early satiety appears related to food aversions, taste changes, and diurnal changes in meal pattern. Physicians can misclassify early satiety as nausea. Early satiety is likely to be caused by both central and peripheral factors, and treatment will require medications that correct both. The few treatment studies published only involve prokinetic agents. No randomized controlled trials in the management of early satiety have been performed. Translational research is needed to understand the relationship of early satiety to changes in gastric motility and accommodation, gastric, and small-bowel hormones. Noninvasive means of measuring gastric emptying and accommodation used in functional dyspepsia should also be used to study early satiety in cancer.
References
Sarhill N, Christie R (2002) Early satiety in advanced cancer: a common unrecognized symptom (letter)? Am J Hospice Palliat Care 19(5):305
Theologides A (1976) Anorexia-producing intermediary metabolites. Am J Clin Nutr 29:552–558
Theologides A (1979) Cancer cachexia. Cancer 43:2004–2012
Walsh D, Donnelly S, Rybicki L (2000) The symptoms of advanced cancer: relationship to age, gender, and performance status in 1,000 patients. Support Care Cancer 8(3):175–179
Armes PJ, Plant HJ, Allbright A, Silverstone T, Slevin ML (1992) A study to investigate the incidence of early satiety in patients with advanced cancer. Br J Cancer 65(3):481–484
Donnelly S, Walsh D (1995) The symptoms of advanced cancer. Semin Oncol 22(2 Suppl 3):67–72
Donnelly S, Walsh D, Rybicki L (1995) The symptoms of advanced cancer: identification of clinical and research priorities by assessment of prevalence and severity. J Palliat Care 11(1):27–32
Komurcu S, Nelson KA, Walsh D, Ford RB, Rybicki LA (2002) Gastrointestinal symptoms among inpatients with advanced cancer. Am J Hospice Palliat Care 19(5):351–355
Sarhill N, Mahmoud F, Walsh D, Nelson KA, Komurcu S, Davis M, LeGrand S, Abdullah O, Rybicki L (2003) Evaluation of nutritional status in advanced metastatic cancer. Support Care Cancer 11(10):652–659
Nielsen SS, Theologides A, Vickers ZM (1980) Influence of food odors on food aversions and preferences in patients with cancer. Am J Clin Nutr 33(11):2253–2261
Homsi J, Walsh D, Nelson KA, Gvozdjan D, Pham H, Rivera N (2001) Symptom assessment in advanced cancer: patient reports versus systematic assessment. Proc ASCO 20(Pt 1 of 2):1541
Ribaudo JM, Cella D, Hahn EA, Lloyd SR, Tchekmedyian NS, Von Roenn J (2000) Re-validation and shortening of the functional assessment of anorexia/cachexia therapy (FAACT) questionnaire. Qual Life Res 9(10):1137–1146
Cella DF, Von Roenn J, Lloyd S, Browder HP (1995) The Bristol-Myers anorexia/cachexia recovery instrument (BACRI): a brief assessment of patients’ subjective response to treatment for anorexia/cachexia. Qual Life Res 4(3):221–231
Thoresen L, Fjeldstad I, Krogstad K, Kaasa S, Falmer UG (2002) Nutritional status of patients with advanced cancer: the value of using the subjective global assessment of nutritional status as a screening tool. Palliat Med 16:33–42
Revicki DA, Rentz AM, Dubois D, Kahrilas P, Stanghellini V, Talley NJ (2003) Development and validation of a patient-assessed gastroparesis symptom severity measure: the Gastroparesis Cardinal Symptom index. Aliment Pharmacol Ther 18(1):141–150
Parker BA, Sturm K, MacIntosh CG, Feinle C, Horowitz M, Chapman IM (2004) Relation between food intake and visual analogue scale ratings of appetite and other sensations in healthy older and young subjects. Eur J Clin Nutr 58(2):212–218
Strubbe JH, Woods SC (2004) The timing of meals. Psych Rev 111(1):128–141
Graaf CD, Dejong LS, Lambers AC (1999) Palatability affects satiation but not satiety. Physiol Behav 66(4):681–688
De Graaf C, WAM Blom, PAM Smeets, Stafleu A, Hendriks HFJ (2004) Biomarkers of satiation and satiety. Am J Clin Nutr 79:946–961
Erkurt E, Erkisi M, Tunali C (2000) Supportive treatment in weight-losing cancer patients due to the additive adverse effects of radiation treatment and/or chemotherapy. J Exp Clin Cancer Res 19(4):431–439
de Castro JM (2004) The time of day of food intake influences overall intake in humans. J Nutr 134(1):104–111
Strubbe JH, van Dijk G (2002) The temporal organization of ingestive behavior and its interaction with regulation of energy balance. Neurosci Biobehav Rev 26(4):485–498
Beglinger C, Degen L (2002) Role of thyrotrophin releasing hormone and corticotrophin releasing factor in stress related alterations of gastrointestinal motor function. Gut 51:45–49
Cota D, Marsicano G, Tschöp M, Grübler Y, Flachskamm, Schubert M, Auer D (2003) The endogenous cannabinoid system affects energy balance via orexigenic drive and peripheral lipogenesis. J Clin Invest 112(3):423–431
Powley TL, Phillips RJ (2004) Gastric satiation is volumetric, intestinal satiation is nutritive. Physiol Behav 82:69–74
Nelson KA, Walsh D (2002) Autonomic nervous system dysfunction in advanced cancer. Support Care Cancer 10:523–528
Delgado-Aros S, Chial HJ, Cremonini F, Ferber I, McKinzie S, Burton DD (2003) Effects of asimadoline, a kappa-opioid agonist, on satiation and postprandial symptoms in health. Aliment Pharmacol Ther 18(5):507–514
Delgado-Aros S, Camilleri M (2005) Visceral hypersensitivity. J Clin Gastroenterol 39(4 Suppl S):S194–S203
Kraly FS (2004) Eating provides important physiological signals for satiety and drinking. Physiol Behav 82:49–52
Kim DY, Delgado-Aros S, Camilleri M, Samsom M, Murray JA, O’Connor MK (2001) Noninvasive measurement of gastric accommodation in patients with idiopathic nonulcer dyspepsia. Am J Gastroenterol 96(11):3099–3105
Simonian HR, Maurer AH, Knight LC, Kantor S, Kontos D, Megalooikonomou V (2004) Simultaneous assessment of gastric accommodation and emptying: studies with liquid and solid meals. J Nucl Med 45:1155–1160
Bredenoord AJ, Chial HJ, Camilleri M, Mullan BP, Murray JA (2003) Gastric accommodation and emptying in evaluation of patients with upper gastrointestinal symptoms. Clin Gastroenterol Hepatol 1(4):264–272
Tack J, Caenepeel P, Piessevaux H, Cuomo R, Janssen J (2003) Assessment of meal induced gastric accommodation by a satiety drinking test in health and in severe functional dyspepsia. Gut 52:1271–1277
Boeckxstaens GE, Hirsch DP, van den Elzen BD, Heisterkamp SH, Tytgat GN (2001) Impaired drinking capacity in patients with functional dyspepsia: relationship with proximal stomach function. Gastroenterol 121(5):1054–1063
Jones KL, Doran SM, Hveem K, Bartholomeusz FD, Morley JE, Sun WM (1997) Relation between postprandial satiation and antral area in normal subjects. Am J Clin Nutr 66(1):127–132
Sarnelli G, Sifrim D, Janssens J, Tack J (2004) Influence of sildenafil on gastric sensorimotor function in humans. Am J Physiol Gastrointest Liver Physiol 287(5):G988–G992
Hornbuckle K, Barnett JL (2000) The diagnosis and work-up of the patient with gastroparesis. J Clin Gastroenterol 30(20):117–124
Syed AA, Rattansingh A, Furtado SD (2005) Current perspectives on the management of gastroparesis. Postgrad Med 51(1):54–60
Nelson KA, Walsh TD, Sheehan FG, O’Donovan PB, Falk GW (1993) Assessment of upper gastrointestinal motility in the cancer-associated dyspepsia syndrome. J Palliat Care 9(1):27–31
Shivshanker K, Bennett RW, Haynie TP (1983) Tumor-associated gastroparesis: correction with metoclopramide. Am J Surg 145(2):221–225
Wilson J, Plourde JY, Marshall D, Yoshida S, Chow W, Harsanyi Z (2002) Long-term safety and clinical effectiveness of controlled-release metoclopramide in cancer-associated dyspepsia syndrome: a multicentre evaluation. J Palliat Care 18(2):84–91
Perkel MS, Hersh T, Moore C, Davidson ED (1980) Metoclopramide therapy in fifty-five patients with delayed gastric emptying. Am J Gastroenterol 74(3):231–236
Edholm T, Levin F, Hellström PM, Schmidt PT (2004) Ghrelin stimulates motility in the small intestine of rats through intrinsic cholinergic neurons. Regul Pept 121:25–30
Davis MP, Dreicer R, Walsh D, Lagman R, LeGrand SB (2004) Appetite and cancer-associated anorexia: a review. J Clin Oncol 22(8):1510–1517
Neary NM, Small CJ, Wren AM, Lee JL, Druce MR, Palmieri C (2004) Ghrelin increases energy intake in cancer patients impaired appetite: acute, randomized, placebo-controlled trial. J Clin Endocrinol Metab 89(6):2832–2836
Shimizu Y, Nagaya N, Isobe T, Imazu M, Okumura H, Hosoda H (2003) Increased plasma ghrelin level in lung cancer cachexia. Clin Cancer Res 9(2):774–778
Janssen JA, van der Lely AJ, Lamberts SW (2004) Is there a role of ghrelin in preventing catabolism? J Endocrinol Invest 27(4):400–403
Wren AM, Seal LJ, Cohen MA, Brynes AE, Frost GS, Murphy KG (2001) Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab 86(12):5992–5995
Flint A, Raben A, Ersboll AK, Holst JJ, Astrup A (2001) The effect of physiological levels of glucagon-like peptide-1 on appetite, gastric emptying, energy and substrate metabolism in obesity. Int J Obes Relat Metab Disord 25(6):781–792
Bray GA (2000) Afferent signals regulating food intake. Proc Nutr Soc 59(3):373–384
Blundell JE, Lawton CL, Cotton JR, Macdiarmid JI (1996) Control of human appetite: implications for the intake of dietary fat. Annu Rev Nutr 16:285–319
Author information
Authors and Affiliations
Corresponding author
Additional information
A World Health Organization demonstration project in palliative medicine.
Rights and permissions
About this article
Cite this article
Davis, M.P., Walsh, D., Lagman, R. et al. Early satiety in cancer patients: a common and important but underrecognized symptom. Support Care Cancer 14, 693–698 (2006). https://doi.org/10.1007/s00520-005-0015-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-005-0015-4