Abstract
Background
The International Pediatric Nephrology Association (IPNA) Global Kidney Replacement Therapy (KRT) Registry was established to evaluate the incidence and outcomes of kidney replacement therapy (dialysis and transplantation) provided to children worldwide. Analysis of registry data for separate regions is feasible.
Methods
Three centers located in Shanghai, Guangzhou, and Zhengzhou, which have the greatest number of pediatric kidney transplantation cases in China, participated in this analysis of transplant data. Data were registered by each center for patients under the age of 19 years who received a single-organ kidney transplant for the first time between 2011 and 2018.
Results
In total, 415 patients (59.8% male) aged 1.4–18.7 (median 12.1) years were followed for 0.3–97.1 (median 27.7) months. The number of kidney transplants increased from a total of 129 during 2011–2014 to 286 cases during 2015–2018. 85.8% of patients received the transplanted kidney from a pediatric (age < 19 years) donor, and deceased donors accounted for 94% of all donors. 8.0% of grafts were lost. One and 5-year patient survival rates were 97.6% and 95.5%, respectively. The major cause of death was infection (7/14). Similar graft and patient survival rates were observed for organs from pediatric and adult donors in 6–11 and 12–18 year recipient age groups, whereas recipients < 6 years showed inferior patient and graft survival.
Conclusions
Pediatric kidney transplantation shows favorable short-term and medium-term outcomes in China. Our experience supports use of pediatric donors in pediatric kidney transplantation, but attention directed to the outcome of recipients aged under 6 is necessary.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Kidney replacement therapy (KRT) for children with kidney failure includes peritoneal dialysis, hemodialysis, and kidney transplantation. After decades of innovation in the development of transplant surgery expertise and highly effective immunosuppressive drug regimens, accompanied by the expansion of donor resources, kidney transplantation has become the preferred KRT modality for children with kidney failure worldwide. In China, pediatric kidney transplantation has lagged behind the practice in developed countries, as there were only 717 pediatric kidney transplants conducted in China during the 28 year period of 1983 to 2010 [1]. In recent years, the improvements of medical technology and economic resources have led to major progress in pediatric kidney transplantation in China. In addition, subsequent to the establishment of a national system for organ donation and transplantation by the Ministry of Health and the Red Cross Society of China in 2010 [2], the donation after cardiac death (DCD) program has gradually matured and has played a pivotal role in the evolution both of pediatric and adult kidney transplantation in China. Moreover, with the growing awareness of the critical role of multidisciplinary teams comprising pediatric nephrologists, transplant surgeons, dialysis and transplant nurses and coordinators, pharmacists, dieticians, psychologists, social workers, and intensive care unit physicians, the “Chinese Pediatric Kidney Transplantation Management Collaboration Group” was established in 2016 to focus on and enhance pre-transplant preparation and post-transplant management to improve the long-term outcome and quality of life of pediatric kidney transplant recipients [3].
Endorsed by the International Pediatric Dialysis Network (IPDN), a national pediatric dialysis network and online registration platform, IPDN-China (www.pedpd.org.cn), was launched in 2012, while a national pediatric kidney transplantation registry was still unavailable. In 2017, the International Pediatric Nephrology Association (IPNA) launched the IPNA Global KRT Registry in an effort to collect information on the incidence and outcome of pediatric KRT worldwide. In addition, the IPNA registry created the opportunity for countries without a KRT registry to collect and analyze country-specific information as part of their goal to increase the quantity and quality of KRT care provided to their respective pediatric kidney failure populations. We, in turn, requested and received approval from IPNA to translate the registry’s data collection form into Chinese as a means by which we were able to contribute to the IPNA Global KRT Registry, in addition to creating a national registry for China. We then conducted an analysis of the submitted data to describe the current status of pediatric kidney transplants in China and to explore factors associated with patient and graft survival.
Methods
Data source and study population
This study was approved by the Ethics Board of the Children’s Hospital of Fudan University. According to the principle of voluntary accession to data registration, the three centers which conduct the largest number of pediatric kidney transplants in China contributed data for this analysis. These three centers were Children’s Hospital of Fudan University (cooperated with Changhai Hospital, Shanghai Center), The First Affiliated Hospital of Sun Yat-sen University (Guangzhou Center), and The First Affiliated Hospital of Zhengzhou University (Zhengzhou Center).
Based on the IPNA registration and data collection form, a Chinese registration form was created. Data collected consisted of the following: patient date of birth, gender, primary kidney disease, dialysis history, date of kidney transplantation, donor type, donor age, survival status of graft and patient, and date and cause of death. Children under the age of 19 years who received their initial single-organ kidney transplant from Jan 1, 2011, to Dec 31, 2018, were included in the analysis. Data on patient and graft survival were collected up to January 2019.
Statistical analysis
Statistical analysis was performed using SPSS 21.0 for Macintosh (IBM SPSS, Chicago, IL). The mean ± standard deviation or median interquartile range was used to describe the quantitative variables, such as age and duration of follow-up, depending on the distribution of the data. Frequency and percentage were used to describe categorical variables such as gender, primary kidney disease, donor type, donor age, dialysis before transplantation, graft loss, and mortality. Kaplan-Meier survival curves were used to calculate the patient survival rate. The chi-square test, Kruskal-Wallis test, Fisher’s exact test, and log-rank test were used to determine the differences in features by transplant center. The chi-square test, Wilcoxon rank-sum test, and Fisher’s exact test were used to determine the difference in characteristics by transplant era. Log-rank test was used to compare patient survival both in different donor-recipient age combinations and different recipient age groups. Binary logistic regression and Cox proportional hazards models were used to identify the risk factors for graft loss and patient mortality, respectively. P values < 0.05 were considered statistically significant.
Results
Patient and donor characteristics
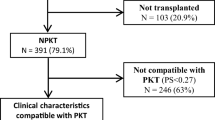
A total of 415 patients were included in this study (Supplement 1 and Table 1); 143 from Shanghai Center, 126 from Guangzhou Center and 146 from Zhengzhou Center. Among the 415 patients, 248 (59.8%) were boys; age at transplantation ranged from 1.4 to 18.7 years (median age: 12.1 years old). Prior to transplantation, 337 patients (81.2%) received dialysis. The leading causes of kidney failure were congenital anomalies of the kidney and urinary tract (CAKUT, 32.1%) and steroid-resistant nephrotic syndrome (SRNS, 18.8%) in the 0–5 years and 6–11 years recipient age groups, respectively. In the adolescent age group (12–18 years), 64.5% of the cases had kidney failure secondary to an unknown etiology (Fig. 1). Deceased donors accounted for 94.2% of all donors, including 78.3% DCD donors and 15.9% donation after brain death (DBD) donors. The “pediatric to pediatric” matching policy (both recipient and donor < 19 years of age) was implemented in 85.8% of the patients.
Primary kidney disease by different age groups. In the recipient age groups 0–5 years and 6–11 years, the leading cause of kidney failure was CAKUT (32.1%) and SRNS (18.8%), respectively. In the recipient age group 12–18 years, 64.5% of the cases had kidney failure secondary to an unknown etiology. CAKUT, congenital anomalies of kidney and urinary tract; SRNS, steroid-resistant nephrotic syndrome
Graft and patient survival
With a median follow-up time of 27.7 (11.4, 52.4) months, no patient was lost to follow-up. One hundred sixty-six and 76 patients reached the 3-year and 5-year follow-up, respectively. The graft loss rate was 8.0%, and the 1-year, 3-year, and 5-year patient survival rates overall were 97.6%, 96.8%, and 95.5%, respectively. Fourteen of the 415 patients died. The median duration from transplantation to death was 7.0 (5.8, 17.7) months. The causes of death included infection (7 cases), cardiopulmonary failure (3 cases), cerebrovascular accident (1 case), malignancy (1 case), hepatic failure (1 case), and unknown reason (1 case).
Comparison by transplant center
Table 1 shows the detailed characteristics of the different transplant centers. The age at transplantation, duration of follow-up, distribution of primary kidney disease, donor type, donor age, and dialysis history differed significantly between the centers, whereas graft loss rate and mortality rates were similar.
Comparison by transplant era
The number of kidney transplantations increased significantly from 129 patients during 2011–2014 to 286 patients during 2015–2018. The comparison of patient characteristics in 2015–2018 and 2011–2014 revealed trends towards younger age at transplantation (11.9 (8.8, 14.8) vs. 12.5 (9.6, 16.1) years, P = 0.028), more frequent pre-emptive transplantation (22.7% vs. 10.1%, P = 0.003), higher utilization of pediatric donor organs (94.4% vs. 66.7%, P < 0.001), and more DBD donors (23.1% vs. 0%, P < 0.001). Graft survival and mortality did not differ significantly (Table 2).
Donor-recipient age combination and comparison of survival
In the recipient age groups 0–5 years and 6–11 years, 100% and 94.3% of patients, respectively received a pediatric donor kidney. In the adolescent age group, 76.8% of recipients received a kidney from a pediatric donor (P = 0.000). Both in the recipient age groups 6–11 years and 12–18 years, organs from pediatric and adult donors showed similar graft loss (OR 0.577 (95% CI 0.066–5.016) in 6–11 years group, OR 2.398 (95% CI 0.529–10.871) in 12–18 years group), and mortality did not differ (Fig. 2).
Risk factors for graft loss and mortality
Variables included age at transplantation, gender, primary kidney disease, dialysis history, donor type, donor age, transplant center, and transplant era. Transplant age 0–5 years was associated with a higher risk both of graft loss (6–11 years: OR 0.159 (95% CI 0.044–0.576), 12–18 years: OR 0.227 (95% CI 0.064–0.811)) and mortality (6–11 years: HR 0.180 (95% CI 0.040–0.811), 12–18 years: HR 0.216 (95% CI 0.052–0.905)) (Fig. 3).
Discussion
We report 415 first kidney transplants which took place at the three most active pediatric transplant centers in China from 2011 to 2018, accounting for 33.5% of all pediatric kidney transplants during that 8-year period according to the Chinese Scientific Registry of Kidney Transplantation (CSRKT, www.csrkt.org). The number of kidney transplantations at these three centers increased more than two-fold from 2011–2014 to 2015–2018, and increasingly younger children underwent transplantation with time. However, prior data showed that only 717 pediatric kidney transplants were performed at 102 different transplantation centers during the period of 1983 to 2010 in China. The mean age at transplantation was 15.4 ± 2.5 years during that period of time [1]. Our study shows deceased donors accounted for 94.2% of all donors and the “pediatric to pediatric” matching policy was implemented in 85.8% of the patients. Favorable short-term and medium-term outcomes with respect to graft and patient survival are observed, whereas recipients younger than 6 years demonstrate inferior patient and graft survival.
As we know, kidney transplantation is widely recognized as being the preferred KRT option for children with kidney failure, offering optimal patient survival probabilities, as well as superior cognitive development, quality of life, and growth compared with dialysis [4, 5]. The United Kingdom Transplant Registry data on 3236 pediatric kidney transplants performed between 1 January 1992 and 31 December 2016 showed 25-year patient survival reached 79% and 86% in deceased donor transplant and living donor transplant, and the half-lives for living donor and deceased donor kidneys were 14 and 15 years, respectively [6]. Since the establishment of a new national system for organ donation and transplantation by the Ministry of Health and the Red Cross Society of China in 2010 [2], pediatric kidney transplantation in China has developed relatively rapidly in recent years. The establishment of the Chinese Pediatric Kidney Transplantation Management Collaboration Group in 2016 has also proven to be exceedingly important. This national collaboration group has focused on pre-transplant preparation (vaccinations for preventable diseases, diagnosis of primary kidney disease, effective dialysis and nutrition, attention to cognitive delays, social-psychological assessment) and post-transplant management (regular evaluation and follow-up, nutrition and growth, financial support) [3]. In our study, the 1-year and 5-year patient survival rates were 97.6% and 95.5%, respectively, well comparable to the data from the 2018 report of the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) [7], which demonstrated 5-year patient survival rates of 98.10% and 97.95% in living donor and deceased donor transplant recipients, respectively during the transplant period of 2007 to 2017.
Currently, infection is still the dominant cause of pediatric hospitalizations and death after kidney transplant [5, 7]. In our study, infections accounted for 50% and cardiopulmonary failure for 21% of deaths after transplantation. In the 2018 NAPRTCS report, infection and cardiopulmonary failure were responsible for 25.0% and 13.9% of deaths, respectively [7]. In the Australian and New Zealand Dialysis and Transplant Registry following 1810 children and adolescents from 1970 to 2015, 5-year patient survival increased from 85% in 1970–1985 to 99% in 2005–2015, predominantly because of marked reductions in cardiovascular and infection-related deaths [8]. Preventive measures (vaccinations for preventable diseases, prophylactic antibiotics/antiviral therapy) and monitoring and management of infection in pediatric kidney transplantation still need to be strengthened in China.
Our previous studies have demonstrated that the use of grafts from deceased pediatric donors is a potential approach to expand the donor pool and thus minimize waiting time [9, 10]. Shortages in donor kidneys along with improvements in surgical technique have led to an increased popularity of using young donor kidneys for transplantation. There is also a potential benefit for the family of the deceased child, as many families desire to donate their child’s organs to provide an opportunity for another human to survive [11]. In this study, comparing the data of 2015–2018 with those of 2011–2014, more children received pediatric donor organs, which is in line with an increase in the percentage of pre-emptive transplantation. Although earlier reports have shown a higher risk of graft loss in recipients of (very) young donors due to surgical complications, high rates of graft thrombosis, early rejection, and hyper-filtration injury, there has been an expansion in the practice of deceased pediatric donors recently, and there is emerging evidence that good outcomes can be achieved [12]. In addition, the “pediatric to pediatric” matching policy (both recipient and donor < 19 years of age) has been implemented in many parts of the world, although the percentage of pediatric to pediatric transplants varies by country. In Europe, among deceased donor transplant recipients, an average of 61.4% children received pediatric donor kidneys, ranging from 16.7% in Belarus to 73.2% in France [13]. This “pediatric to pediatric” matching policy potentially eliminates the cardiovascular complications of graft-recipient size mismatch and can reduce the risk of hypo-perfusion and graft non-function [14]. Grafts from pediatric donors have also shown superior long-term kidney function compared with grafts from adult donors [15, 16]. The relative glomerular filtration rate of allografts from pediatric donors was significantly higher than those from adult deceased or living-related donors after at least 4 years of follow-up in a cohort of pediatric kidney allograft recipients [15]. Pediatric donor allografts also tend to adapt to the growing child by maintaining and even increasing glomerular filtration rate over many years after transplantation, as opposed to an adult donor allograft, which will initially adapt to the pediatric recipient following transplantation but thereafter will not increase its filtration function to correlate with the increasing size and filtration demand of the growing child [14]. Data from the Scientific Registry of Transplant Recipients (SRTR) showed that among children (< 10 years) and adolescent (10–18 years) recipients, outcomes using either an ideal kidney from deceased donors aged between 15 and 35 years or split kidney from small pediatric donors (aged ≤ 8 years and weight < 30 kg) were very similar. In turn, the authors concluded that pediatric kidneys could augment the kidney donor pool and should not be considered expanded criteria donor kidneys [17]. To that end, deceased donors accounted for 94.2% of our kidney transplants, and 85.8% of all donors were pediatric donors (< 19 years). With a median follow-up time of 27.7 months, the graft loss rate was 8%, indicating good graft outcomes from the use of pediatric donor kidneys in pediatric recipients. However, the numbers of pediatric to pediatric transplants in children in China and worldwide are relatively limited, and the duration of follow-up is limited. Thus, ongoing data collection by the IPNA KRT registry will be crucial to provide long-term data on graft survival, as well as outcomes such as proteinuria, so as to address concerns regarding issues such as glomerulomegaly and hyper-filtration.
Of course, recipient and donor age are both known to affect graft survival. Graft failure was highest in the youngest and adolescent transplant recipients [13]. In adolescents, poor graft survival was attributed to poor adherence with immunosuppression regimens [18]. Recipients less than 5 years of age showed a higher risk of graft failure, especially during the first 3 months post-transplant, most likely reflecting the surgical difficulties associated with transplantation in the youngest patients [19]. Similar results were demonstrated both in the United Kingdom Transplant Registry data and the 2014 NAPRTCS report [6, 20]. The former indicated recipients under the age of 6 years had lower 1-year kidney allograft survival than recipients aged 6 years and over and this difference was maintained up to 10 years, and the latter showed the poorest graft survival in deceased donor recipients less than 2 years of age, especially during the initial post-transplant period. The European Society for Paediatric Nephrology/European Renal Association-European Dialysis and Transplantation Association (ESPN/ERA-EDTA) registry study also demonstrated that graft survival varied by recipient age. Compared with the recipient age group 6–11 years, graft failure risk was higher in patients transplanted at 0–5 years of age and during adolescence (12–19 years). In addition, the youngest deceased donor age group (0–5 years) showed the highest risk of graft failure [13]. In our study, 100%, 94.3%, and 76.8% of recipients aged 0–5 years, 6–11 years, and 12–18 years received pediatric donor kidneys, respectively. Transplant age under 6 years showed a higher risk both in graft loss and mortality compared with transplants performed with children aged 6–11 years and 12–18 years. In both of the latter patient cohorts, recipients of pediatric donor and adult donor kidneys showed similar graft loss rates and mortality risks. Therefore, additional data will be required to better determine whether recipient age under 6 years is an independent risk factor for graft failure and mortality or whether the pediatric donor-youngest recipient (0–5 years) combination is most predictive of a poor outcome in the Chinese pediatric kidney transplantation cohort.
Some limitations of our study need to be acknowledged. First, the exact age of the graft, as well as the date and cause of graft failure, were not included in the registry, which could further help differentiate early from long-term graft failure and optimal donor-recipient age combination. Second, the issue of unmeasured donor and recipient variables, such as the number of human leucocyte antigen mismatches, the percentage of panel reactive antibodies, the ischemia time, and immunosuppression regimens, might lead to residual confounding. Third, in this study, more than 50% of the cases had kidney failure from unknown etiology. Fourth, the median follow-up time in this study was 27.7 months. Only 166 and 76 patients reached the 3-year and 5-year follow-up, respectively. Therefore, the outcome results should be interpreted accordingly. Finally, only the three most active centers in terms of number of pediatric kidney transplants performed were enrolled in this study. Our results are hardly generalizable to the rest of China and should stimulate additional data collection from transplant centers throughout China.
Conclusion
The number of pediatric kidney transplantations has increased, and kidney transplantation shows favorable short-term and medium-term outcome with respect to graft and patient survival in the three largest pediatric kidney transplant centers in China. Our limited experience provides evidence that the use of pediatric donor kidneys can result in successful transplant outcomes. In order to decrease the graft loss and mortality in the youngest recipients, not only are additional multidisciplinary efforts required, but also further granular data collection in regard to pediatric donor kidneys and different donor-recipient age combinations are needed to better identify the risk factors. In July 2018, the National Health Commission of the People’s Republic of China announced an updated organ allocation and sharing policy [21]. This current allocation scheme preferentially allocates pediatric deceased donor kidneys to children on the transplant waitlist. We believe the new strategy for implementation increases the organ allocation priority for children and will promote the further development of pediatric kidney transplantation in China.
Data availability
All data generated or analyzed during this study are included in this paper.
References
Liu L, Zhang H, Fu Q, Chen L, Sun C, Xiong Y, Shi B, Wang C (2014) Current status of pediatric kidney transplantation in China: data analysis of Chinese Scientific Registry of Kidney Transplantation. Chin Med J 127:506–510
China Organ Donation Administrative Center (2010) China organ donation pilot program. http://www.rcsccod.cn/cstatute/cdonationdocuments/20100301/699052.htm Accessed 10 April 2020
Shen Q, Jiaojiao L, Yihui Z, Jing C, Xiaoyan F, Jia R, Lin F, Xiaoshan T, Jialu L, Yunli B, Wu B, Lei Z, Zhu Y, Xu M, Zhu T, Li Z, Hong X (2020) Multi-disciplinary management of pediatric renal transplantation. J Nephrol Dialy Transplant 29:20–25 (article in Chinese)
Winterberg PD, Garro R (2019) Long-term outcomes of kidney transplantation in children. Pediatr Clin N Am 66:269–280
Verghese PS (2017) Pediatric kidney transplantation: a historical review. Pediatr Res 81:259–264
Mumford L, Maxwell H, Ahmad N, Marks SD, Tizard J (2019) The impact of changing practice on improved outcomes of paediatric renal transplantation in the United Kingdom: a 25 years review. Transpl Int 32:751–761
Chua A, Cramer C, Moudgil A, Martz K, Smith J, Blydt-Hansen T, Neu A, Dharnidharka VR, NAPRTCS investigators (2019) Kidney transplant practice patterns and outcome benchmarks over 30 years: the 2018 report of the NAPRTCS. Pediatr Transplant 23:e13597
Francis A, Johnson DW, Melk A, Foster BJ, Blazek K, Craig JC, Wong G (2020) Survival after kidney transplantation during childhood and adolescence. Clin J Am Soc Nephrol 15:392–400
Zhao WY, Zhang L, Zhu YH, Zhu FY, Chen Y, Shen Q, Xu H, Zeng L (2014) Single kidneys transplanted from small pediatric donors less than 15 kilograms into pediatric recipients. Transplantation 98:e97–e100
Zhao WY, Zhang L, Zhu YH, Chen Y, Zhu FY, Shen Q, Xu H, Zeng L (2014) En bloc kidneys transplanted from infant donors less than 5 kg into pediatric recipients. Transplantation 97:555–558
Sung RS (2010) Transplantation: pediatric kidney donation after cardiac death. Nat Rev Nephrol 6:387–388
Marlais M, Callaghan C, Marks SD (2016) Kidney donation after circulatory death: current evidence and opportunities for pediatric recipients. Pediatr Nephrol 31:1039–1045
Chesnaye NC, van Stralen KJ, Bonthuis M, Groothoff JW, Harambat J, Schaefer F, Canpolat N, Garnier A, Heaf J, de Jong H, Schwartz Sørensen S, Tönshoff B, Jager KJ (2017) The association of donor and recipient age with graft survival in paediatric renal transplant recipients in a European Society for Paediatric Nephrology/European Renal Association-European Dialysis and Transplantation Association Registry study. Nephrol Dial Transplant 32:1949–1956
Chaudhuri A, Grimm P, Concepcion W (2016) Small pediatric deceased donors for pediatric renal transplant recipients. Pediatr Transplant 20:7–10
Dubourg L, Cochat P, Hadj-Aïssa A, Tydén G, Berg UB (2002) Better long-term functional adaptation to the child’s size with pediatric compared to adult kidney donors. Kidney Int 62:1454–1460
Pape L, Hoppe J, Becker T, Ehrich JH, Neipp M, Ahlenstiel T, Offner G (2006) Superior long-term graft function and better growth of grafts in children receiving kidneys from paediatric compared with adult donors. Nephrol Dial Transplant 21:2596–2600
Suneja M, Kuppachi S, Katz D, Hunsicker L (2019) Small split pediatric kidneys to expand the donor pool: an analysis of Scientific Registry of Transplant Recipients (SRTR) data. Transplantation 103:2549–2557
Van Arendonk KJ, King EA, Orandi BJ, James NT, Smith JM, Colombani PM, Magee JC, Segev DL (2015) Loss of pediatric kidney grafts during the ‘high-risk age window’: insights from pediatric liver and simultaneous liver-kidney recipients. Am J Transplant 15:445–452
Arbus GS, Rochon J, Thompson D (1991) Survival of cadaveric renal transplant grafts from young donors and in young recipients. Pediatr Nephrol 5:152–157
North American Pediatric Renal Trials and Collaborative Studies (2014) NAPRTCS 2014 Annual Transplant Report. https://web.emmes.com/study/ped/annlrept/annualrept2014.pdf. Accessed 31 December 2017
National Health Commission of the People’s Republic of China (2018) China organ allocation and sharing policy. http://www.nhc.gov.cn/yzygj/s3586/201808/d35d96f2db82403ebe2ba41f2c583896.shtml. Accessed 10 April 2020
Funding
This study was funded by multicenter clinical research project of Shanghai Municipal Health Commission (Pediatrics) (EKYY20180201).
Author information
Authors and Affiliations
Contributions
Each author has participated sufficiently in the work to take public responsibility for the content. Hong Xu and Qian Shen participated in the conception and design of the study; Qian Shen, Xiaoyan Fang, Xinyue Man, Yihui Zhai, Longshan Liu, Changxi Wang, Wenjun Shang, Guiwen Feng, Lei Zhang, and Li Zeng conducted data acquisition, analysis, and interpretation; Qian Shen and Xiaoyan Fang drafted the article and provided intellectual content of critical importance to the work described; Hong Xu, Bradley A Warady, Franz Schaefer, Youhua Zhu, Jing Chen, and Jia Rao revised the article. All authors have final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Ethics Board of the Children’s Hospital of Fudan University.
Consent to participate
Not applicable
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shen, Q., Fang, X., Man, X. et al. Pediatric kidney transplantation in China: an analysis from the IPNA Global Kidney Replacement Therapy Registry. Pediatr Nephrol 36, 685–692 (2021). https://doi.org/10.1007/s00467-020-04745-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04745-7