Abstract
The relationship between heat waves and mortality has been widely described, but there are few studies using long daily data on specific-cause mortality. This study is undertaken in central Spain and analysing natural causes, circulatory and respiratory causes of mortality from 1975 to 2008. Time-series analysis was performed using ARIMA models, including data on specific-cause mortality and maximum and mean daily temperature and mean daily air pressure. The length of heat waves and their chronological number were analysed. Data were stratified in three decadal stages: 1975–1985, 1986–1996 and 1997–2008. Heat-related mortality was triggered by a threshold temperature of 37 °C. For each degree that the daily maximum temperature exceeded 37 °C, the percentage increase in mortality due to circulatory causes was 19.3 % (17.3–21.3) in 1975–1985, 30.3 % (28.3–32.3) in 1986–1996 and 7.3 % (6.2–8.4) in 1997–2008. The increase in respiratory cause ranged from 12.4 % (7.8–17.0) in the first period, to 16.3 % (14.1–18.4) in the second and 13.7 % (11.5–15.9) in the last. Each day of heat-wave duration explained 5.3 % (2.6–8.0) increase in respiratory mortality in the first period and 2.3 % (1.6–3.0) in the last. Decadal scale differences exist for specific-causes mortality induced by extreme heat. The impact on heat-related mortality by natural and circulatory causes increases between the first and the second period and falls significantly in the last. For respiratory causes, the increase is no reduced in the last period. These results are of particular importance for the estimation of future impacts of climate change on health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
From the last century until the present, a number of studies have described the relationship between high ambient temperature and morbidity/mortality and how this extends to different settings with their respective geographical and socio-economic determinants. Hence, the effects of heat on mortality have been observed to be swifter than those of cold, in that they tend to be concentrated in the first 3–4 days following the occurrence of high temperatures (Alberdi et al. 1997; Hajat et al. 2002; Montero et al. 2012). Threshold temperatures have also been established, above which mortality is seen to rise sharply. Moreover, such threshold temperature has come to be viewed as the benchmark from which a heat wave can be considered to be present, though this continues to be a controversial aspect from a public health standpoint (Montero et al. 2013). This threshold also varies according to the geographical setting of the study, so that the maximum temperature would be 36.5 °C for Madrid (Diaz et al. 2006a), 33.5 °C for Lisbon (Dessai 2002), 32 °C for Paris (Pascal et al. 2013) or 41.7 °C (apparent temperature) for Phoenix (Harlan et al. 2014). Similarly, there is evidence to show that the longer the duration of a heat wave, the greater the rise in mortality (Gasparrini and Armstrong 2011; Montero et al. 2012), as is also the case with the first heat wave of the season (Diaz et al. 2006b).
Yet, aside from the geographical differences detected (Baccini et al. 2008; Hajat et al. 2005; Keatinge et al. 2000), observation has also shown that this temperature-mortality association is not stable across time and, indeed, that it can display shifts in the trend of both the so-called threshold temperatures (Mirón et al. 2010) and their effects on morbidity and mortality. This may well mean that previously established preventive measures must be reviewed and that estimates of the possible longer-term impacts of climate change on health must be reconsidered (Huang et al. 2011; Ostro et al. 2012). Although there are studies investigating this aspect, they are not yet very wide-spread and could report different or nuanced results, depending on the geographical area where they are undertaken. Indeed, most of the studies conducted to date have described a weakening of the heat-mortality association with the passage of years, as in the USA, where analysis of heat-related excess mortality in 28 USA cities from 1964 to 1998 showed that in 19 of these, the weakening of the relationship was statistically significant (Davis et al. 2003a), with similar results being reported for London (Carson et al. 2006), South Korea (Ha and Kim 2013) and Italy (Schifano et al. 2012). Not only have there been few such studies but also most of them have focused on all-cause mortality, without taking the behaviour of the different specific causes of heat-related mortality into account (Basu 2009). Furthermore, the length of the time series used, in all cases less than 30 consecutive years, detracted from the climatic representativeness of the results obtained, in terms of the characteristics of extreme thermal events.
This paper reports on a study which analysed the changes over time in natural-, circulatory- and respiratory-cause mortality during heat waves in the region of Castile-La Mancha (Spain) from 1975 to 2008.
Materials and methods
The Autonomous Region of Castile-La Mancha is situated in the centre of the Iberian Peninsula, with the greater part of its territory extending across the so-called Submeseta Meridional (Southern Sub-plateau) (latitude, 38° 01′ N and 41° 20′ N; longitude, 0° 55′ W and 5° 24′ W). Close on 70 % of Castile-La Mancha lies at an altitude of 600 to 1000 m above sea level and has a land surface area of 79,463 km2, which is equivalent to 15.7 % of Spanish territory and so makes it the third largest region in the country. It has a Mediterranean-type climate of a pronounced continental nature, with wide-ranging temperatures, both daily and seasonal, i.e. summers generally tend to be dry and hot, with temperatures frequently rising to over 30 °C, and winters are marked by frequent ground frost and an irregular rainfall distribution. The latest official census (2011) shows the population as being 2,099,057, which translates as a population density of only 26.42 inhabitants per square kilometres. All population data cited in this study were drawn from official, ten-yearly, population censuses and intercensal population estimates at 1 January of each year, published by the National Statistics Institute (NSI) (Instituto Nacional de Estadística).
The daily regional mortality data for the period 1975–2008 were sourced from the NSI, were coded as per the International Classification of Diseases (ICD 8: 1975–1979, ICD 9: 1980–1998 and ICD 10: 1999–2008) and covered daily mortality due to natural causes (all except external) (ICD 10, A00-R99), circulatory causes (ICD 10, I00-I99) and respiratory causes (ICD 10, J00-J99).
Daily maximum temperature and air pressure records for the period 1975–2008 were supplied by the State Meteorological Agency (Agencia Estatal de Meteorología/AEM). We chose those corresponding to the Toledo observatory (initially known as Lorenzana and currently as Buenavista), which can be regarded as representative of the regional thermometric cluster following principal components factor analysis (Mirón et al. 2006).
We first calculated the threshold temperature of natural cause mortality in Castile-La Mancha, considering the entire study period. To this end, the daily mortality data series was filtered using an autoregressive integrated moving average (ARIMA) model obtained for this purpose (pre-whitened). This enabled us to control for variability due to autoregressive characteristics, seasonal cyclical characteristics, periodicities and the series own intrinsic trend, and so obtain a series of residuals which was compared against the series of maximum daily temperatures at 2 °C intervals to calculate a threshold temperature above which mortality rose significantly (Mirón et al. 2010; Montero et al. 2012). This threshold temperature would be the midpoint of the interval of maximum daily temperatures, above which—and for intervals of increasing temperatures—all the mortality residuals would be significantly higher (p < 0.05) than the mean value of the mortality residuals obtained using the whole series. This threshold would determine the creation of the variable, “Thw”, of differences between maximum daily temperatures (Tmax) and said threshold. On the basis of this mortality trigger temperature, a heat-wave day could then be defined, for study purposes only, as any day on which the maximum temperature exceeded the threshold.
For the next stage in our analysis, we selected the summer months (from June to September) and constructed multivariate ARIMA models (Makridakis et al. 1983) divided into three sub-periods (1975–1985, 1986–1996 and 1997–2008), in order to perform result intercomparisons and ascertain the temporal changes in results over time. We obtained these models of three dependent variables, i.e. natural-cause mortality, circulatory-cause mortality and respiratory-cause mortality.
The independent external variables included in the analysis were as follows:
-
Maximum temperatures (Tmax) higher than the threshold, lagged 0 to 7 days: Thw0, Thw1, Thw2,…Thw7, expressed as the difference between Tmax and threshold temperature (37 °C). This variable would have a value of 0 if Tmax ≤ 37 °C.
-
Pressure trend (PT), obtained as the difference between mean air pressure on any given day less that of the following day, lagged 0 to 7 days: PT0, PT1, PT2,…PT7. A negative PT would indicate a rise in air pressure (anticyclonic trend), and a positive PT would indicate a fall in pressure or cyclonic trend.
-
Heat-wave duration (Dhw), whereby a heat wave was coded with a number corresponding to the number of consecutive days on which the threshold was exceeded, e.g., where the threshold temperature was surpassed on only one day, this received a value of 1, where the threshold temperature was surpassed on two consecutive days, a value of 2, and so on.
-
Heat-wave number (Nhw). This described the chronological number of a heat wave in any given summer, such that when the threshold was exceeded the first time, it was coded as 1, the second time as 2 and so on.
These last two variables, heat-wave duration and heat-wave number, would show the increase produced in mortality by a variation in their respective ordinal scales, i.e. in a case where heat-wave duration increased by 1 day or, alternatively, where the heat wave was not the first of the year.
No indicator of absolute moisture in the atmosphere has entered because the only variable available during the completed period was the relative humidity, and its inverse relationship with temperature makes it not advisable to use in modelling (Morán 1984). The meteorological indicator variable of air pressure has introduced into the models as control variable. Previous studies undertaken in Castile-La Mancha justify the need for this independent variable to be included in the analysis of the impact of thermal extremes on mortality (Montero et al. 2012). Furthermore, the physiopathological mechanisms linked to changes in pressure make their inclusion in the analysis necessary (González et al. 2001).
The autocorrelation of the series was controlled by introducing the autoregressive and moving-average operators of the ARIMA model. Trends and seasonalities were controlled using circular functions—sine and cosine—with annual and six-monthly periodicities. The model’s goodness-of-fit was obtained by analysis of residuals (ACF, PACF, Box-Ljung) (Mirón 2012).
In addition, a jackknife sensitivity analysis was performed, with the series being divided into four periods for the purpose, i.e. 1975–1983, 1984–1996, 1997–2003 and 2004–2008.
The values of the estimator of the variables that were significant at p < 0.05 (p value supplied by SPSS v15) indicated the increase in mortality for an increase of one unit in each independent variable. When there were several significant lags for the same variable, the value of the estimator was obtained by summing the values of all the significant estimators. The percentage increase in mortality was obtained by considering the average mortality due to this cause across the season considered.
Results
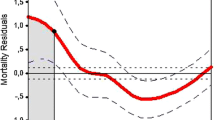
A natural-cause mortality threshold temperature of 37 °C was obtained for the Region of Castile-La Mancha, by considering the maximum daily temperature series for the city of Toledo (Fig. 1). Any day on which a temperature was registered that was higher than this threshold was defined for study purposes as a heat-wave day. Moreover, this served as the reference temperature for the creation of the variable, Thw, which was introduced, with up to 7 lags (from 0 to 7), into the multivariate ARIMA models (one model for each of the three sub-periods to be compared and for each cause of death considered). Table 1 shows the descriptive statistical data for the variables, by sub-period, while Table 2 shows data on heat-wave changes from 1975 to 2008. The variables and lags which proved significant (p < 0.05) in each sub-period are shown in Table 3.
Natural causes
A significant relationship between extreme heat (Thw) and mortality was found at lags 1, 2 and 4 during the first sub-period, lags 1, 2, 4 and 6 during the second sub-period and lags 0, 2 and 3 during the third sub-period. Immediately following the date on which the maximum extreme temperature was recorded, the number of successive days on which natural-cause mortality proved significant rose between the first and the second sub-periods and then fell in the third. In terms of aggregate mortality at all significant lags, and taking the mean mortality for each sub-period as reference (Table 3), the increase in natural-cause mortality in Castile-La Mancha for each degree centigrade that the temperature at the Toledo observatory exceeded 37 °C was as follows: 14.7 % (±1.6 %) from 1975 to 1985, 13.3 % (±0.9 %) from 1986 to 1996 and 9.1 % (±0.9 %) from 1997 to 2008 (statistically significant decrease (p < 0.05).
The indicator variable of heat-wave duration (Dhw) entered the models of the first and second third of the 34-year series at lag 0, with the value of the estimator translating as increases in natural-cause mortality of 1.7 % in the period 1975–1985 and 1.15 % in the period 1986–1996 for each day that the heat wave lasted (days with Tmax > 37 °C).
Circulatory causes
In the case of peak temperatures, a significant relationship with circulatory causes of death was found at lags 1, 3 and 4 during the first sub-period, lags 1, 3, 4 and 6 during the second sub-period and lags 0 and 2 during the third sub-period. The sequence of significant Thw lags across these three sub-periods was 3-4-2. Considering the sum of the estimators of all the significant lags for each sub-period, circulatory-cause mortality in Castile-La Mancha increased by 19.3 % (±2.0 %) in the sub-period 1975–1985, 30.3 % (±2.0 %) in the sub-period 1986–1996 and 7.3 % (±1.1 %) in the sub-period 1997–2008 (significant decrease).
In the sub-period 1986–1996, mortality due to this cause increased by 2.8 % (±0.8 %) for each day of heat-wave duration.
Respiratory causes
In this case, the significant relationship between high temperature and mortality appeared at lag 3 during the first sub-period, lags 2 and 3 during the second sub-period and lags 2 and 4 during the third sub-period. Expressed as a sequence, the number of significant Thw lags per period was 1-2-2. In other words, there was one more day with significant effects of peak extreme temperatures on mortality due to this cause with respect to the first third of the series (1975–1985). When the increase in regional mortality was calculated on the basis of the estimators of the significant lags in each sub-period and the mean mortality of each sub-period, it showed increases in respiratory-cause mortality for each degree centigrade that the maximum temperature exceeded 37 °C at the reference observatory of 12.4 % (±4.6 %) from 1975 to 1985, 16.3 % (±2.1 %) from 1986 to 1996 and 13.7 % (±2.2 %) from 1997 to 2008. The variable “Dhw” also appeared in the multivariate models when this cause of mortality was considered as a dependent variable, showing increases in mortality of 5.3 % (±2.7 %) and 2.3 % (±0.7 %) for each day that the heat wave persisted in the first and last sub-periods, respectively.
The indicator variable of heat-wave number did not prove significant in any of the models constructed. The sensitivity analysis yielded similar results when periods other than those described were chosen.
Discussion
This study’s most noteworthy findings are the detection of changes over time in heat-related mortality similar to those reported by other recent studies (Ha and Kim 2013; Schifano et al. 2012), as well as the difference in the trend for circulatory-cause and respiratory-cause mortality across the 34 years of previously unanalysed daily heat-wave data for Castile-La Mancha. Whereas a significant decline was observed in the last third of the time series in terms of the increase in circulatory-cause mortality for each degree centigrade that the maximum temperature exceeded 37 °C at the Toledo observatory, in the case of respiratory causes, however, no such decline was in evidence: Instead, the rate was maintained from 1974 to 2008. There are no prior references to the comparative time trends for these groups of causes of mortality with respect to extreme temperatures, so that these results are novel and undoubtedly relevant, bearing in mind that it is precisely these two groups of causes of death which are most closely implicated in increased heat-related mortality (Basu and Ostro 2008; Pan et al. 1995; Van Rossum et al. 2001). Within the context of the favourable trend in the socio-economic indicators during this period, both in Spain in general and in Castile-La Mancha in particular, it is possible that the improvement in health services may have had a greater impact on improved care of health problems linked to rapidly progressive acute circulatory processes (infarction, angina pectoris, stroke, etc.), such as those associated with extreme heat (Linares and Díaz 2008), than of health problems linked to respiratory processes, which tend to have a less immediate, more chronic nature. Some studies identify atrial fibrillation as a risk factor for infarction, which raises the susceptibility of individuals in situations of extreme heat (Bouchama et al. 2007; Zanobetti et al. 2013). It is known that in the last 15 years, early mortality (at 30 days) due to ST-segment elevation acute myocardial infarction has gone from 13 to 4 % in France (Puymirat et al. 2012) and that in the period between 1995 and 2005, it fell from 12.6 to 6 % in Spain (Aros et al. 2011), with this being attributed not only to epidemiological changes in the population, such as the reduction in smoking (Soriano Ortiz et al. 2009), but also to improved and faster health-care delivery, with the implementation of new reperfusion and thrombolysis techniques (Jiménez-Candil et al. 2013). In Castile-La Mancha, the number of percutaneous coronary interventions (reperfusions) multiplied by 5.6 between 2003 and 2008, due to the expansion of the regional haemodynamics network (Moreu et al. 2011). The above took place in the context of a parallel improvement in the economic resources allocated to public health funding in Spain, with the budget rising from 4.30 % of the country’s gross domestic product (GDP) in 1980 to 6.25 % in 2008.
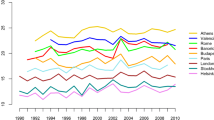
Observation of the trend in the percentage of the region’s population aged over 65 years (Fig. 2) shows that this rose sharply from 1975 to 2002 and then declined until 2008, when it dropped to 1993 levels as a consequence of the arrival of immigrants, who were generally young and thus less susceptible to circulatory diseases but who might nevertheless be affected by respiratory processes of essentially infectious aetiology. According to data furnished by the Castile-La Mancha Statistics Department (www.ies.jccm.es), in the period from 2003 to 2008, the foreign population rose by 135,109 persons (a 290 % increase) and went from representing 3.95 % to account for 10.14 % of the total population, with only 1.01 % being aged 65 years or over in 2008.
Bearing in mind that the older population is indicated as being the segment most susceptible to heat-related health problems (Díaz et al. 2002), these demographic determinants linked to population ageing have most likely influenced the trend in the lagged effects of heat waves on natural-cause and, by extension, circulatory-cause mortality, with the increase (greater number of significant lags) between the first and the second third of the series of years considered, coinciding with this marked population ageing, even though it might not translate as an increase in aggregate mortality at the respective significant lags for each degree centigrade that the maximum temperature exceeds the mortality trigger threshold (37 °C), as suggested by previous studies (Miron et al. 2008). In the last third of the study period (1997–2008), which not only includes the change in sign of the older-adult population trend from 2003 onwards but also reflects more intense health-service improvements, such as those described above, the effects of heat waves diminish, both in terms of their lagged effects on natural-cause mortality (and even more so in the case of mortality specifically due to circulatory causes) and in terms of being expressed quantitatively as a percentage increase in mortality.
The trend projected for this factor from 2008 onwards is extremely unfavourable, since the current serious economic crisis has returned Castile-La Mancha to the path of population ageing, a development which, coupled with the foreseeable deterioration in health services for reasons of budgetary restrictions, will doubtless be reflected in the trend plotted by the extreme temperature-mortality relationship if the scenario indicated by the statistics should persist and be confirmed.
During the period covered by this study, NSI data show that there was an increase in the number of homes with air conditioning in Castile-La Mancha, rising from 2.9 % in 1991 to 13.9 % in 2001 and finally to 36.2 % in 2008. Taken together with the percentage decrease in the most susceptible population, this improvement in living conditions must have contributed to the favourable trend in heat-related natural-cause and circulatory-cause mortality in the latter years of the study. Studies conducted elsewhere attribute a decline in the association between heat and circulatory causes over time to an improvement in a population’s socio-economic conditions and, by extension, an improvement in health facilities and infrastructures, and dwellings (including the use of air conditioning), as in the USA (Davis et al. 2003b; Barnett 2007), South Korea (Ha and Kim 2013) and the Czech Republic (Kysely and Kriz 2008), where a downward trend in the relationship between heat and cerebrovascular disease mortality has been described.
Even so, these circumstances have not sufficed to bring about a similar trend in Castile-La Mancha in the case of respiratory-cause mortality. It could be argued that the rise in economic activity during this period caused an increase in air pollution from industry and vehicular traffic, both in the region itself and in neighbouring areas having a greater industrial and population concentration, such as Madrid: This, in turn, resulted in an increase in the levels of secondary pollutants such as ozone, which, together with the increase in suspended particulate concentrations in meteorological conditions characterised by heat waves due to inflows into the Iberian Peninsula of hot air masses from the Sahara (Jiménez et al. 2009; Tobías et al. 2011), are linked to the increase in respiratory processes, such as asthma or chronic obstructive pulmonary disease (Anderson et al. 1997; Kheirbek et al. 2013; Medina-Ramón et al. 2006). Given, however, that air pollution also has an influence on the rise in circulatory-cause mortality (Brook et al. 2004; Miller et al. 2007; Pérez et al. 2012), this factor cannot be one of the causes of the different temporal changes in heat-wave-related circulatory- and respiratory-cause mortality. We feel, therefore, that the most plausible explanation would be that the above-described health-care improvements introduced in the case of circulatory-system diseases have been more successful in reducing mortality due to these causes than those that have improvements introduced in the case of respiratory diseases. At all events, there is no air-pollution time series that covers the entire area of Castile-La Mancha, and still less, one having the length of the series analysed here. The measuring stations are concentrated in the most important urban areas and can in no way represent the exposure of the regional population, in view of the latter’s low density and geographical dispersion. There are no major urban or industrial centres in the region, so that the possible influence of air pollution would be closely limited to certain cities, without having sufficient bearing on regional or provincial mortality to alter the temperature-mortality association to any significant degree. Nevertheless, this may be regarded as a limitation of the study.
The improvement seen in the latter years of the study in the behaviour pattern of heat-related natural-cause mortality in general and circulatory-cause mortality in particular might be attributable to the favourable effect presumably had by the implementation of heat prevention plans in Spain since 2004. There is, however, evidence to show that the climatological bases of these annual plans were not the most appropriate (Montero et al. 2010; Tobias et al. 2012) and that prevention plans must be based on threshold temperatures calculated with epidemiological criteria for each province. The plans implemented in Castile-La Mancha in 2004 were not based on these epidemiological criteria, and the results yielded have not been satisfactory (Culqui et al. 2013). Hence, this is not an explanatory factor of the temporal changes described for Castile-La Mancha.
Furthermore, as has been described in a number of studies, the results show an effect of high temperatures on mortality at short lags, from 0 to 6 (Díaz et al. 2002; Hajat et al. 2002; Montero et al. 1997), though in the case of respiratory causes, the effects of heat waves are slightly more delayed, in that they are not significant until lag 2. This goes to show the less acute nature, in general, of respiratory processes causing mortality due to high temperatures.
It should be noted that the number of heat-wave days, namely, days on which the mortality threshold temperature (37 ° C) was exceeded in Toledo (Table 2), increased from 70 in the sub-period 1975–1985 to 197 in 1986–1996 and then to 208 in the last period studied, 1997–2008 (with one year more), with the mean number of days of heat-wave duration going from 2.5 to 4.7 and 4.6, respectively. In other words, there was an increase in heat-wave frequency and duration, particularly as between the first two sub-periods studied, i.e. those in which there was an increase in the lagged effects of extreme heat on mortality (though not quantitatively, as pointed out above) in Castile-La Mancha, coinciding with a stage of marked population ageing. It was from the second to the third study sub-period, at a time when there was no such sharp increase in heat-wave frequency and duration, and coinciding with a fall in the percentage of the population aged 65 years or over, that a decrease was observed in the relationship between heat waves and natural-cause mortality, due to the significant loss of influence of circulatory causes on this relationship. The significant entry into the multivariate models of the variable, Dhw, indicates the influence of heat-wave duration on the increase in mortality and the importance to public health of forecasts about global warming for these purposes, since these envisage the increase in the frequency and intensity of extreme meteorological situations. The hard evidence of the increase in heat-wave frequency and duration from 1975 to 2008 in this region of central Spain goes to reinforce the value of predictions issued by experts (IPCC 2007). The fact that this variable, Dhw, was only significant for respiratory-cause mortality (and not in the remaining causes studied) in the last sub-period (1997–2008) is revealing, in that it reinforces the differential behaviour pattern vis-à-vis circulatory causes. In this connection, some authors have proposed certain indices that would allow for this circumstance, such as the so-called heat-wave intensity index, which takes into account both the maximum temperature value reached above a given threshold and the number of days on which this limit temperature is exceeded (Diaz et al. 2006b). For this purpose, it will serve to indicate that a recent paper (Tobias et al. 2014) compares the risk of dying by taking a temperature in the 90th percentile of the summer months and comparing this to the 99th percentile in the period 1990–2004. The results indicate that for Castile-La Mancha, these values lie within the interval of 9.2–14.5 % and, translated as percentage increases per degree, are very similar to those reported by us here.
This study observed no significant influence of the chronological number of a heat wave (i.e. whether it is the first of the year or some subsequent one) on mortality, though previous studies suggest that June heat waves—the first—are those which lead to the highest mortality (Montero et al. 2012) due to the population’s lack of acclimatisation to these initial heat waves (Mastrangelo et al. 2007; Barnett et al. 2011). At the same time, however, these are the ones having the shortest duration, while those that occur in mid-summer (July and August) are the longest (Table 2), bringing about a greater increase in cumulative heat-wave mortality.
With regard to the behaviour pattern displayed by the pressure trend, it should be noted that in some cases, the sign is positive, i.e. cyclonic trend, and centres on short lags (0 and 1), whereas in others, it is negative, i.e. anticyclonic trend, and centres on longer lags (3 and 4). This result is perfectly coherent with the synoptic situations that give rise to heat-induced extreme temperatures in Spain (García et al. 2002). On the one hand, the depressions situated in the south of Spain tend to bring an advection of hot air masses from the Sahara, which cause a sharp rise in temperatures in Castile-La Mancha and would explain the short-term effect of the cyclonic trend. However, there is another synoptic situation which is not as frequent and leads to high temperatures, and this is the existence of an anticyclone over the Iberian Peninsula. In this case, since heating is due, not to advection, but rather to a heating-up of the atmosphere as a consequence of intense solar radiation, the effect is longer-term, which is in line with the longer lag observed. These results are also coherent with the physiopathological mechanisms linked to changes in pressure (González et al. 2001).
The sensitivity analysis performed to analyse the variables used in this study on mortality due to different causes demonstrates the robustness of these results.
The results yielded by this study serve to underscore the need to bear in mind temporal variation in the impacts of temperature on mortality, and this is something that adds even more uncertainty to the models used to predict the future impacts of heat on mortality under different scenarios (Linares et al. 2014a).
Conclusions
In Castile-La Mancha, the trend observed for the effects of heat waves on respiratory-cause mortality was different to that observed for circulatory-cause mortality: While in the former case, the effects were maintained from 1975 to 2008, and in the latter case, these effects showed a decline in recent years, specifically from 1997 to 2008. This differential behaviour may in part be due to the fact that the improvement in health-care services has had a greater impact on circulatory-cause mortality, due to speedier and more effective attention to patients with acute diseases more closely related to this type of cause of death, in a context, not only of socio-economic improvement and better living conditions but also of population growth attributed mainly, since 2003, to the arrival of young immigrants, with the result that from this year onwards, the total population ageing trend seen for the region until then, was reversed.
This differentiated behaviour pattern of the trend in mortality due to different specific causes, with the pronounced decline in circulatory-cause mortality, may underlie the results found by recent studies, which point towards a decrease in the effect of heat on mortality. Furthermore, these results tend to question the reliability of climate-change impact-prediction models insofar as these pertain to high temperatures, bearing in mind that such estimates assume mortality trigger temperatures and heat-related mortality to be constant.
Nevertheless, further studies are needed to establish whether the results found by us are merely local or whether they indicate a generalised trend. Moreover, it is essential to extend these types of studies to the behaviour over time of cold waves, whose impact on mortality is—at the very least—similar to that of heat waves (Linares et al. 2014b).
References
Alberdi JC, Díaz J, Montero JC, Mirón IJ (1997) Daily mortality in Madrid community (Spain) 1986–1991: relationship with atmospheric variables. Eur J Epidemiol 14:571–578
Anderson HR, Spix C, Medina S, Schouten JP, Castellsague J, Rossi G et al (1997) Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: results from the APHEA project. Eur Respir J 10(5):1064–1071. doi:10.1183/09031936.97.10051064
Aros F, Heras M, Vila J, Sanz H, Ferreira-Gonzalez I, Permanyer-Miralda G et al (2011) Reduction in 28 days and 6 months of acute myocardial infarction mortality from 1995 to 2005. Data from PRIAMHO I, II and MASCARA registries. Rev Esp Cardiol 64:972–980. doi:10.1016/j.recesp.2011.05.011
Baccini M, Biggeri A, Accetta G, Kosatsky T, Katsouyanni K, Analitis A et al (2008) Heat effects on mortality in 15 European cities. Epidemiology 5(19):711–719. doi:10.1097/EDE.0b013e318176bfcd
Barnett AG (2007) Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology 18(3):369–372
Barnett A, Rocklöv J, Hajat S (2011) The susceptible pool and its impact on the risk of death. Epidemiology 22(1):S175. doi:10.1097/01.ede.0000392213.20767.a6
Basu R (2009) High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health 8:40. doi:10.1186/1476-069X-8-40
Basu R, Ostro BD (2008) A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am J Epidemiol 168:632–637. doi:10.1093/aje/kwn170
Bouchama A, Dehbi M, Mohamed G, Matthies F, Shoukri M, Menne B (2007) Prognostic factors in heat wave related deaths: a meta-analysis. Arch Intern Med 167:2170–2176. doi:10.1001/archinte.167.20.ira70009
Brook RD, Franklin B, Cascio W et al (2004) Air pollution and cardiovascular disease: a statement for healthcare professionals from the expert panel on population and prevention science of the American heart association. Circulation 109:2655–2671. doi:10.1161/01.CIR.0000128587.30041.C8
Carson C, Hajat S, Armstrong B, Wilkinson P (2006) Declining vulnerability to temperature-related mortality in London over the 20th century. Am J Epidemiol 164(1):77–84. doi:10.1093/aje/kwj147
Culqui DR, Diaz J, Simón F, Tobías A, Linares C (2013) Evaluation of the plan for surveillance and controlling of the effects of heat waves in Madrid. Int J Biometeorol. doi:10.1007/s00484-013-0731-2
Davis RE, Knappenberger PC, Novicoff WM, Michaels PJ (2003a) Decadal changes in summer mortality in U.S. cities. Int J Biometeorol 47(3):166–175. doi:10.1007/s00484-003-0160-8
Davis RE, Knappenberger PC, Michaels PJ, Novicoff WM (2003b) Changing heat-related mortality in the United States. Environ Health Perspect 111(14):1712–1718
Dessai S (2002) Heat stress and mortality in Lisbon. Part I: model construction and validation. Int J Biometeorol 47:6–12. doi:10.1007/s00484-002-0143-1
Díaz J, Jordán A, García R, López C, Alberdi JC, Hernández E et al (2002) Heat waves in Madrid 1986–1997: effects on the health of the elderly. Int Arch Occup Environ Health 75:163–170
Diaz J, Linares C, Tobias A (2006a) Impact of extreme temperatures on daily mortality in Madrid (Spain) among the 45–64 age-group. Int J Biometeorol 50:342–348. doi:10.1007/s00484-006-0033-z
Diaz J, Garcia-Herrera R, Trigo RM, Linares C, Valente MA, De Miguel JM, Hernandez E (2006b) The impact of the summer 2003 heat wave in Iberia: how should we measure it? Int J Biometeorol 50(3):159–166. doi:10.1007/s00484-005-0005-8
García R, Prieto L, Díaz J, Hernández E, Del Teso MT (2002) Synoptic conditions leading to extremely high temperatures in Madrid. Ann Geophys 20:237–245
Gasparrini A, Armstrong B (2011) The impact of heat wave mortality. Epidemiology 22:68–73. doi:10.1097/EDE.0b013e3181fdcd99
González S, Díaz J, Pajares MS, Alberdi JC, López C, Otero A (2001) Relationship between atmospheric pressure and mortality in the Madrid autonomous region: a time series study. Int J Biometeorol 45:34–40
Ha J, Kim H (2013) Changes in the association between summer temperature and mortality in Seoul, South Korea. Int J Biometeorol 57:535–544. doi:10.1007/s00484-012-0580-4
Hajat S, Kovats RS, Atkinson RW, Haines A (2002) Impact of hot temperatures on death in London: a time series approach. J Epidemiol Community Health 56:367–372. doi:10.1136/jech.56.5.367
Hajat S, Armstrong BG, Gouveia N, Wilkinson P (2005) Mortality displacement of heat-related deaths: a comparison of Delhi, Sao Paulo, and London. Epidemiology 16(5):613–620
Harlan SL, Chowell G, Yang S, Petitti DB, Morales Butler EJ, Ruddell BL, Ruddell DM (2014) Heat-related deaths in hot cities: estimates of human tolerance to high temperature thresholds. Int J Environ Res Public Health 11(3):3304–3326. doi:10.3390/ijerph110303304
Huang C, Barnett AG, Want X, Vaneckova P, Fitzgerald G, Tong S (2011) Projecting future heat-related mortality under climate change scenarios: a systematic review. Environ Heal Perspect 119:1681–1690. doi:10.1289/ehp.1103456
IPCC WGI (2007) Climate change 2007: the physical science basis. In: Solomon S, Qin D, Manning M, Chen Z, Marquis M, Tignor KBM, Miller HL (eds) Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press, Cambridge
Jiménez E, Linares C, Rodríguez LF, Bleda MJ, Díaz J (2009) Short-term impact of particulate matter (PM2,5) on daily mortality among the over-75 age group in Madrid (Spain). Sci Total Environ 407(21):5486–5492. doi:10.1016/j.scitotenv.2009.06.038
Jiménez-Candil J, Díaz-Castro O, Barrabés JA, García de la Villa B, Bodí Peris V, López Palop R, Fernández-Ortiz A, Martínez-Sellés M (2013) Update on ischemic heart disease and critical care cardiology. Rev Esp Cardiol 66(3):198–204. doi:10.1016/j.recesp.2012.10.019
Keatinge WR, Donaldson GC, Cordioli E, Martinelli M, Kunst AE, Mackenbach JP et al (2000) Heat-related mortality in warm and cold regions of Europe: observational study. BMJ 321(7262):670–673. doi:10.1136/bmj.321.7262.670
Kheirbek I, Wheeler K, Walters S, Kass D, Matte T (2013) PM2.5 and ozone health impacts and disparities in New York City: sensitivity to spatial and temporal resolution. Air Qual Atmos Health 6(2):473–486. doi:10.1007/s11869-012-0185-4
Kysely J, Kriz B (2008) Decreased impacts of the 2003 heat waves on mortality in the Czech Republic: an improved response? Int J Biometeorol. doi:10.1007/s00484-008-0166-3
Linares C, Díaz J (2008) Impact of high temperatures on hospital admissions: comparative analysis with previous studies about mortality (Madrid). Eur J Public Health 18(3):317–322. doi:10.1093/eurpub/ckm108
Linares C, Montero JC, Mirón IJ, Criado-Álvarez JJ, Díaz J (2014a) The time trend temperature-mortality as a factor of uncertainty analysis of impacts of future heat waves. Environ Health Perspect 122(5):A118. doi:10.1289/ehp.1306670
Linares C, Diaz J, Tobías A, Carmona R, Mirón IJ (2014b) Impact of heat and cold waves on circulatory-cause and respiratory-cause mortality in Spain: 1975–2008. Stoch Environ Res Risk Assess. doi:10.1007/s00477-014-0976-2
Makridakis S, Wheelwright SC, McGee VE (1983) Forecasting methods and applications. Wiley, San Francisco
Mastrangelo G, Fedeli U, Visentin C, Milan G, Fadda E, Spolaore P (2007) Pattern and determinants of hospitalization during heat waves: an ecologic study. BMC Public Health 7:200. doi:10.1186/1471-2458-7-200
Medina-Ramón M, Zanobetti A, Schwartz J (2006) The effect of ozone and PM10 on hospital admissions for pneumonia and chronic obstructive pulmonary disease: a national multicity study. Am J Epidemiol 163:579–588. doi:10.1093/aje/kwj078
Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JC (2007) Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 356:447–458. doi:10.1056/NEJMoa054409
Mirón IJ (2012) Temperaturas extremas y mortalidad en Castilla- La Mancha, España. Evolución temporal 1975–2003 de la relación entre temperatura y mortalidad y perspectivas ante el cambio climático [Extreme temperatures and mortality in Castile-La Mancha, Spain. Time trend from 1975 to 2003 in the relationship between temperature and mortality, and prospects in the face of climate change]. Editorial Académica Española, Lap Lambert Academic Publishing GmbH & Co, Berlín, Germany
Mirón IJ, Montero JC, Criado-Alvarez JJ, Gutiérrez AG, Paredes BD, Mayoral AS, Linares C (2006) Treatment and temperature series study for use in public health. The case of Castilla-La Mancha, Spain. Rev Esp Salud Publ 80(2):113–124
Miron IJ, Criado-Alvarez JJ, Diaz J, Linares C, Mayoral S, Montero JC (2008) Time trends in minimum mortality temperatures in Castile-La Mancha (Central Spain): 1975–2003. Int J Biometeorol 52(4):291–299. doi:10.1007/s00484-007-0123-6
Mirón IJ, Montero JC, Criado-Alvarez JJ, Díaz J, Linares C (2010) Effects of temperature extremes on daily mortality in Castile-La Mancha (Spain): trends from 1975 to 2003. Gac Sanit 24(2):117–122. doi:10.1016/j.gaceta.2009.10.016
Montero JC, Mirón IJ, Díaz J, Alberdi JC (1997) The influence of environmental variables on mortality due to respiratory and cardiovascular diseases among the elderly in the Madrid region, Spain. Gac Sanit 11:164–170
Montero JC, Miron IJ, Criado-A lvarez JJ, Linares C, Diaz J (2010) Comparison between two methods of defining heat waves: a retrospective study in Castille-La Mancha (Spain). Sci Total Environ 408:1544–1550. doi:10.1016/j.scitotenv.2010.01.013
Montero JC, Mirón IJ, Criado-Álvarez JJ, Linares C, Díaz J (2012) Influence of local factors in the relationship between mortality and heat waves: Castile-La Mancha (1975–2003). Sci Total Environ 1(414):73–80. doi:10.1016/j.scitotenv.2011.10.009
Montero JC, Mirón IJ, Criado-Álvarez JJ, Linares C, Díaz J (2013) Difficulties of defining the term “heat wave” in public health. Int J Environ Health Res 23(5):377–379. doi:10.1080/09603123.2012.733941
Morán F (1984) Apuntes de Termodinámica. Ed. Instituto Nacional de Meteorología, Madrid
Moreu J, Espinosa S, Canabal R, Jiménez-Mazuecos J, Fernández-Vallejo V, Cantón T et al (2011) The primary percutaneous coronary intervention program in Castile-La Mancha. Rev Esp Cardiol Supl 11(C):61–68
Ostro B, Barrera-Gómez J, Ballester J, Basagaña X, Sunyer J (2012) The impact of future summer temperature on public health in Barcelona and Catalonia, (Spain). Int J Biometeorol. doi:10.1007/s00484-012-0529-7
Pan WH, Li LA, Tsai MJ (1995) Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet 345(8946):353–355. doi:10.1016/S0140-6736(95)90341-0
Pascal M, Wagner V, Le Tertre A, Laaidi K, Honoré C, Bénichou F, Beaudeau P (2013) Definition of temperature thresholds: the example of the French heat wave warning system. Int J Biometeorol 57:21–29. doi:10.1007/s00484-012-0530-1
Pérez L, Tobías A, Pey J, Pérez N, Alastuey A, Sunyer J, Querol X (2012) Effects of local and Saharan particles on cardiovascular disease mortality. Epidemiology 23(5):768–769. doi:10.1097/EDE.0b013e3182625d0d
Puymirat E, Simon T, Steg PG, Schiele F, Gueret P, Blanchard D et al (2012) Association of changes in clinical characteristics and management with improvement in survival among patients with ST-elevation myocardial infarction. JAMA 308:998–1006. doi:10.1001/2012.jama.11348
Schifano P, Leone M, De Sario M, de Donato F, Bargagli AM, Díppoliti D et al (2012) Changes in the effects of heat on mortality among the elderly from 1998–2010: results from a multicenter time series study in Italy. Environ Health 11:58. doi:10.1186/1476-069X-11-58
Soriano Ortiz JB, Almagro P, Sauleda Roig J (2009) Causes of mortality in COPD. Arch Bronconeumol 45(Supl 4):8–13. doi:10.1016/S0300-2896(09)72857-1
Tobías A, Pérez L, Díaz J, Linares C, Pey J, Alastruey A, Querol X (2011) Short-term effects of particulate matter on total mortality during Saharan dust outbreaks: a case-crossover analysis in Madrid (Spain). Sci Total Environ 15(412–413):386–389. doi:10.1016/j.scitotenv.2011.10.027
Tobias A, Armstrong B, Zuza I, Gasparrini A, Linares C, Diaz J (2012) Mortality on extreme heat days using official thresholds in Spain: a multi-city time series analysis. BMC Public Health 12:133. doi:10.1186/1471-2458-12-133
Tobias A, Armstrong B, Gasparrini A, Diaz J (2014) Effects of high summer temperatures on mortality in 50 Spanish cities. Environ Health 13:48. doi:10.1186/1476-069X-13-48
Van Rossum C, Shipley MJ, Hemingway H, Grobbee DE, Mackenbach JP, Marmot MG (2001) Seasonal variation in cause-specific mortality: are there high-risk groups? 25-year follow-up of civil servants from the first Whitehall study. Int J Epidemiol 30:1109–1116. doi:10.1093/ije/30.5.1109
Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD (2013) Susceptibility to mortality in weather extremes. Effect modification by personal and small-area characteristics. Epidemiology 24:809–819. doi:10.1097/01.ede.0000434432.06765.91
Acknowledgments
This study was funded by grants from the Castile-La Mancha Socio-Healthcare Foundation (Fundación Sociosanitaria de Castilla-La Mancha), Dossier PI 2010/007, and from the Spanish Health Research Fund (Fondo de Investigaciones Sanitarias, FIS), Dossier PI12/01404-ENPY 1001/13 and “Miguel Servet Type 1” Grant: SEPY 1037/14 from the Carlos III Institute of Health.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 27 kb)
Rights and permissions
About this article
Cite this article
Miron, I.J., Linares, C., Montero, J.C. et al. Changes in cause-specific mortality during heat waves in central Spain, 1975–2008. Int J Biometeorol 59, 1213–1222 (2015). https://doi.org/10.1007/s00484-014-0933-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00484-014-0933-2