Abstract
Goals of work
To study outcome and its predictive factors in cancer patients admitted to the ICU with septic shock, and the implications of neutropenia as a risk factor in this advanced stage of systemic inflammatory response.
Patients and methods
A prospective consecutive observational cohort study was conducted in 73 adults with cancer and septic shock admitted to the ICU at the Cancer Medical Center associated with the University of Buenos Aires.
Main results
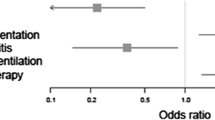
The mortality rate from septic shock was 53.4% (95%CI 41.9 to 64.8%). The mean Acute Physiology and Chronic Health Evaluation (APACHE) II score on admission, the mean number of organ dysfunctions on admission or during the ICU stay, liver dysfunction, respiratory dysfunction, and the need for mechanical ventilation were predictive of mortality in a univariate analysis. Neutropenia was not associated with a worse prognosis in terms of mortality (56%) or mean days of ICU stay (6.64 days) in comparison with nonneutropenic patients (52.1% and 6.8 days) in the univariate analysis. In the logistic regression model only the need for mechanical ventilation and liver dysfunction remained independent predictors of mortality.
Conclusions
Septic shock among cancer patients admitted to the ICU has a mortality rate similar to that reported for mixed populations, and it is particularly increased when hepatic or respiratory dysfunction develop. Neutropenia on admission does not seem to modify outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The admission of cancer patients to an intensive care unit (ICU) involves immense resources and an extraordinary degree of distress for the patient, with frequently discouraging outcomes [8, 13, 28]. In this regard, prognosis information is critical, albeit still limited [28]. Septic shock is a severe consequence of infection with a mortality rate in mixed ICU populations ranging from 46% to 61% [20, 24]. Reports concerning the evolution of critically ill cancer patients admitted to the ICU [1, 10, 13, 16, 19, 26, 28] include a wide range of causes for admission other than septic shock. Overall mortality rates ranging from 38% to more than 80% have been reported depending on the series [10, 13, 14, 16, 19, 26, 28], and these rise to 70% [19] or 87% [28] when shock is analyzed. In these studies, however, there were many reasons for ICU admission, septic shock was not defined according to ACCP/SCCM criteria [20], or the designs did not allow conclusions to be drawn about prognostic factors specifically associated with this severest stage of systemic inflammatory response syndrome (SIRS). There have been, to our knowledge, no studies specifically centered on septic shock and its prognostic factors among cancer patients.
Of the many possible risk factors in cancer patients with septic shock, neutropenia warrants special attention. Neutrophils play a critical role in the acute inflammatory response and host defense against bacterial infections [7], and the neutrophil seems to be a key cell in SIRS production. Septic shock, on the other hand, is considered to be the severest form of SIRS, and neutrophils are suggested to play a critical role in its pathogenesis [2]. Neutropenia is common in cancer patients, predisposing patients to severe infections and death [7], and its combination with ICU admission has long been considered ominous [3, 8]. It is intuitive to expect that severe diminution of the neutrophil population would result in a different systemic response to an infectious insult [5]. The data available at present, however, point to the similarities of the profiles of inflammatory mediators in septic patients with and without neutropenia [12, 21]. In contrast, clinical descriptions of the manifestations of SIRS among neutropenic patients with cancer are scarce and controversial [15, 22, 25]. Some studies have focused on neutropenic critically ill cancer patients [3, 4, 8, 11, 15, 22, 25], but they do not clarify whether there are additional implications for neutropenia when septic shock ensues, and there is no consistent view as to its repercussions on overall ICU survival [14, 28]. As the main cause of neutropenia is cancer, which could also modify shock evolution, we considered this an appropriate population to explore the implications of neutropenia in septic shock.
On this basis, we investigated outcome and its predictive factors in cancer patients admitted to the ICU with septic shock, and secondarily we centered on the implications of neutropenia as a risk factor in this advanced stage of systemic inflammatory response.
Materials and methods
All cancer patients admitted with septic shock to the ICU of the Instituto Alexander Fleming, an oncologic center affiliated to the University of Buenos Aires, between May 1994 and June 1999, were prospectively included. All patients were ≥16 years old, with active malignant neoplasm defined as a positive histologic diagnosis with at least one of the following: metastasis, ongoing or recent chemotherapy, or surgical oncologic therapy or radiotherapy prior to or during admission. All patients had to have been admitted to the ICU with a primary diagnosis of septic shock. The institutional review board approved the protocol. The study was observational and did not represent a risk for patients, so informed consent was not required. In the institution all cancer patients are eligible for ICU admission unless an explicit directive states otherwise.
The following data were collected as possible explanatory variables: demographic characteristics, type of tumor, Acute Physiology and Chronic Health Evaluation (APACHE) II score on admission, presence of neutropenia (neutrophil count in peripheral blood <1000/mm3) while in the ICU, need for mechanical ventilation, and the number of organ dysfunctions (hepatic, hematologic, renal, respiratory, neurologic, and cardiovascular). Need for mechanical ventilation was considered dichotomously as any assistance to the respiratory muscles, with or without an endotracheal tube and the day of implementation. The outcome variable was ICU mortality.
Septic shock was defined according to ACCP/SCCM criteria [20]. According to the criteria of Marshall et al. [18], the following organ dysfunctions were recorded and considered dichotomously: liver dysfunction (bilirubin >20 μmol/l), renal failure (creatinine >100 μmol/l), respiratory dysfunction (PaO2/FIO2 <300), cardiovascular failure (product of heart rate and the ratio of the central venous pressure to the mean arterial pressure >10.0), neurologic dysfunction (Glasgow coma scale <15), and hematologic dysfunction (platelet count <120,000/mm3). Malignancies were grouped as: leukemia, lymphoma, and solid tumor. Standard therapy for treating septic shock in this population was to institute broad-spectrum antibiotics against gram-negative bacilli, to add vancomycin when suitable, and to give standard hemodynamic and respiratory support. Supportive treatment is not withdrawn on the basis of terminally ill considerations.
The initial analysis included all possibly explanatory variables. For univariate comparisons, the t-test and chi-square test, with Fisher’s exact correction when necessary, were performed. Means and proportions are expressed with 95% confidence interval (95% CI). All P values are two-tailed and considered significant if <0.05.
To investigate the association between possible predictors and death, a stepwise backwards logistic regression model was adjusted by including the variables found to be significant at P<0.2 by univariate analysis as explanatory, and ICU mortality as outcome. These variables were included in a complete model, from which nonsignificant variables were progressively eliminated in order to obtain the most parsimonious model with the best overall predictive power. Analysis was performed with STATISTIX 7.0, Analytical Software, and SPSS 10.0 for Windows.
Results
The characteristics of all 73 included patients are shown in Table 1. ICU mortality rate for septic shock in the cancer patients was 53.4% (95%CI 41.9% to 64.8%). Sources of infection were: not apparent in 25 patients, respiratory in 20, abdominal in 9, cutaneous in 8, urinary in 5, and central catheter in 3 patients. There were two patients with infectious diarrhea and one with purulent pericarditis.
In the univariate analysis mortality predictors were mean APACHE II score on admission, mean number of organ dysfunctions present on admission or during the ICU stay, liver dysfunction, respiratory dysfunction, negative blood cultures and need for mechanical ventilation (Tables 2 and 3). Overall, the 25 neutropenic patients were younger, were more frequently females, and more frequently showed hepatic and, as expected, hematologic dysfunction than their nonneutropenic counterparts; both populations were otherwise similar with respect to the other studied variables. Neutropenia was not associated with a worse prognosis (Table 4) in terms of mortality or length of ICU stay. At the time of admission, 72% of the patients (18/25) had severe neutropenia (PMN less than 100/mm3), 72% of the survivors (8/11) and 71.4% of the nonsurvivors (10/14). Mean neutrophil count at the end of follow-up was not different between survivors (3075.0/mm3) and nonsurvivors (2477.3/mm3) among patients who had been admitted with neutropenia (P=0.8).
In the logistic regression model, the need for mechanical ventilation and hepatic failure were identified as independent predictors of mortality, length of ICU stay being at the limit of statistical significance (Table 5).
Blood cultures were collected from all patients on admission and during hospitalization when required by the attending physicians. Cultures were positive in 20 patients (27.4%). The predominant group of microorganisms in blood cultures was gram-positive cocci, and the commonest isolated pathogen was methicillin-resistant Staphylococcus aureus (Table 6).
Despite high mortality among patients with leukemia (11/15; 73.3%) in comparison to those with lymphoma (9/17; 52.9%) or solid tumors (19/41; 46.3%), we were unable to show a statistically significant difference between groups (chi-squared, P=0.2), as was the case when comparing the APACHE II scores and the mean number of organ dysfunctions between tumor type groups (data not shown).
Discussion
The ICU mortality for oncologic patients with septic shock was 53.4%, not too different from that reported for mixed populations. Previously reported overall ICU mortality rates for cancer patients range from approximately 38% to 59% in populations with different malignancies and reasons for ICU admission [1, 3, 13, 19, 23, 28], to 80% in some series of patients with hematologic malignancy and the need for mechanical ventilation [16, 26]. Staudinger et al. [28] reported a 53% ICU survival among cancer patients admitted for different reasons that rose to 87% when septic shock ensued. However, in contrast to the conditions of our study, this was septic shock developing during the ICU stay following admission for other reasons. Azoulay et al. [1] in 120 consecutive patients with solid cancer admitted to the medical ICU found a 58.7% overall 30-day mortality rate, and a 69% mortality among 37 patients with septic shock. Septic shock mortality in other studies was not reported [10, 13, 16, 19, 26], and others, in addition, were centered exclusively in neutropenic populations [3, 8] or bone marrow transplant recipients [23], rendering comparison unfeasible.
In our study, the type of tumor was not predictive of mortality. Similar results were obtained in two previous series of critically ill cancer patients [13, 28]. Site or stage of disease have also been found not to affect mortality when only solid tumors were included [1] or neutropenia was present [3]. Conversely, some of the above-cited studies showed higher mortality rates among patients with hematologic malignancies. Probably the largest is the study of Groeger et al. [10] where patients with leukemia/bone marrow transplantation, lymphoma/myeloma, and solid tumor had mortality rates of 57.1%, 43.5%, and 33.2%, respectively. Septic shock mortality was not reported. Age was not an independent predictor of a worse prognosis, as has been found by others [1, 28]. In this regard, however, it must be taken into account that a selection bias probably existed, because age modifies eligibility for some cancer therapies.
Neutropenic septic shock is of particular interest. It is intuitive to expect that severe diminution of the neutrophil population would result in a different systemic response to an infectious insult [5]. In the present study neutropenia was not associated with higher mortality, even when most of the patients were suffering from severe neutropenia at the time of admission. Some authors [13] have found neutropenic patients to have similar mortality rates to nonneutropenic patients (approximately 40%); however, in contrast to our study, they included other reasons for ICU admissions than septic shock. In another study [10], it was found, in agreement with our results, that the absolute neutrophil count was not associated with prognosis. Darmon et al. [8], in a retrospective cohort of 102 neutropenic patients admitted to the ICU, found mortality to be worsened if acute respiratory or renal failure ensued, but their design did not allow evaluation of the implications of neutropenia on septic shock outcome. On the other hand, in their series, shock was not an independent predictor of death. In a series of patients with hematologic malignancies admitted to the ICU for many reasons [14], neutropenia, again, was not associated with overall ICU mortality. In other studies [1, 28], neutropenia was not found to be a predictor of mortality in cancer patients admitted to the ICU for any cause, regardless of type of tumor. Even though we did not analyze the duration of neutropenia while patients were in the ICU, which weakens our conclusion, our conclusion is supported by the fact that most of the patients were admitted with severe neutropenia and the lack of difference in PMN counts at the end of the ICU stay between (previously neutropenic) survivors and nonsurvivors.
Previous reports on the prognosis for neutropenic patients with septic shock have not specifically evaluated septic shock [3, 4, 8]. Thus, the present findings could be valuable in the debate about the rationale of care in these seriously ill patients [26] and strengthens the point of view that septic shock could be a relatively autonomous pathophysiologic process. Furthermore, the present findings have to be considered when the clinical relevance of experimental data concerning the role of neutrophils in the pathogenesis of septic shock are discussed. It is noteworthy that some basic studies found similar profiles of inflammatory mediators in septic patients independently of whether they had neutropenia or not [5]. Inflammation-mediated processes such as SIRS [25] and the ARDS [15, 22] also occur in neutropenic patients. Our results, therefore, strengthen those partial descriptions, in showing a similar clinical evolution of septic shock in terms of mortality and number of organ failures, despite a low white cell count. While qualitative changes in neutrophils are not studied, at present only cell number is considered to be the most important clinical parameter [7]. In addition, the mean cell count was so small that functional aspects were unlikely to be of relevance.
As previously reported [13], mortality was especially increased among patients with hepatic or respiratory dysfunction. Once more, it is interesting to compare neutropenic and nonneutropenic patients. Hepatic failure appears to be particularly ominous [3] and neutrophils have been proposed to be the major responsible cell type in septic liver damage [9]. Nevertheless, hepatic failure occurred in the present series in the presence of very low neutrophil counts; indeed, liver compromise was higher in neutropenic than in nonneutropenic cancer patients with septic shock (Table 4). Although noncontrolled factors such as primary tumor extension or treatment-derived toxicity could have accelerated the development of hepatic failure, the results indicate doubt as to whether neutrophils contribute to septic organ failure in patients with cancer. Thus, this view is similar to the doubt that has emerged concerning the occurrence of ARDS in neutropenic patients [15].
Respiratory failure has been reported to adversely affect outcome in critically ill cancer patients [6, 28], especially when mechanical ventilation is needed [1] and the patient suffers from a hematologic malignancy [19]. However, given the fact that the need for mechanical ventilation was not studied as a time-dependent variable, the results should be interpreted with caution.
We did not observe a relationship between the number of organ dysfunctions on admission and the mortality rate, similar to the findings of other studies [6]. The APACHE II score was equally unrelated to mortality in the multivariate analysis. The APACHE II score on admission was not analyzed by some authors [6, 13], and has been found to be inaccurate in predicting mortality by others [19, 27, 28]. Some authors argue that daily variation in organ failures should be used instead of admission scores as a more powerful predictor of outcome [19].
Interestingly a positive blood culture during the ICU stay was an independent predictor of survival in the univariate analysis, and remained near statistical significance in the logistic regression model. Somewhat coincident with this result, in another study [16] identification of an organism did not affect prognosis. However, findings of other studies among critically ill patients indicate that the prognostic value of a positive blood culture is controversial [17].
Several limitations of our study must be taken into account. First, we are aware that the sample was not large enough to make a definitive negative conclusion about the impact of neutropenia on septic shock. However, these preliminary results suggest some interesting clinical as well as pathophysiologic hypotheses that deserve further study. Second, the study was performed at a single institution; thus, selection bias regarding ICU admission policy or do-not-resuscitate orders cannot be excluded. Third, hematologic malignancies and solid tumors were pooled. We acknowledge that this may render the analysis confusing, but as it has been stated above, many studies have shown no difference between these tumor type groups. In fact, the prognosis for patients with hematologic malignancies cannot be predicted by the severity of the underlying oncologic disease; rather, it depends upon the degree of acute organ dysfunction [19]. Fourth, we did not include information about cancer disease stage in the analysis. This surely influences many decisions prior to ICU admission, and thus it is a factor difficult to control for any study in this field. Another weakness was the lack of a long-term follow-up. Nevertheless, ICU mortality is an accepted end-point. Finally, it can be argued that the duration of neutropenia was not analyzed. ICU neutropenia duration has been found not to influence outcome [8], and in our study neutrophil count at the time of ICU discharge was not different between survivors and nonsurvivors.
Nevertheless, our results have a number of clinical implications. First, they show that mortality of cancer patients admitted to the ICU with septic shock is high but comparable to that in mixed populations, and is not influenced by tumor type or the presence of neutropenia. In consequence, we believe that there is no apparent support for the reluctance to admit cancer patients with septic shock to the ICU even in the presence of neutropenia or advanced age and regardless of the type of tumor. Furthermore, and in agreement with other authors [28], we think that scoring systems are not accurate enough at present to support decisions about nonutilization of expensive treatments, even in such an extreme situation as cancer with septic shock.
In summary, cancer patients admitted to the ICU with septic shock have a mortality rate close to that reported in mixed populations, and is specifically increased when hepatic or respiratory dysfunction develops. Neutropenia, type of tumor, or other organ failures on admission do not appear to modify septic shock outcome. It is therefore believed that the rationale for critical care in patients with cancer and septic shock should not be based on the type of cancer or neutrophil count on admission, and that further studies are needed to elucidate the real place of neutrophils in the evolution of septic shock.
References
Azoulay E, Moreau D, Alberti C, et al (2000) Predictors of short-term mortality in critically ill patients with solid malignancies. Intensive Care Med 26:1817–1823
Bellingan G (2000) Leukocytes: friend or foe. Intensive Care Med [Suppl] 26:s111–s118
Blot F, Guiguet M, Nitenberg G, et al (1997) Prognostic factors for neutropenic patients in an intensive care unit: respective roles of underlying malignancies and acute organ failures. Eur J Cancer 33:1031–1037
Blot F, Cordonier C, Nitenberg G, et al (2001) Severity of illness scores: are they useful in febrile neutropenic adult patients in hematology wards? Crit Care Med 29:2125–2131
Bogolioubov A, Keefe DL, Groeger JS (2001) Circulatory shock. Crit Care Clin 17:697–719
Boussat S, El’rini T, Dubiez A, et al (2000) Predictive factors of death in primary lung cancer patients on admission to the intensive care unit. Intensive Care Med 26:1811–1816
Boxer L, Dale DC (2003) Neutropenia: causes and consequences. Semin Hematol 39:75–81
Darmon M, Azoulay E, Alberti C, et al (2002) Impact of neutropenia duration on short-term mortality in neutropenic critically ill cancer patients. Intensive Care Med 28:1775–1780
Dhainaut JF, Marin N, Mignon A, et al (2000) Hepatic response to sepsis: interaction between coagulation and inflammatory processes. Crit Care Med [Suppl] 29:s42–s47
Groeger JS, Lemeyow S, Price K, Nierman DM, et al (1998) Multicenter outcome study of cancer patients admitted to the intensive care unit: a probability of mortality model. J Clin Oncol 16:761–770
Guiguet M, Blot F, Escudier B, Antoun S, Leclercq B, Nitenberg G (1998) Severity-of-illness scores for neutropenic cancer patients in an intensive care unit: which is the best predictor? Do multiple assessment times improve the predictive value? Crit Care Med 26:488–493
Haj MA, Neilly IJ, Robbie LA, et al (1995) Influence of white blood cells on the fibrinolytic response to sepsis: studies of septic patients with or without severe leucopenia. Br J Haematol 90:541–547
Kress JP, Christenson J, Pohlman AS, et al (1999) Outcomes of critically ill cancer patients in a university hospital setting. Am J Respir Crit Care Med 160:1957–1961
Kroschinsky FK, Weise M, Illmer T, et al (2002) Outcome and prognostic features of intensive care unit treatment in patients with hematologic malignancies. Intensive Care Med 28:1294–1300
Laufe MD, Simon RH, Flint A, et al (1986) Adult respiratory distress syndrome in neutropenic patients. Am J Med 80:1022–1026
Lloyd-Thomas AR, Wright I, Lister TA, et al (1988) Prognosis of patients receiving intensive care for life threatening medical complications of haematologic malignancy. BMJ 296:1025–1029
Luna CM, Videla A, Mattera J, et al (1999) Blood cultures have limited value in predicting severity of illness and as a diagnostic tool in ventilator-associated pneumonia. Chest 116:1075–1084
Marshall JC, Cook DJ, Christou NV, et al (1995) Multiple organ dysfunction score: a reliable descriptor of a complex clinical outcome. Crit Care Med 23:1638–1652
Massion PB, Dive AM, Doyen C, et al (2002) Prognosis of hematologic malignancies does not predict intensive care unit mortality. Crit Care Med 30:2260–2270
Muckart DJJ, Bhagwanjee S (1997) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definitions of the systemic inflammatory response syndrome and allied disorders in relation to critically injured patients. Crit Care Med 25:1789–1795
Neilly IJ, Copland M, Haj M, et al (1995) Plasma nitrate concentrations in neutropenic and non-neutropenic patients with suspected septicaemia. Br J Haematol 89:199–202
Ognibene FP, Martin SE, Parkers MM, et al (1986) Adult respiratory distress syndrome in patients with severe neutropenia. N Engl J Med 315:547–551
Price KJ, Thall PF, Kish SK, et al (1998) Prognostic indicators for blood and marrow transplant patients admitted to an intensive care unit. Am J Respir Crit Care Med 158:876–884
Rangel-Frausto MS, Pittet D, Costigan M, et al (1995) The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA 273:117–123
Regazzoni CJ, Khoury M, Irrazabal C, et al (2003) Neutropenia and the development of the systemic inflammatory response syndrome. Intensive Care Med 29:135–138
Schuster DP, Marion JM (1983) Precedents for meaningful recovery during treatment in a medical intensive care unit. Am J Med 75:402–408
Sculier JP, Paesmans M, Markiewicz E, Berghmans T (2000) Scoring systems in cancer patients admitted for an acute complication in a medical intensive care unit. Crit Care Med 28:2786–2792
Staudinger T, Stoiser B, Müllner M, et al (2000) Outcome and prognostic factors in critically ill cancer patients admitted to the intensive care unit. Crit Care Med 28:1322–1328
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Regazzoni, C.J., Irrazabal, C., Luna, C.M. et al. Cancer patients with septic shock: mortality predictors and neutropenia. Support Care Cancer 12, 833–839 (2004). https://doi.org/10.1007/s00520-004-0667-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-004-0667-5