Abstract
Consecutive cancer referrals to a palliative medicine program were evaluated to assess nutritional status using a standard protocol. The study included 352 patients (180 men, 172 women; median age 61 years, range 22–94 years). The most common diagnosis was lung cancer. All had metastatic disease, 139 with gastrointestinal involvement. The most common gastrointestinal symptoms were weight loss (n=307), anorexia (n=285), and early satiety (n=243). Of those with any weight loss, 71% had lost ≥10% of their pre-illness weight. The most common factor identified which might have contributed to weight loss was hypophagia (n=275/307). Men had lost weight more often and to a greater extent than women. Triceps skinfold (TSF) was measured in 337: 51% had values that suggested severe fat deficiency. Upper mid-arm muscle area (AMA) was measured in 349: 30% had evidence of significant muscle mass reduction. The body mass index (BMI) was normal or increased in most patients. Calculated resting energy expenditure (REE) (n=324) was high in 41%. C-reactive protein was elevated in 74% of those measured (n=50). We conclude that: (1) most of this group of cancer patients referred to palliative medicine had severe weight loss; (2) there was a gender difference in the severity and type of weight loss; (3) males lost more weight overall and more muscle than females; (4) males with any degree of weight loss had a higher REE than females; (5) a significant correlation existed between the time from diagnosis to death and the severity of weight loss in the prior month; (6) BMI was normal in most patients, suggesting precancer diagnosis obesity; and (7) both TSF and AMA correlated well with body composition of both fat and protein as determined by bioelectrical impedance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malnutrition is common in cancer and adversely affects quality of life and survival. It is multifactorial involving host/tumor interactions with increased energy requirements and/or losses, despite normal or increased food intake [49, 50]. Malnutrition contributes to death in up to 80% of cancer patients [17, 38, 46, 47, 56]. Optimal nutrition may improve clinical outcomes [33, 34, 52]. Nutritional assessments identify those who need nutritional care, and help plan intervention [27, 47, 48, 49]. Successful nutritional assessment, however, requires standardization of definitions, assessment tools, criteria for nutritional intervention and appropriate end-points for outcomes [27, 48, 49, 50]. There is no agreed approach to this in cancer management.
Four types of data may help determine nutritional status [27, 33, 34, 52]:
-
1.
Dietary: appetite, weight, activity level, food habit, bowel movements, medications, food aversions, intolerance, allergies, and symptoms related to digestion.
-
2.
Physical: clinical indicators that detect nutritional deficiencies.
-
3.
Biochemical: levels of visceral proteins and other compounds in serum and urine
-
4.
Anthropometric: these quantify body compartments and are compared with values from age- and sex-matched normal populations to estimate body muscle and fat mass.
An ideal nutrition tool needs to be easy to use, cost-effective, reproducible in several clinical settings, valid, and able to predict those who need intervention [4, 16, 34, 52]. No single tool meets these criteria [4, 16].
We report a prospective evaluation of nutritional status in advanced cancer at the Palliative Medicine Program of the Cleveland Clinic Foundation. We developed an empirical nutritional assessment that included easily performed non-invasive parameters suitable for use at the bedside or in the outpatient clinic amongst patients with advanced cancer. We emphasize those assessments with high validity and practicality for cancer populations based on literature review and our clinical experience. To our knowledge, this was the first such comprehensive nutritional assessment to be conducted specifically amongst patients with advanced cancer.
Patients and methods
Between November 1998 and August 1999, consecutive patients with advanced cancer presenting to the Palliative Medicine Program of the Cleveland Clinic Foundation were evaluated for nutritional status. Evaluation took place on the palliative medicine inpatient unit, outpatient clinic and other inpatient units through our consultation service. The study protocol was approved by Cleveland Clinic Foundation Institutional Review Board (IRB). Information gathered included age, gender, primary diagnosis, and extent of disease including gastrointestinal (GI) or intraabdominal involvement. Current medication possibly affecting nutritional status such as anabolic steroid (e.g. testosterone), corticosteroids, immunotherapy (e.g. interleukins), megestrol acetate, recent chemotherapy, and radiotherapy within the last month was noted from the medical records. A standardized GI symptom questionnaire was administered by a palliative medicine physician.
Physical examination including the appearance of skin, lips, and tongue, loss of subcutaneous fat, extremity edema and ascites, body temperature, pleural effusion, weight and height were determined by a physician using a checklist (present/absent). Cheilosis (vertical cracks in center of lips with swelling), angular stomatitis (redness, cracking and flaking at the corners of the mouth), lingual papillary atrophy (smooth, pale tongue, and atrophied taste buds) and glossitis (red and painful tongue with atrophic taste buds) were sought. Ascites and pleural effusions were detected using the most recent available prior CT scan and other radiology reports. Loss of subcutaneous fat suggests cachexia.
Loss of subcutaneous fat was identified by clinical observation (clinical appearance of cachexia). Ideal body weight is the weight value recommended for a given height and age in the weight tables published by the United States government [24]. The actual body weight was measured using the hospital electronic weight scale. Patients were weighed without shoes, purse, or Foley bag. The absolute body weight was measured using bioelectrical impedance (BEI). Either ≥10% weight loss over the prior 6 months, or ≥5% over the prior month has been used to define cachexia [6, 8]. All ascites and pleural effusion were identified by the most recent available suitable tests (e.g. CT scan). Hemoglobin and serum albumin were recorded from the chart. C-reactive protein (CRP) was ordered after verbal consent from the patient but only done when there was another routine non-research laboratory blood test on the same day of assessment.
Triceps skinfold (TSF) measurement is a practical, inexpensive, and objective assessment of nutritional status. It measures subcutaneous fat and evaluates both body fat and caloric stores [2, 22, 23, 24, 25]. It was measured in the right arm, unless arm edema or paralysis was present. If possible, the patient was standing or sitting erect with bare arm and shoulder. The arm was held vertically, so as not to rest on any surface. Fat thickness at the triceps muscle is not uniform, so measurement was always at a specific point (the posterior midpoint between the acromion and olecranon process). We compared our measurements to the National Center for Health Statistics tables [1, 23, 24]. Fat depot deficiency is mild if the TSF is within the 30th to 40th percentile of the standard, moderate between the 25th to 35th percentile, and severe below the 25th percentile [2].
A direct measurement of mid-arm circumference (MAC) and calculation of bone-free mid-arm muscle area (AMA) is sensitive to body protein stores [2, 22, 23, 24, 25] and assesses muscle wasting and protein-calorie malnutrition [2, 22, 23, 24, 25]. MAC at the posterior midpoint between the acromion and olecranon process was measured by flexible nonstretch tape. The tape was held firmly but gently so there was no soft tissue compression. AMA less than the 15th percentile suggests severe muscle mass reduction [2]. AMA was calculated from the following formulas: for women [(MAC−π)×(TSF)]2/4π−6.5, and for men [(MAC−π)×(TSF)2/4π]−10 [20, 32]. We compared our results with normal values (by age and gender) [1, 23, 24].
Body mass index (BMI) was calculated from BMI=weight (kg)/height (m2) [31, 32]. BMI has been used in evaluating both cachexia and obesity [11]. The normal range proposed by the World Health Organization (WHO) is 18.5 to 24.9 kg/m2 [58]. The risk for protein-calorie malnutrition was graded as mild, moderate or severe according to BMI: mild 17.0 to 18.4 kg/m2; moderate 16.0 to 16.9 kg/m2; severe <16.0 kg/m2 [11, 29]. Resting energy expenditure (REE) was calculated using the Harris-Benedict formulas: for men REE (kcal/day)=5×(height in centimeters)+13.7×(weight in kilograms)+66−6.8×(age in years); for women REE (kcal/day)=1.85×(height in centimeters)+9.6×(weight in kilograms)+655−4.7×(age in years) [28]. REE results were compared to the normal median REE (1377 kcal/day) measured using indirect calorimetry in 12 healthy males and 5 healthy females 56±3.5 years old [57].
BEI was measured between the right wrist and right ankle using a tetrapolar electrode method [31, 41, 42]. The subject was lightly clothed without shoes or socks, supine with extended extremities. Adhesive electrodes were positioned in the middle of the dorsal surfaces of the right hand and right foot proximal to the metacarpophalangeal and metatarsophalangeal joints. A second set was placed between the distal prominence of the radius and the ulnar styloid and between the medial and lateral malleoli of the ankle. A small alternating electrical current was applied to the distal electrodes and the proximal electrode detected voltage drop [37, 51, 55]. A body composition analyzer (Preventive Medicine Technology, Beaverton, Ore.) was used to measure the total BEI score. Lean body mass, body fat, and basal metabolic rate were calculated from a computer analysis of weight, height, age, gender, and BEI. The t-test was used to compare each variable between men and women.
Results
Demographics and survival
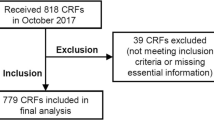
Of 451 consecutive patients screened, 99 were ineligible, resulting in a final study population of 352. Of these, 262 were seen in the palliative medicine inpatient unit, 34 in outpatient clinic and 56 in other inpatient units through our consultation service. Reasons for ineligibility were: confusion and altered mental status (n=35), actively dying (n=28), patient refusal (n=20), language barrier (n=11), and hearing or communication impairment (n=5). There were 180 men and 172 women, median age 61 years (range 22–94 years). All had metastatic cancer with the lung as the most common primary site (Table 1). The patient population was representative of the general cancer population in terms of age; cancer primary sites were similar to current cancer mortality by disease site in the United States [18]. GI or intraabdominal metastases were present in 40%, liver metastases in 26%, and intraabdominal lymphadenopathy in 11%.
Gender differences were found. Male actual body weight was greater (P=0.001), they had lower BMI (P=0.034), smaller TSF (P<0.001), greater AMA (P=0.03), greater lean body mass (P<0.001), and higher calculated REE (P<0.001). It is also noteworthy that there was a higher total BEI score in women compared to men: mean (530±106 vs 484±100; P<0.001). Survival information was available in 53%. The median survival from diagnosis to death was 16 months (range 0.5 to 470 months) and after assessment about 1 month (range 1 day to 7 months). A significant correlation existed between survival post-study and the severity of weight loss in the prior month, but not with severity of weight loss overall. There was no relationship between survival after assessment and CRP level.
History and symptoms
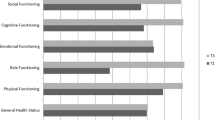
There were 16 distinct GI symptoms (Table 2). The most common were weight loss, anorexia and early satiety. The absolute number of GI symptoms correlated (r=0.8) with severity of weight loss (P=0.01; Fig. 1). Taste changes included an abnormal (e.g. metallic) taste in 16%, decreased taste in 16%, and increased taste in 7%. Decreased sense of smell was present in 10%. Diarrhea was more common in women (30%) than in men (18%; P=0.01). Men lost weight more frequently and severely than women (Fig. 2). This was true for both the 1-month and 6-month time frames.
Weight loss was more common than anorexia. In the 6 months before assessment, 87% had lost some weight, and most (71%) lost ≥10% of pre-illness weight. Of the latter most (61%) also had anorexia. Comparing males (n=161) and females (n=139) with any degree of weight loss, males showed a higher calculated REE (54% vs 24%; P=0.0001). Females had lower TSF than males (79% vs 27%; P=0.0001). Most of those with anorexia (n=285, 81%) also had either hypophagia (84%) or had lost some weight (88%; P=0.001). It is noteworthy that a significant minority (16%) of those with anorexia reported either normal food intake or hyperphagia. Nevertheless, 83% of all patients had hypophagia within both 1 month and 6 months before assessment.
Of all those studied, 47% were receiving corticosteroids (which may increase appetite) for various reasons including brain metastasis, spinal cord compression, and nausea, and 7% were on megestrol acetate. No other known appetite stimulants were being used. Within the month prior to evaluation, 24% had received chemotherapy and 28% radiation therapy. With regard to nutritional supplementation, 3% were receiving enteral nutrition (due to dysphagia from esophageal or head and neck cancer), 2% parenteral nutrition, and 1% other supplements.
Biochemical measurements and radiological investigation
Hemoglobin was measured in 106 patients. The median was 10.6 g/dl (range 6.5–22 g/dl). Most patients (72%) were anemic (hemoglobin <12 g/dl in females and <13.5 g/dl in males) [12]. Serum albumin was measured in 103 patients. The median was 3.2 g/dl (range 1.6–4.8 g/dl). The majority of patients (66%) were hypoalbuminemic (normal 3.5–5 g/dl) [12]. CRP was measured in a subgroup of 50 patients, of whom 74% had a high CRP (median 5.1 mg/dl, range 0.3–29 mg/dl; normal 0–2 mg/dl). A low serum albumin was found in 92% of those with elevated CRP compared to 11% with normal CRP (P=0.0001).
Physical examination and anthropometric measurements
Physical signs suggestive of nutritional deficiency were common (Table 3). The median/range (kilograms) of lean body mass, body fat, and absolute body weight were 51.3 (9.9–92.4), 12.4 (1–57), and 65 (33–182), respectively, calculated individually by BEI (n=329). The proportion of those with fat loss increased with greater weight loss. Of those with ≥10% weight loss during the prior 6 months, males lost more muscle mass than fat. Females lost both muscle mass and fat. Patients with clinical cachexia were significantly different from those without (Table 4). The former had more abdominal metastasis, hypophagia, and anorexia. They had also lost more weight, fat, and muscle compared to non-cachectic patients. There were also gender differences amongst those with clinical cachexia. Males lost less fat and had a higher REE than females (Table 5). Of all patients, 48% were judged to be clinically cachectic, and nearly all (95%) of those had anorexia. Peripheral edema was common (31%), and was more frequent in women than men (P=0.03).
BMI was calculated in 346 patients. The median was 23.6 kg/m2 (range 12–54 kg/m2). BMI was normal or high in 87%. Amongst those with either normal or high BMI, 11% had AMA values consistent with severe muscle mass reduction (P=0.0001; r=0.4). AMA was calculated in 349 patients. The median was 32.6 cm2 (range 11.3–117.9 cm2). Severe muscle mass reduction was seen in 30%, and in 78% of these BMI was either normal or increased. TSF thickness was measured in 337 patients. The median was 1.1 cm (range 0.06–2.1 cm). There was evidence of severe fat storage deficiency in 51%, and paradoxically amongst these BMI again was usually (86%) either normal or increased. REE was calculated in 324 patients. The median was 1350 kcal/day (range 872–2415 kcal/day). A REE greater than 1377 kcal/day, suggesting a high basal metabolic rate, was seen in 41%.
Discussion
Symptoms and malnutrition
The distribution of primary sites in our study was similar to that in data on current cancer mortality by disease site in the United States. GI symptoms were common [17, 35], even without intraabdominal carcinomatosis or GI metastasis. The absolute number of GI symptoms correlated with weight loss severity. Evidence of vitamin and nutritional deficiencies were common. Survival correlated with the severity of weight loss during the previous month. Survival information was not available in most. This was due to death in a hospice other than the Cleveland Clinic, in a state other than Ohio, or of non-hospice patients at home. Many cancer patients seem to die with a normal ideal weight despite significant weight loss. Radiation, chemotherapy, nausea, dysphagia, diarrhea, and constipation may contribute to malnutrition [6, 26] in addition to the cancer.
Anorexia and cachexia
The term cachexia is derived from the Greek kakos (bad) and hexis (condition). It was reported in 1932 as an important cause of death in advanced cancer [1, 56]. Cachexia may develop in different diseases (cancer, congestive heart failure, etc.). Proinflammatory cytokines are important etiologies [14, 15, 21]. The definition is controversial. Either tissue loss or ≥10% weight loss during a 6-month period has been used [7, 45]. Amongst those in our study judged to be clinically cachectic, anorexia was nearly universal, but anorexia was not necessarily accompanied by reduced food intake (hypophagia). Even amongst those with severe weight loss, anorexia was not always present, suggesting perhaps a different pathophysiology. In our study, some patients with anorexia had either normal food intake or hyperphagia. Anorexia may not be the cause of cachexia. The term "anorexia-cachexia syndrome" may therefore be misleading. Some believe cachexia is due to a sequence of anorexia, hypophagia, and starvation. This may be incorrect. Total parenteral nutrition does not reverse cachexia [3, 9, 33]. Starvation initially only causes fat loss, while cachexia is associated with both fat and muscle loss [10, 54].
Cachexia and weight loss
Weight loss is known to negatively affect both quality of life and survival [3, 4, 39]. Despite significant weight loss, most of our cancer patients seemed to die with a normal ideal body weight. This appeared to be due to precancer diagnosis obesity. Weight loss alone is therefore insufficient to define cachexia [36, 26]. Obesity appears to be a significant risk factor for developing cancer or perhaps itself is a poor prognostic indicator in those who develop cancer.
Cachexia
Clinical cachexia seemed to be the best representative of the anorexia-cachexia syndrome. In our study, there was a high frequency of anorexia, constipation, and hypophagia amongst those who were clinically cachectic. Moreover, clinical cachexia was an important predictor of severe weight loss. Strong relationships existed between clinical cachexia and abnormalities in TSF and AMA. However, significant weight loss existed amongst those without clinical cachexia. Our data showed two different gender-related catabolic changes. Females lost equal amounts of muscle mass and fat while males lost more muscle mass. In advanced cirrhosis, males have been reported to lose more muscle mass and females more fat [40, 43]. In advanced cancer, some have reported muscle loss only, others both fat and muscle loss [13, 14, 30]. A significant correlation has been previously reported between TSF and weight loss amongst cancer patients [13]. This was also true in our study. TSF abnormalities have also been reported to predict mortality [44], but we did not find a correlation (however, our survival data were incomplete).
CRP, REE, and malnutrition
Increased REE [5, 59] may be responsible for cancer-associated weight loss. Males lost weight more frequently and severely than females especially from muscle wasting. It is noteworthy that males with any degree of weight loss had a higher REE than females. Increased CRP was highly correlated with decreased albumin but not with degree of weight loss or survival. In a previous study, CRP and REE have been found to be correlated in patients with advanced lung cancer [19, 53]. We did not observe this. However, our laboratory data for albumin and CRP were incomplete and therefore may not have reflected the entire group. There was no correlation between REE and AMA, TSF, or MAC.
Bioelectrical impedance
AMA, TSF, and both body fat and muscle mass, as measured by BEI, were correlated with clinical cachexia. Although there was a difference in the BEI score between men and women, we have no evidence that the BEI score alone has any validity. High female body fat content might have caused the low BEI scores [1]. We consider clinical cachexia, AMA, TSF, and BEI of body fat and muscle mass together (but not weight loss alone) therefore best to evaluate nutritional status. AMA and TSF do not appear to add any additional information to BEI used alone. We consider BEI as an additional easy method to assess cachexia [36].
Future research
Clinical trials in cachexia need to incorporate laboratory and anthropometric measurements with quality of life and prognostic instruments. Universally applicable diagnostic criteria for cachexia need to be developed. BEI should be incorporated in all therapeutic trials in cachexia to evaluate the body composition response to the studied drug.
Conclusions
-
1.
Most patients had severe weight loss. BMI was normal in most. Most had normal actual weight despite significant post-illness weight loss suggesting pre-illness obesity. Men lost weight more frequently and severely than women.
-
2.
Major differences in anthropometrics were found between males and females. Females lost equal amounts of both fat and protein, while males lost more protein. Males with any degree of weight loss had a higher REE than females.
-
3.
Neither anorexia nor weight loss alone were sufficient to define cachexia. Clinical cachexia seemed to be the best representative of the anorexia-cachexia syndrome. The absolute number of GI symptoms correlated with severity of weight loss. GI symptoms, particularly anorexia and weight loss, were frequent. A significant minority of patients with anorexia reported either normal or increased food intake. Physical signs of nutritional deficiency were common.
-
4.
A significant correlation existed between the time from diagnosis to death and weight loss in the prior month.
-
5.
No single measurement is adequate to evaluate nutrition or protein-energy malnutrition. There was evidence of cachexia by BEI, AMA, and TSF despite normal or high BMI. AMA and TSF do not appear to add further information to BEI used alone. BEI is a non-invasive and simple test of body composition and nutritional status in advanced disease and can be used as an alternative to TSF and AMA. Serum CRP was often abnormal and correlated with decreased serum albumin but not with severity of weight loss. Anemia and hypoalbuminemia were common.
References
Abraham S, Carroll MD, Najjar MF, Fulwood R (1983) Obese and overweight adults in the United States. Vital Health Stat 11:1–93
Alpers DH, Stenson WF, Bier DM (1995) Protein and calories requirements, intake and assessment. In: Apers DH, Stenson WF, Bier DM (eds) Manual of nutrition therapy. Little, Brown and Company, Boston, MA, pp 73–114
Baker JP, Detsky AS, Wesson DE, et al (1982) Nutritional assessment: a comparison of clinical judgement and objective measurements. N Engl J Med 306:969–972
Baker JP, Detsky AS, Whitwell J, Langer B, Jeejeebhoy KN (1982) A comparison of the predictive value of nutritional assessment techniques. Hum Nutr Clin Nutr 36:233–241
Baumann H, Gauldie J (1994) The acute phase response [see comments]. Immunol Today 15:74–80
Berry JK, Braunschweig CA (1998) Nutritional assessment of the critically ill patient. Crit Care Nurs Q 21:33–46
Blackburn G (1998) Wasting away: cancer cachexia. Health News 4:4
Blackburn GL, Bistrian BR, Maini BS, Schlamm HT, Smith MF (1977) Nutritional and metabolic assessment of the hospitalized patient. JPEN J Parenter Enteral Nutr 1:11–22
Bowman BB, Rosenberg IH (1982) Assessment of the nutritional status of the elderly. Am J Clin Nutr 35:1142–1151
Brennan MF (1977) Uncomplicated starvation versus cancer cachexia. Cancer Res 37:2359–2364
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr (1999) Body-mass index and mortality in a prospective cohort of U.S. adults [see comments]. N Engl J Med 341:1097–1105
Cleveland Clinic Foundation (1999) Guide to laboratory services. Pathology and Laboratory Medicine. The Cleveland Clinic Foundation, Cleveland, OH
Cohn SH, Gartenhaus W, Sawitsky A, et al (1981) Compartmental body composition of cancer patients by measurement of total body nitrogen, potassium, and water. Metabolism 30:222–229
Cohn SH, Gartenhaus W, Vartsky D, et al (1981) Body composition and dietary intake in neoplastic disease. Am J Clin Nutr 34:1997–2004
Delmore G (1997) Assessment of nutritional status in cancer patients: widely neglected? Support Care Cancer 5:376–380
Detsky AS, Baker JP, Mendelson RA, Wolman SL, Wesson DE, Jeejeebhoy KN (1984) Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: methodology and comparisons. JPEN J Parenter Enteral Nutr 8:153–159
Donnelly S, Walsh D, Rybicki L (1995) The symptoms of advanced cancer: identification of clinical and research priorities by assessment of prevalence and severity. J Palliat Care 11:27–32
Edwards BK, Howe HL, Ries LA, et al (2002) Annual report to the nation on the status of cancer, 1973–1999, featuring implications of age and aging on U.S. cancer burden. Cancer 94:2766–2792
Falconer JS, Fearon KC, Plester CE, Ross JA, Carter DC (1994) Cytokines, the acute-phase response, and resting energy expenditure in cachectic patients with pancreatic cancer. Ann Surg 219:325–331
Forbes GB, Brown MR, Griffiths HJ (1988) Arm muscle plus bone area: anthropometry and CAT scan compared. Am J Clin Nutr 47:929–931
Freeman LM, Roubenoff R (1994) The nutrition implications of cardiac cachexia. Nutr Rev 52:340–347
Frisancho AR (1974) Triceps skin fold and upper arm muscle size norms for assessment of nutrition status. Am J Clin Nutr 27:1052–1058
Frisancho AR (1981) New norms of upper limb fat and muscle areas for assessment of nutritional status. Am J Clin Nutr 34:2540–2545
Frisancho AR (1984) New standards of weight and body composition by frame size and height for assessment of nutritional status of adults and the elderly. Am J Clin Nutr 40:808–819
Frisancho AR (1988) Nutritional anthropometry. J Am Diet Assoc 88:553–555
Goodinson SM (1987) Assessment of nutritional status. Prof Nurse 2:367–369
Goulet O (1998) Assessment of nutritional status in clinical practice. Baillieres Clin Gastroenterol 12:647–669
Harris J, Benedict F (1919) A biometric study of basal metabolism in man. Carnegie Institute of Washington, Washington, DC
Heiat A, Vaccarino V, Krumholz HM (2001) An evidence-based assessment of federal guidelines for overweight and obesity as they apply to elderly persons. Arch Intern Med 161:1194–1203
Heymsfield SB, McManus CB (1985) Tissue components of weight loss in cancer patients. A new method of study and preliminary observations. Cancer 55:238–249
Heymsfield SB, McManus C, Smith J, Stevens V, Nixon DW (1982) Anthropometric measurement of muscle mass: revised equations for calculating bone-free arm muscle area. Am J Clin Nutr 36:680–690
Hirsch S, de Obaldia N, Petermann M, et al (1991) Subjective global assessment of nutritional status: further validation. Nutrition 7:35–37
Jeejeebhoy KN, Meguid MM (1986) Assessment of nutritional status in the oncologic patient. Surg Clin North Am 66:1077–1090
Jeejeebhoy KN, Detsky AS, Baker JP (1990) Assessment of nutritional status. JPEN J Parenter Enteral Nutr 14:193S–196S
Komurcu S, Nelson K, Walsh D, Ford R, Rybicki L (2002) Gastrointestinal symptoms amongst inpatients with advanced cancer. Am J Hosp Palliat Care 19:351–355
Kotler DP (2000) Cachexia. Ann Intern Med 133:622–634
Kushner RF (1992) Bioelectrical impedance analysis: a review of principles and applications. J Am Coll Nutr 11:199–209
Lawson DH, Richmond A, Nixon DW, Rudman D (1982) Metabolic approaches to cancer cachexia. Annu Rev Nutr 2:277–301
Lipkin EW, Bell S (1993) Assessment of nutritional status. The clinician's perspective. Clin Lab Med 13:329–352
Lolli R, Marchesini G, Bianchi G, et al (1992) Anthropometric assessment of the nutritional status of patients with liver cirrhosis in an Italian population. Ital J Gastroenterol 24:429–435
Lukaski HC (1987) Methods for the assessment of human body composition: traditional and new. Am J Clin Nutr 46:537–556
Lukaski HC, Bolonchuk WW, Hall CB, Siders WA (1986) Validation of tetrapolar bioelectrical impedance method to assess human body composition. J Appl Physiol 60:1327–1332
Merli M, Riggio O, Romiti A, et al (1990) Basal energy production rate and substrate use in stable cirrhotic patients. Hepatology 12:106–112
Mullen JL, Gertner MH, Buzby GP, Goodhart GL, Rosato EF (1979) Implications of malnutrition in the surgical patient. Arch Surg 114:121–125
Neale G (1990) Undernutrition. Med Int 82:3386–3391
Nelson KA (2000) The cancer anorexia-cachexia syndrome. Semin Oncol 27:64–68
Nelson KA, Walsh D, Sheehan FA (1994). The cancer anorexia-cachexia syndrome [see comments]. J Clin Oncol 12:213–225
Ottery FD (1994) Rethinking nutritional support of the cancer patient: the new field of nutritional oncology. Semin Oncol 21:770–778
Ottery FD (1995) Supportive nutrition to prevent cachexia and improve quality of life. Semin Oncol 22:98–111
Ottery FD (1996) Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition 12:S15–S19
Paijmans IJ, Wilmore KM, Wilmore JH (1992) Use of skinfolds and bioelectrical impedance for body composition assessment after weight reduction. J Am Coll Nutr 11:145–151
Smith LC, Mullen JL (1991) Nutritional assessment and indications for nutritional support. Surg Clin North Am 71:449–457
Staal-van den Brekel AJ, Schols AM, ten Velde GP, Buurman WA, Wouters EF (1994) Analysis of the energy balance in lung cancer patients 1. Cancer Res 54:6430–6433
Tisdale MJ (2001) Cancer anorexia and cachexia. Nutrition 17:438–442
Van Loan M, Mayclin P (1987) Bioelectrical impedance analysis: is it a reliable estimator of lean body mass and total body water. Hum Biol 59:299–309
Warren S (1932) The immediate causes of death in cancer. Am J Med Sci 184:610–615
Wigmore SJ, Falconer JS, Plester CE, et al (1995) Ibuprofen reduces energy expenditure and acute-phase protein production compared with placebo in pancreatic cancer patients. Br J Cancer 72:185–188
World Health Organization (2000) Obesity: preventing and managing the global epidemic (Technical Report Series, no. 894). WHO, Geneva
Xing Z, Gauldie J, Cox G, et al (1998) IL-6 is an anti-inflammatory cytokine required for controlling local or systemic acute inflammatory responses. J Clin Invest 101:311–320
Author information
Authors and Affiliations
Corresponding author
Additional information
The Harry R. Horvitz Center for Palliative Medicine is a World Health Organization Demonstration Project in Palliative Medicine.
This work was presented at the American Society of Clinical Oncology 35th Annual Meeting in Atlanta, Georgia, May 15–18, 1999.
Rights and permissions
About this article
Cite this article
Sarhill, N., Mahmoud, F., Walsh, D. et al. Evaluation of nutritional status in advanced metastatic cancer. Support Care Cancer 11, 652–659 (2003). https://doi.org/10.1007/s00520-003-0486-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-003-0486-0