Abstract
Purpose
The prognosis of critically ill cancer patients has improved recently. Controversies remain as regard to the specific prognosis impact of neutropenia in critically ill cancer patients. The primary objective of this study was to assess hospital outcome of critically ill neutropenic cancer patients admitted into the ICU. The secondary objective was to assess risk factors for unfavorable outcome in this population of patients and specific impact of neutropenia.
Methods
We performed a post hoc analysis of a prospectively collected database. The study was carried out in 17 university or university-affiliated centers in France and Belgium. Neutropenia was defined as a neutrophil count lower than 500/mm3.
Results
Among the 1,011 patients admitted into the ICU during the study period 289 were neutropenic at the time of admission. Overall, 131 patients died during their hospital stay (hospital mortality 45.3 %). Four variables were associated with a poor outcome, namely allogeneic transplantation (OR 3.83; 95 % CI 1.75–8.35), need for mechanical ventilation (MV) (OR 6.57; 95 % CI 3.51–12.32), microbiological documentation (OR 2.33; CI 1.27–4.26), and need for renal replacement therapy (OR 2.77; 95 % CI 1.34–5.74). Two variables were associated with hospital survival, namely age younger than 70 (OR 0.22; 95 % CI 0.1–0.52) and neutropenic enterocolitis (OR 0.37; 95 % CI 0.15–0.9). A case–control analysis was also performed with patients of the initial database; after adjustment, neutropenia was not associated with hospital mortality (OR 1.27; 95 % CI 0.86–1.89).
Conclusion
Hospital survival was closely associated with younger age and neutropenic enterocolitis. Conversely, need for conventional MV, for renal replacement therapy, and allogeneic hematopoietic stem cell transplantation (HSCT) were associated with poor outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Therapeutic advances regarding hematological malignancies during the last two decades translated into overall improvement of both short-term and long-term prognosis of hematological patients [1, 2]. Concomitantly, the prognosis of critically ill cancer patients has improved in the overall population but also in specific subgroups of patients such as those presenting with septic shock [3], acute respiratory failure [4], or pulmonary infiltration during acute myeloid leukemia [5]. However, doubt remains as regard to the specific prognosis of neutropenic patients and as regard to the prognostic impact of neutropenia in critically ill cancer patients [6, 7]. Hence, although in previous study, we found meaningful survival associated with acute respiratory failure (ARF) in neutropenic patients, hospital mortality was particularly high raising questions as regard to the benefit of ICU admission in this specific population [8].
Despite the availability of new molecules with lower side effects [9], neutropenia remains an accepted side effect of most of treatments of hematological patients [10, 11]. Neutropenia is a transient and expected immune dysfunction. Beyond cancer chemotherapy, several additional factors including sepsis, lung injury, response to chemotherapy, and underlying malignancy and its stage are usual factors associated with neutropenia duration [12]. ICU admission is frequently required in these patients as consequences of sepsis [6] and acute respiratory failure [7] and less frequently in specific conditions such as neutropenic enterocolitis [13]. Only little recently published information is, however, available as regard to these patients’ prognosis and to factors associated with outcome in this specific population of patients.
The primary objective of this study was to assess hospital outcome of critically ill neutropenic cancer patients admitted into the ICU. The secondary objective was to assess risk factors for unfavorable outcome in this population of patients and to delineate the specific prognostic impact of neutropenia in these patients’ prognosis.
Methods
Study population
We performed a post hoc analysis of a prospectively collected database specifically designed to assess outcome of critically ill hematologic patients [14]. Patients were prospectively included from 2010 to 2012. The study was carried out in 17 university or university-affiliated centers in France and Belgium that belonged to a research network instituted in 2005. In all 17 centers, a senior intensivist and a senior hematologist are available around the clock and make ICU admission decisions together. Adult patients were included in this secondary analysis if they were admitted to the ICU with a neutropenia (defined as a neutrophil count lower than 500/mm3). The appropriate ethics committees approved this study [14].
Definitions
The data in the tables and figure were collected prospectively. Newly diagnosed malignancies were defined as diagnosed within the past 4 weeks. The sepsis-related organ failure assessment (SOFA) score was computed at admission then daily throughout the patient’s stay in the ICU; this score provides an estimate of the risk of death based on organ dysfunction [15]. The performance status [16] and Charlson comorbidity index were determined at ICU admission [17]. Both leukemia and lymphoma are already part of the Charlson index.
Reasons for ICU admission were recorded on the basis of the main symptoms at ICU admission. An admission in the context of neutropenia recovery was defined as an ICU admission on the day of neutropenia recovery or in the 3 days preceding or following this. Acute respiratory failure was defined as oxygen saturation less than 90 % or PaO2 less than 60 mmHg on room air combined with severe dyspnea at rest with an inability to speak in sentences or a respiratory rate greater than 30 breaths per minute or clinical signs of respiratory distress [18]. Shock was defined as previously reported [19, 20]. Life-supporting interventions, anti-infectious agents, prophylactic treatments, urate oxidase use, and diagnostic procedures were administered at the discretion of the attending intensivists, who followed best clinical practice and guidelines. Chemotherapy, corticosteroids, hematopoietic growth factors, immunosuppressive drugs, and other cancer-related treatments were prescribed by the hematologist in charge of each patient in accordance with institutional guidelines.
Etiologic diagnoses were made by consensus by the intensivists, hematologists, and consultants, according to recent definitions [14]. In particular, etiologies of pulmonary involvement were diagnosed on the basis of predefined criteria [18]; for possible or probable invasive pulmonary aspergillosis, the most recent definitions were used [21].
Statistical analysis
The primary outcome was vital status at hospital discharge. Quantitative variables are described as median (interquartile range, IQR), qualitative variables as number (percentage). Predictors of hospital death were identified in univariate analyses either by Fisher tests or Wilcoxon tests according to the variable. Covariates that were associated with mortality at a significance level less than 0.1 were selected as candidates for multivariate logistic regression analysis. The final multivariate model was selected by a backward procedure based on p value. Log-linearity was checked for continuous variables. Non-log-linear variables were dichotomized. Hosmer–Lemeshow goodness-of-fit tests were performed on multivariate regression models.
In order to more clearly assess the influence of neutropenia on outcome, a case–control analysis was performed with patients of the initial database [14]. In this analysis, cases (neutropenic patients) were matched with controls (non-neutropenic patients). The matching procedure was performed using the Match function in the Matching (version 4.8-3.4) package of R. We used a Mahalanobis distance including the following variables: SOFA score above 7, age below 70 years, underlying malignancy (coded as lymphoid, myeloid, other), need for invasive MV, and need for vasopressors to evaluate distance between patients. Matching was performed without replacement and groups of ties were randomly broken. The seed of the process was kept to reproduce results. Among the 289 patients with neutropenia, 255 were matched. Conditional logistic regression was used to identify factors associated with hospital mortality. The cumulative survival rate in hospital according to neutropenia was presented as a Kaplan–Meier curve, and differences among groups were tested by the log-rank test. To account for the competing risk of discharge alive, survival in hospital was presented by plotting one minus the cumulative incidence of death in hospital for both groups, and the cumulative incidence of death in hospital was compared between neutropenic patients non-neutropenic patients using Gray’s test [22]. All tests were two-sided and p values less than 0.05 were considered as indicating significant association.
In order to assess the impact of prolonged life-supporting interventions, the conditional survival probability was plotted according to duration of mechanical ventilation, vasoactive drugs, and/or renal replacement therapy (RRT).
Finally, the influence of the length of stay in ICU on outcome was assessed by the transition probability of being discharged alive from ICU when estimated via multistate modeling, i.e., for each time t, the probability that a patient still in ICU at t will eventually be discharged alive.
Analyses were performed using the R statistical software version 2.15.0 (available online at http://www.R-project.org).
Results
Study population
Among the 1,011 patients admitted into the ICU during the study period 289 were neutropenic at the time of admission. The characteristics of these patients are reported in Tables 1 and 2. The main underlying malignancies were acute leukemia (n = 144; 50 %) and lymphoma (n = 75; 26 %). Ninety-seven patients were bone marrow or hematopoietic stem cell transplant (BMT/HSCT) recipients (34 %). Among reasons for ICU admission (some patients may have more than one) the more common were sepsis (230; 80 %), acute respiratory failure (186; 64 %), and shock (167; 58 %). At the time of ICU admission 228 (79 %) patients had already received an antimicrobial therapy and the vast majority of these patients received an antimicrobial therapy during their first ICU day (262; 91 %). During ICU stay, 35 patients (12 %) received cancer chemotherapy, 101 (35 %) noninvasive mechanical ventilation, 146 (50.5 %) conventional mechanical ventilation, 176 (61 %) vasopressors, and 66 (23.5 %) renal replacement therapy. The ICU mortality was 33.6 % (97 patients). Regarding treatment limitations, 70 (24.2 %) patients with neutropenia had an end-of-life decision. Among them 63 (90 %) died in ICU.
Hospital outcome
Overall, 131 patients died during their hospital stay (hospital mortality 45.3 %). The main factors associated with poor hospital outcome are reported in Table 2. After adjustment for confounders, six factors were independently associated with outcome (Fig. 1). Four variables were associated with a unfavorable outcome, namely allogeneic BMT/HSCT (OR 3.83; 95 % CI 1.75–8.35), need for conventional MV (OR 6.57; 95 % CI 3.51–12.32), microbiological documentation of a suspected sepsis (OR 2.33; CI 1.27–4.26), and need for RRT (OR 2.77; 95 % CI 1.34–5.74) while two variables were associated with hospital survival, namely younger age (<70 years; OR 0.22; 95 % CI 0.1–0.52) and neutropenic enterocolitis (OR 0.37; 95 % CI 0.15–0.9).
The probability of being discharged alive according to ICU stay is reported in Electronic Supplementary Material Fig. 1. This figure reports the proportion of patients still hospitalized in ICU for each of the reported days and finally being discharged alive. During the first 21 days, transition probabilities were similar suggesting a similar risk of favorable outcome despite ICU length of stay. Similarly, the duration of life-supporting intervention was not associated with increased hospital mortality (Electronic Supplementary Material Fig. 2).
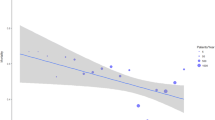
Influence of neutropenia on outcome
Finally, in order to more clearly assess the influence of neutropenia on outcome, a case–control analysis was performed after adjustment for the main confounders. A total of 251 cases and controls were included in this analysis. After adjustment, neutropenia was not associated with hospital mortality (OR 1.27; 95 % CI 0.86–1.89) (Fig. 2 and Electronic Supplementary Material Fig. 3).
Discussion
We report the results of a large multicenter cohort assessing the prognosis of neutropenic cancer patients admitted to the ICU. Overall, this study provides three important pieces of information. First, hospital survival was meaningful in this specific population of critically ill cancer patients. Hence, hospital mortality was 55 %. In addition, neutropenia was not associated with outcome after adjustment for age, initial severity, underlying malignancy, and organ support therapies. These findings suggest that neutropenia may not be a relevant risk factor for unfavorable outcome when compared to organ failure or initial severity. Finally, this study reports factors associated with unfavorable outcome in this population of patients.
This multicenter study provides an accurate snapshot of characteristics and outcome of neutropenic critically ill patients. Our results suggest a meaningful hospital survival of these patients and suggests that neutropenia has little influence on outcome. In keeping with previous studies, underlying hematological malignancy type or status was not associated with in-hospital prognosis [6, 8]. Conversely, the main independent prognosis factors were initial severity as assessed by required organ support therapy, pre-existing allogeneic HSCT, and older age [6, 8, 23, 24]. Older age is a well-known risk factor in critically ill cancer patients [6, 8, 23, 24] but also outside ICU [25–28]. Finally, despite the fact that neutropenia may reflect the engraftment period for most of the allogeneic SCT included in this study, the prognosis was poor in this subset of patients [24]. Our results suggest that in the specific subgroup of neutropenic patients, allogeneic BMT/HSCT recipients represent a high-risk population in whom two kinds of immunosuppression are concomitant. Neutropenia represents the reversal part of this immunosuppression in which engraftment period and neutropenia recovery represent two crucial steps associated with high-risk situations such as neutropenia-related sepsis, pre-engraftment and engraftment syndromes [12]. These situations could contribute to the mortality. Although graft versus host disease and treatment toxicity may contribute to the poor prognosis of these patients, all of the included patients undergoing allogeneic BMT in our study were admitted during the engraftment period. As a consequence, these specific complications were unlikely to have occurred at this stage of transplantation. Additionally, neutropenia recovery may be associated with worsening of respiratory status in up to 50 % of critically ill cancer patients [29]. Granulocyte colony-stimulating factor (G-CSF) has been associated with this event [30]. Furthermore, therapeutic use of G-CSF (i.e., to treat established fever rather than to prevent infectious complications) remains of debated interest [31].
Two of the independent prognosis factors are, however, unusual. First, there was an association in this study between neutropenic enterocolitis and survival. Abdominal syndrome is usually considered as an uncommon but relevant life-threatening complication [32]. Neutropenic enterocolitis, also known as typhlitis, is a classical complication of intensive chemotherapy [32]. Neutropenic enterocolitis usually presents with fever and abdominal pain in association with severe mucositis and is seen primarily in severely immunosuppressed, neutropenic patients with cytosine arabinoside-based chemotherapy regimens. Usual management includes antibiotics and supportive care along with careful search for signs suggesting perforation or peritonitis. Surgery is usually required in the latter or in patients experiencing abrupt organ dysfunction along with usual presentation [33]. Interestingly, in this cohort of critically ill patients, neutropenic enterocolitis was diagnosed in 17 % of the neutropenic critically ill cancer patients. In this study, diagnoses were made by consensus between the intensivists, hematologists, and consultants. Although we cannot rule out that this diagnosis was overestimated, our results suggest that this complication is of heterogeneous severity, might translate into severe sepsis/septic shock and require ICU admission, but that evolution is in general favorable. However, despite the favorable outcome in the majority of these patients, some patients nevertheless experience secondary complications such as perforation or necrosis [33]. This heterogeneous presentation with a majority of patients experiencing favorable outcome and a minority experiencing life-threatening complications requiring surgery further underlines the need for a close collaboration between intensivist, radiologist, surgeon, and hematologist in assessing these patients’ care [14, 32–34]. The existing uncertainty regarding optimal management of this complication along with its high incidence is a plea for an urgent assessment of optimal therapy in patients developing this complication.
Additionally, patients with microbiologically documented infection had a poor outcome. In our study, 80 % of patients presented with sepsis, severe sepsis, or septic shock. Septic shock was, however, not independently associated with hospital mortality. This might partly reflect recent advances in supportive care in these patients along with improvements regarding management of sepsis in both neutropenic [3, 6] and non-neutropenic patients [35, 36]. As recommended [37], 81 % of septic patients were treated with a combination therapy at ICU admission. However, only 47 % of them were treated with an anti-pseudomonal beta-lactam at ICU admission; in this situation compliance with guidelines [37] was inadequate. Accordingly, positive microbiological documentation in ICU was associated with poor prognostic and might suggest an inadequacy between the initial antibiotherapy and documented infection.
Our study has several limitations that need to be taken into account. First, 25 % of patients considered for ICU admission were finally refused, suggesting that this population was selected upon ICU admission. Similarly, an unrecorded number of hematological patients with organ failure are likely not to have been considered for ICU admission because of progressive and intractable disease or expected quality of life. Nevertheless, the multicenter design of this study is likely to have limited the influence of local admission policy that may have biased the final results. Additionally, patients were included in centers with close cooperation with a hematologist and where both senior intensivists and hematologists were available at any time. Our results may therefore not translate to ICUs or hospitals with lower physician availability. In the same way, two potential interesting variables were not taken into account in our analysis. First, our study was not designed to assess the influence of ICU admission or organ failures on cancer treatment options for ICU survivors. Previous studies suggested that AKI at the initial stage of hematological malignancies was associated with lower remission rate [38, 39]. Hematologist willingness to aggressively treat patients who experienced severe complication during neutropenia remains unknown. Information in this field might be required in order to more clearly understand the influence of ICU admission of these patients on long-term prognosis. Moreover, neutropenia duration before ICU admission and therefore whole neutropenia duration were not evaluated by this study. Despite the methodological limit that may arise in evaluating this time-dependent variable [23], we believe that studies assessing the influence of neutropenia duration on outcome may be required in order to assess the prognostic influence of this variable. Finally, the absence of prognosis impact of neutropenia after matching in our study cannot be viewed as a lack of prognostic impact of this complication. First, the overall survival of neutropenic patients was non-significantly lower than survival of non-neutropenic patients after matching (Fig. 2). This may reflect a lack of statistical power to detect a prognostic impact of neutropenia. Our findings nevertheless suggest that the prognosis impact of this complication, if any, may be viewed as limited when compared to the one of initial severity or organ dysfunctions. Therefore, despite the uncertainty mentioned above, neutropenia should probably no longer be viewed as a relevant factor for triage purposes.
Overall, our results confirm the meaningful hospital survival of critically ill cancer patients with neutropenia. Additionally, our study suggests that the prognostic impact of neutropenia among critically ill cancer patients is limited when the main confounders are taken into account. Conversely, patients’ characteristics (namely age older than 70 years and allogeneic HSCT) or initial severity were associated with poor outcome whereas neutropenic enterocolitis as the main reason for ICU admission was associated with hospital survival.
References
Recher C, Coiffier B, Haioun C, Molina TJ, Ferme C, Casasnovas O et al (2011) Intensified chemotherapy with ACVBP plus rituximab versus standard CHOP plus rituximab for the treatment of diffuse large B-cell lymphoma (LNH03-2B): an open-label randomised phase 3 trial. Lancet 378:1858–1867
Vogelzang NJ, Benowitz SI, Adams S, Aghajanian C, Chang SM, Dreyer ZE et al (2012) Clinical cancer advances 2011: annual report on progress against cancer from the American Society of Clinical Oncology. J Clin Oncol 30:88–109
Zuber B, Tran TC, Aegerter P, Grimaldi D, Charpentier J, Guidet B et al (2012) Impact of case volume on survival of septic shock in patients with malignancies. Crit Care Med 40:55–62
Azoulay E, Mokart D, Rabbat A, Pene F, Kouatchet A, Bruneel F et al (2008) Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multicenter data. Crit Care Med 36:100–107
Vincent F, Hospital MA, Lemiale V, Bruneel F, Darmon M, Gonzalez F et al (2012) Therapeutic of respiratory manifestations at the early phase of acute myeloid leukaemia. Rev Mal Respir 29:743–755
Legrand M, Max A, Peigne V, Mariotte E, Canet E, Debrumetz A et al (2012) Survival in neutropenic patients with severe sepsis or septic shock. Crit Care Med 40:43–49
Mokart D, van CT, Lambert J, Textoris J, Brun JP, Sannini A et al (2012) Prognosis of acute respiratory distress syndrome in neutropenic cancer patients. Eur Respir J 40:169–176
Mokart D, Azoulay E, Schnell D, Bourmaud A, Kouatchet A, Pene F et al (2013) Acute respiratory failure in neutropenic patients is associated with a high post-ICU mortality. Minerva Anestesiol 79:1156–1163
Vanneman M, Dranoff G (2012) Combining immunotherapy and targeted therapies in cancer treatment. Nat Rev Cancer 12:237–251
Maschmeyer G, Carratala J, Buchheidt D, Hamprecht A, Heussel CP, Kahl C et al (2015) Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients (allogeneic SCT excluded): updated guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO). Ann Oncol 26:21–33
Maschmeyer G, Beinert T, Buchheidt D, Cornely OA, Einsele H, Heinz W et al (2009) Diagnosis and antimicrobial therapy of lung infiltrates in febrile neutropenic patients: guidelines of the infectious diseases working party of the German Society of Haematology and Oncology. Eur J Cancer 45:2462–2472
Mokart D, Textoris J, Ettori F, Chetaille B, Blache JL (2011) Acute respiratory distress syndrome (ARDS) in neutropenic patients. In: Azoulay E (ed) Pulmonary involvement in patients with hematological malignancies. Springer, Berlin Heidelberg, pp 477–490
Zafrani L, Azoulay E (2014) How to treat severe infections in critically ill neutropenic patients? BMC Infect Dis 14:512
Azoulay E, Mokart D, Pene F, Lambert J, Kouatchet A, Mayaux J et al (2013) Outcomes of critically ill patients with hematologic malignancies: prospective multicenter data from France and Belgium—a groupe de recherche respiratoire en reanimation onco-hematologique study. J Clin Oncol 31:2810–2818
Vincent JL, de MA, Cantraine F, Moreno R, Takala J, Suter PM et al (1998) Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med 26:1793–1800
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Charlson ME, Sax FL, MacKenzie CR, Braham RL, Fields SD, Douglas RG Jr (1987) Morbidity during hospitalization: can we predict it? J Chronic Dis 40:705–712
Azoulay E, Mokart D, Lambert J, Lemiale V, Rabbat A, Kouatchet A et al (2010) Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med 182:1038–1046
Mourad M, Chow-Chine L, Faucher M, Sannini A, Brun JP, de Guibert JM et al (2014) Early diastolic dysfunction is associated with intensive care unit mortality in cancer patients presenting with septic shock. Br J Anaesth 112:102–109
Mourad M, Chow-Chine L, Faucher M, Sannini A, Brun JP, de Guibert JM et al (2013) Early diastolic dysfunction is associated with intensive care unit mortality in cancer patients presenting with septic shock. Br J Anaesth 112(1):102–109
De PB, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T et al (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821
Resche-Rigon M, Azoulay E, Chevret S (2006) Evaluating mortality in intensive care units: contribution of competing risks analyses. Crit Care 10:R5
Darmon M, Azoulay E, Alberti C, Fieux F, Moreau D, Le Gall JR et al (2002) Impact of neutropenia duration on short-term mortality in neutropenic critically ill cancer patients. Intensive Care Med 28:1775–1780
Pene F, Aubron C, Azoulay E, Blot F, Thiery G, Raynard B et al (2006) Outcome of critically ill allogeneic hematopoietic stem-cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol 24:643–649
Azoulay E, Thiery G, Chevret S, Moreau D, Darmon M, Bergeron A et al (2004) The prognosis of acute respiratory failure in critically ill cancer patients. Medicine (Baltimore) 83:360–370
Buchner T, Berdel WE, Wormann B, Schoch C, Haferlach T, Schnittger S et al (2005) Treatment of older patients with AML. Crit Rev Oncol Hematol 56:247–259
Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, Bouabdallah R et al (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346:235–242
Thieblemont C, Coiffier B (2007) Lymphoma in older patients. J Clin Oncol 25:1916–1923
Rhee CK, Kang JY, Kim YH, Kim JW, Yoon HK, Kim SC et al (2009) Risk factors for acute respiratory distress syndrome during neutropenia recovery in patients with hematologic malignancies. Crit Care 13:R173
Karlin L, Darmon M, Thiery G, Ciroldi M, de Miranda S, Lefebvre A et al (2005) Respiratory status deterioration during G-CSF-induced neutropenia recovery. Bone Marrow Transplant 36:245–250
Berghmans T, Paesmans M, Lafitte JJ, Mascaux C, Meert AP, Jacquy C et al (2002) Therapeutic use of granulocyte and granulocyte–macrophage colony-stimulating factors in febrile neutropenic cancer patients. A systematic review of the literature with meta-analysis. Support Care Cancer 10:181–188
Hohenberger P, Buchheidt D (2005) Surgical interventions in patients with hematologic malignancies. Crit Rev Oncol Hematol 55:83–91
Badgwell BD, Cormier JN, Wray CJ, Borthakur G, Qiao W, Rolston KV et al (2008) Challenges in surgical management of abdominal pain in the neutropenic cancer patient. Ann Surg 248:104–109
Cronin CG, O’Connor M, Lohan DG, Keane M, Roche C, Bruzzi JF et al (2009) Imaging of the gastrointestinal complications of systemic chemotherapy. Clin Radiol 64:724–733
Annane D, Sebille V, Charpentier C, Bollaert PE, Francois B, Korach JM et al (2002) Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA 288:862–871
Ferrer R, Artigas A, Levy MM, Blanco J, Gonzalez-Diaz G, Garnacho-Montero J et al (2008) Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA 299:2294–2303
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA et al (2011) Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 52:427–431
Canet E, Zafrani L, Lambert J, Thieblemont C, Galicier L, Schnell D et al (2013) Acute kidney injury in patients with newly diagnosed high-grade hematological malignancies: impact on remission and survival. PLoS One 8:e55870
Munker R, Hill U, Jehn U, Kolb HJ, Schalhorn A (1998) Renal complications in acute leukemias. Haematologica 83:416–421
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
A study from the Groupe de Recherche en Réanimation Respiratoire en Onco-Hématologie (GRRROH), Paris, France (http://www.grrroh.com).
Take-home message: Hospital survival is closely associated with younger age and with neutropenic enterocolitis. Need for conventional MV, for renal replacement therapy, and allogeneic HSCT were associated with poor outcome.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mokart, D., Darmon, M., Resche-Rigon, M. et al. Prognosis of neutropenic patients admitted to the intensive care unit. Intensive Care Med 41, 296–303 (2015). https://doi.org/10.1007/s00134-014-3615-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3615-y