Abstract
Background
This study aimed to evaluate short- and long-term outcomes of kidney transplantation over 37 years in a national referral center and compare outcomes between Israeli Jewish and Arab children.
Methods
Data on 599 pediatric transplantations performed in 545 children during 1981–2017, including demographic parameters, kidney failure disease profile, and pre-transplant dialysis duration, were retrieved from our computerized database and patient files. Patient and graft survival were estimated using the Kaplan-Meier method.
Results
Twenty-year patient survival was 91.4% for live donor (LD) and 80.2% for deceased donor (DD) kidney recipients. Respective 10-year and 20-year graft survival rates for first kidney-only transplants were 75.2% and 47.0% for LD and 60.7% and 38.4% for DD grafts. Long-term graft survival improved significantly (p < 0.001) over the study period for recipients of both LD and DD allografts and reached 7-year graft survival of 92.0% and 71.3%, respectively. The proportion of DD transplantations was higher in the Arab subpopulation: 73.8% vs. 48.4% (p < 0.001). Graft survival was not associated with age at transplantation and did not differ between the Arab (N = 202) and Jewish children (N = 343). Median (IQR) waiting time on dialysis did not differ significantly between the Arab and Jewish children: 18 (10–30) and 15 (9–30) months, respectively (p Mann-Whitney = 0.312).
Conclusions
Good and progressively improving long-term results were obtained in pediatric kidney transplantation at our national referral center, apparently due to expertise gained over time and advances in immunosuppression. Equal access to DD kidney transplant and similar graft survival were found between ethnic groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney transplantation is universally accepted as the treatment of choice for children needing kidney replacement therapy and affords them the opportunity for improved quality of life compared with dialysis therapy. Recently published data of pediatric kidney transplantation attest to high rates of patient survival and graft survival [1,2,3,4,5,6,7]. However, disparities in policies and outcomes of kidney replacement therapy, including access to kidney transplants and graft survival, have been reported among populations of various ethnic backgrounds in the USA, Europe, and New Zealand [8,9,10,11,12,13].
The Pediatric Renal Transplant Program in Israel was initiated in the Pediatric Department of Beilinson Medical Center (later Schneider Children’s Medical Center) in 1981. Until 2013, this was the only government-approved pediatric kidney transplant program in Israel.
The National Transplant and Organ Donation Center was established in 1993 as an institution of the Ministry of Health, to monitor and supervise organ transplantation. Israel national health insurance provides access to primary health care for all its citizens. Patients are listed for deceased donor (DD) kidney transplantation after starting dialysis. Pre-emptive transplantation is performed only if a living donor (LD) is available. While the Arab minority comprises approximately 21% of the population [14], the prevalence range of kidney failure (KF) for the decade from 2007 to 2017 was 47.1–52.4/million for non-Jewish children (overwhelmingly of Arab ethnicity), compared with only 19.3–25.7/million for the population as a whole [15]. We examined, over 37 years, short- and long-term outcomes of pediatric kidney transplant recipients at our national transplant center and compared the results with published data. We also examined the possibility of social and ethnic disparities, by comparing waiting time for DD grafts and outcomes of kidney transplantation between the two major ethnic groups in Israel: Jews and Arabs.
Methods
We conducted a retrospective, longitudinal cohort study of all the patients below age 19 years who underwent kidney transplantation at our center between January 1981 and December 2017. Sixteen patients who received combined liver and kidney transplants were not included in the current analysis due to having different prognosis [16]. Data were obtained from the National Israeli Kidney Transplantation Registry computerized database and patient files, as well as from the Collaborative Transplant Study where our patients are reported [17]. We retrieved information on age, gender, ethnicity, native kidney disease, pre-transplant dialysis time, patient and graft survival, causes of graft failure, and causes of death. Graft loss was defined as death with a functioning graft, return to dialysis, or the date of a new preemptive transplantation. For evaluation of changes in short- and long-term patient and graft survival, the study period was divided into four eras: 1981–1990, 1991–2000, 2001–2010, and 2011–2017.
Allocation and living donation
The allocation system for DD organs is based on four parameters: time on dialysis, level of antibodies (PRA), HLA DR and B match, and age. In addition, kidneys from young donors aged < 18 years are allocated to children. For LD, first- and second-degree relatives are interviewed and approved by the hospital ethics committee, while other remote relatives and altruistic donors undergo additional psychological evaluation and an interview by a Ministry of Health Ethics committee representative.
Immunosuppression
During the early 1980s, prednisone and azathioprine were mainstay treatment. In 1985, cyclosporine was introduced as a component of a triple regimen. During the mid-1990s, cyclosporine and azathioprine were replaced by tacrolimus and mycophenolate mofetil, as maintenance immunosuppressive drugs. The current protocol consists of a triple tacrolimus-based drug regimen, which includes mycophenolate mofetil and prednisone. Tacrolimus dosages are adjusted to maintain trough level at 10–15 ng/mL for the first month, 8–12 ng/mL for the second month, 5–10 ng/mL up to 6 months after transplantation, and 4–6 ng/mL thereafter. Mycophenolate mofetil is given from day 1 after transplantation, 600 mg/m2 BSA/dose twice a day for 2 weeks, and 300 mg/m2/dose twice a day thereafter. Patients are switched to mycophenolic acid (Myfortic) if they do not tolerate mycophenolate mofetil due to gastrointestinal disturbances. Methylprednisolone is started intravenously at a dose of 10 mg/kg, 5 mg/kg, and 2.5 mg/kg in the first 3 days, replaced by oral prednisone 40 mg/m2 until day 7, and slowly tapered to 5 mg/m2 at 6 months after transplantation. In cases of severe adverse effects, tacrolimus is replaced by cyclosporine or sirolimus.
In the mid-1980s, anti-thymocyte globulin (ATG) was used as transplant induction therapy for patients with primary graft non-function, and also for treatment of steroid-resistant acute rejection. Over the past decade, ATG has been replaced by thymoglobulin for both these purposes. IL-2 receptor blocking antibodies were introduced in low-risk patients (non-sensitized, 1st transplant) as a standard induction therapy. Daclizumab 1–1.5 mg/kg × 3 doses were used until 2009 and were replaced by basiliximab 10–20 mg IV × 2, on days 1 and 4 thereafter.
Transplant biopsies were performed mostly in cases of suspected acute rejection (a rise in serum creatinine of at least 20%).
The study was approved by the Institutional Research Ethics Board of Rabin Medical Center and Schneider Children’s Medical Center of Israel.
Statistical methods
The statistical analysis was performed using IBM-SPSS software version 25 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp). Quantitative data are presented as medians and interquartile ranges (IQR) for non-parametric variables. Categorical variables are expressed as percentages. Groups were compared using Student’s t test and the nonparametric Mann–Whitney U test for continuous variables and Fisher's test or χ2 test for categorical variables. Patient and graft survival were assessed using the Kaplan-Meier survival method and the log-rank test for significance level. Cox proportional hazards analyses were used to calculate hazard ratios and 95% confidence intervals (CIs). All tests were two tailed. A p value < 0.05 was considered significant.
Results
Since the beginning of the pediatric kidney transplantation program in 1981, through the end of 2017, 545 children (63% males) received a total of 599 grafts: 499 (91.6%), a single graft; 38 (7%), two grafts; and 8 (1.5%) received three grafts. Of the 599 grafts, 378 were transplanted in 343 children of Jewish origin and 221 (37%) in 202 children of Arab origin (Table 1). The median age of recipients at transplantation was 13 years (IQR 8–17 years). Twenty-one transplantations (3.7%) were performed in children younger than age 3 years, 96 (16.0%) in children aged 3–6 years, 119 (19.8%) in children aged 7–11 years, and 363 (60.5%) in children aged 12–19 years.
The most common cause of KF was kidney dysplasia, with or without congenital anomalies of the urinary tract, 45.2%. Twenty-five percent of the patients developed KF as a result of hereditary diseases; juvenile nephronophthisis presented in 9% of the study population and atypical hemolytic uremic syndrome in 3.8%. Eight patients (1.9%) with primary hyperoxaluria received kidney transplants only, as this was common practice in the earlier period of the transplant program, before the performance of combined, or sequential, liver and kidney transplantation became accepted [16]. Focal segmental glomerulosclerosis and other glomerulopathies caused another 10.5% and 9.5% of KF, respectively. The proportion of hereditary diseases among the causes of KF was slightly higher among Arab patients: 29.0% vs. 22.5% in Jewish patients (p = 0.08).
During the study period, the majority of grafts were from deceased donors: 346 (57.8%). The proportion of DD transplantations was significantly higher in the Arab subpopulation: 73.8% vs. 48.4% (p < 0.001) (Table 1). The proportion of LD grafts was 37.8% (165/437) for the first 3 decades of the study and remained fairly constant throughout this period. During the last 7 years, 2011–2017, the proportion increased to 54.3% (88/162) (p < 0.01).
LD kidneys were transplanted pre-emptively in 18.8% (N = 113) of the total transplants; the remaining transplantations were after a median (IQR) time on dialysis of 17 (9–30) months. The median (IQR) period on dialysis while waiting for DD transplantation did not differ significantly between Arab and Jewish children: 18 (10–30) and 15 (9–30) months, respectively (p Mann-Whitney = 0.312) (Table 1).
Survival analysis
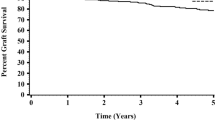
Sixteen patients who were lost to follow-up were excluded from survival analysis. Outcome data were therefore available for 529 children who underwent 583 transplantations: 248 from LDs and 335 from DDs. The median follow-up for all-cause mortality was 146 months after the last documented transplantation, including multiple transplantations. At the end of the study, 467 children were alive with functioning grafts. Twelve patients (2.3%) died with functioning grafts, 50 (9.5%) died on dialysis, after graft failure. Causes of death of patients who died with functioning grafts included post-transplant lymphoproliferative disease (5), cardiovascular complications (3), sepsis (2), and cytomegalovirus pneumonitis (1). One patient was killed by a terrorist attack. The cumulative patient survival rates were 94.8% for LD and 89.9% for DD allograft recipients at 10 years and 91.4% and 80.2% at 20 years, respectively (p = 0.005) (Fig. 1). Following both LD and DD transplants, 7-year patient survival rates were significantly (p < 0.001) lower in the first decade (82.4%) than in the second, third, and fourth periods: 91.0%, 96.8%, and 97.7%, respectively. In a multivariable regression model for all-cause mortality, the HR of transplantation between 1981 and 1990 compared with 2011–2017 was 5.03 (1.37–18.41, p = 0.015). The HR for survival following DD compared with LD transplantation was 2.05 (95%CI: 1.02–4.11, p = 0.044).
The 5-year and 10-year graft survival rates were 87.9% and 75.2% for LD and 77.0% and 60.7% for DD grafts, respectively. Figure 2 shows the Kaplan-Meier death-censored survival curves: 47.0% for LD and 38.4% for DD over 20 years: 44.6% for LD and 26.4% for DD over 25 years. The estimated half-life for LD transplants is 225 months (18.75 years), and for DD transplants, 179 months (14.9 years).
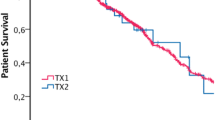
Graft survival improved significantly (p < 0.001) over time for both LD and DD transplantations. Over the four periods analyzed, 7-year graft survival increased for LD graft recipients 59.3%, 83.6%, 81.7%, and 92.0% (Fig. 3a); and for the DD graft recipients: 39.5%, 76.5%, 76.6%, and 71.3% (Fig 3b). In a multivariable proportional hazards Cox regression for graft survival, the HR of transplantation in the first decade compared with 2011–2017 was 3.04 (1.72–5.36, p < 0.001). The HR for DD compared with LD graft survival was 1.53 (95%CI: 1.15–2.03, p = 0.004).
Ten-year graft survival did not differ significantly between Arab (65.3%) and Jewish (67.4%) children, p = 0.621 (Fig. 4). No significant (p = 0.709) difference was found in 10-year graft survival among the age groups of kidney transplant recipients: < 3 years, 78.7%; 3–6 years, 67.3%; 7–11 years, 63.0%; 12–19 years, 66.8%. No significant (p ≥ 0.2) association was found between patient's sex or ethnicity, or their interaction with patient and graft survival.
During the 37-year study period, 248 transplants were lost (41.1%). The leading cause of graft failure was chronic allograft nephropathy (53.6%); additional causes were acute rejection (12.5%) and recurrence of primary kidney disease, primarily focal segmental glomerulosclerosis (10.9%). Loss of grafts from acute rejection and recurrent disease decreased in frequency over the decades. Acute rejection and chronic allograft nephropathy accounted for 4.8% and 59.0%, respectively, of LD graft failure and 10.3% and 50.9%, respectively, for DD graft failure. These differences were insignificant (p = 0.254).
Discussion
To the best of our knowledge, this is the largest reported single-center cohort of pediatric kidney transplantation covering almost four decades of experience. We report very good patient survival rates of 94.8% for LD and 89.9% for DD allograft recipients at 10 years and 91.4% and 82.2%, respectively, at 20 years. These results compare favorably to those reported in the USA by the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS): 10-year patient survival of 92.4% for LD grafts and 86.6% for DD grafts [18], and those reported by other centers around the world. A recently published review from the UK, of transplantations performed during 1992–2016, showed 10-year and 20-year patient survival of 94% and 84%, respectively [2]. A Japanese series that reported mostly LD graft recipients noted 10- and 20-year patient survival rates of 93% and 88%, respectively [4].
In our study, 10- and 20-year graft survival were 75.2% and 47.4% for LD and 60.7% and 38.4% for DD grafts, with respective estimated half-lives of 18.8 years and 14.9 years. Other long-term studies, which mainly comprised data from earlier periods: the 1970s and before the year 2000 [19, 20], reported significantly lower rates. However, more recent studies show results more similar to ours. These include 10-year LD graft survival rates of 59% in Norway [21] and 74% in the UK and Japan [2, 4], and a 20-year rate of 42% in the UK [2]. For DD grafts, 10-year survival was reported at 72% in Portugal and France and 61% in the UK [2, 6, 7]. The data from the Scientific Registry of Transplant Recipients (SRTR) in the USA showed 10-year graft survival of 70.3% for LD and 60.6% for DD transplantations performed in 2007–2008 [22].
Significant improvement in graft survival was achieved in our patients over time. Seven-year graft survival for LD kidneys increased from 59.3% for the first decade of our study to as high as 92.0% in 2011–2017. Improved 7-year survival was also seen among recipients of DD grafts, from 39.5% for the first decade to over 71% from the second decade onward. The graft survival rate at our national center compares favorably with the recently reported data from the (NAPRTCS) registry: 7-year survivals of 86.2% and 75.6% for LD and DD transplants, respectively [1].
As has been reported previously, the improvement observed over time might be attributable to the accumulated experience in the field. This includes implementation of more potent immunosuppressive protocols; the use of virtual cross-match in non-sensitized recipients, which reduced cold ischemic time; improved infection prophylaxis, surveillance and management; and increased use of early diagnostic biopsies, together with early aggressive treatment of both cellular and humoral rejection [1,2,3, 7, 23]. Chronic allograft nephropathy remains the major cause of graft loss in our patients, as has been widely reported elsewhere.
Hereditary diseases were more prevalent as a KF etiology in our cohort, representing 25% of all causes, compared with 11.2–15.1% elsewhere [4, 19, 20]. The high incidence of hereditary causes of KF in the Israeli population is probably related to the high incidence of consanguinity, especially in the Arab minority [24, 25].
We did not find an association of recipients’ age at transplantation with graft survival. This differs from data of the NAPRTCS and SRTR [5, 18, 26], which show poorer long-term graft survival among adolescents than among younger recipients. The proposed explanation for such is greater incidence of non-adherence reported among adolescents in those studies. In our series, the overall rate of graft loss for non-adherence was only 5.6%. We did not observe a considerable difference in adherence for adolescent patients, nor was this reported in studies from centers in the UK [2] or Japan [4]. Differences in outcomes may be related to cultural differences. Increased parental supervision, extending into adult life in a more traditional culture, may explain the more favorable outcomes in our teenage group, compared with other studies. Moreover, the Israeli social health system, which covers all health care expenses, including medications and clinical visits, regardless of socioeconomic status, may also play a role.
We report better outcomes of LD than DD transplants, corroborating with most reports. The proportion of LD transplants in our cohort, 42.2%, is similar to the 36–40% rate recently reported in the USA [1, 22], and substantially lower than the 80% rate reported in some European centers [6]. The dearth of living donors in Israel results in a rather long waiting time of 17 months. In recent years, we noted an increasing proportion of living donation, reaching 54.3%. This is expected to reduce waiting time and further improve results. The proportions of living donation in the Arab population remains considerably lower. The overall increase in living donation is presumably related to changes in the law regulating organ donation in 2008. In that year, the Knesset (Israeli Parliament) approved two laws aimed to facilitate organ transplantation: the first clarifies the definition of brain-respiratory death [27]; the second provides reimbursements of medical expenses, lost work compensation up to 18,000 NIS (roughly US$5,000), and priority on the transplant list should donors require a future organ donation. In addition, the law criminalizes organ trafficking, receiving compensation for organs, and acting as an organ broker [28]. Two other factors that have contributed to the rise in LD transplants are: an increase in altruistic donors, who now comprise 50% of the LD pool, and the introduction of a pair exchange program that enables non-matched parents to indirectly donate kidneys to their children.
We report equal access to deceased donor kidneys for the Arab minority and Jewish majority, concurring with an earlier Israeli study that investigated an 11-year period [29]. The mean waiting time of Arab children on dialysis for a deceased donor kidney transplant was not significantly different from the waiting time of Jewish children. Furthermore, our data show similar graft survival after transplantation between the majority and minority populations in our country. In contrast, African Americans, including African American children, have been reported to wait longer for deceased donor kidneys in the USA [8,9,10,11], as do the Maori in New Zealand [13]. Although graft survival has improved among African American children, they were reported to continue to lag behind their Caucasian peers by as much as 20% after 5 years [9]. A large recently published European study showed that black and Asian children and adolescents were about half as likely to receive kidney transplants as white patients; the risk of death was 2.5-fold higher in transplanted Asian patients than in white patients [12]. Several factors have been proposed to explain the differences in both access to grafts and to graft survival in the USA. These include socioeconomic factors that influence the access to medical services, low rates of African American organ donation, high rates of KF that increase immunological incompatibility, genetic factors that may increase the risk of rejection, and institutional racism [30]. The equality of access to DD kidneys of the Israeli Arab minority and equality of graft survival may be attributed to the non-discriminating social health care system in Israel, which provides coverage of immunosuppressive medication and other drugs after transplantation. Genetic similarities of the two populations, Arabs and Jews, which lead to similarities in immunologic responses, may also explain comparable results.
Conclusion
We report results of 37-year experience of the national pediatric kidney transplant program in Israel. Long-term, 12-year median follow-up shows high patient and graft survival with LD and DD kidneys, comparable with data reported by US consortium and European series. Continuously improving results reached a 7-year graft survival rate of 92% for LD and 71% for DD transplants. Ethnic disparities were not observed between Jewish and Arab children, regarding access to transplants and outcomes after transplantation, despite differences in disease prevalence and in living donation.
Data availability
The authors will provide access to data upon reasonable request.
References
Chua A, Cramer C, Moudgil A, Martz K, Smith J, Blydt-Hansen T, Neu A, Dharnidharka VR (2019) NAPRTCS investigators. Kidney transplant practice patterns and outcome benchmarks over 30 years: the 2018 report of the NAPRTCS. Pediatr Transplant 23:e13597
Mumford L, Maxwell H, Ahmad N, Marks SD, Tizard J (2019) The impact of changing practice on improved outcomes of paediatric renal transplantation in the United Kingdom: a 25 years review. Transpl Int 32:751–761
Francis A, Johnson DW, Melk A, Foster BJ, Blazek K, Craig JC, Wong G (2020) Survival after kidney transplantation during childhood and adolescence. Clin J Am Soc Nephrol 15:392–400
Aoki Y, Hamasaki Y, Satoh H, Matsui Z, Muramatsu M, Hamada R, Ishikura K, Hataya H, Honda M, Sakai K, Shishido S (2020) Long-term outcomes of pediatric kidney transplantation: a single-center experience over the past 34 years in Japan. Int J Urol 27:172–178
Van Arendonk K, Boyarsky BJ, Orandi BJ, James NT, Smith JM, Colombani PM, Segev DL (2014) National trends over 25 years of pediatric kidney transplant outcomes. Pediatrics 133:594–601
Branco F, Almeida F, Cavadas V, Ribeiro S, Osório L, Rocha A, Ramos M, Martins L, Dias L, Castro-Henriques A, Mota C, Reis A, Fraga A (2013) Pediatric kidney transplantation: a single center experience with 134 procedures. Transplant Proc 45:1057–1059
Harambat J, Ranchin B, Bertholet-Thomas A, Mestrallet G, Bacchetta J, Badet L, Basmaison O, Bouvier R, Demède D, Dubourg L, Floret D, Martin X, Cochat P (2013) Long-term critical issues in pediatric renal transplant recipients: a single-center experience. Transpl Int 26:154–161
Patzer RE, Sayed BA, McClellan WM, Kutner N, Amaral S (2013) Racial and ethnic differences in pediatric access to preemptive kidney transplantation in the United States. Am J Transplant 13:1769–1781
Patzer RE, Mohan S, Kutner N, McClellan WM, Amaral S (2015) Racial and ethnic disparities in pediatric renal allograft survival in the United States. Kidney Int 87:584–592
Ku E, McCulloch CE, Grimes BA, Johansen KL (2017) Racial and ethnic disparities in survival of children with ESRD. J Am Soc Nephrol 28:1584–1591
Laster M, Sohoo M, Hall C, Streja E, Rhee C, Ravel V, Reddy U, Norris K, Salusky I, Kalantar-Zadeh K (2017) Racial-ethnic disparities in mortality and kidney transplant outcomes among pediatric dialysis patients. Pediatr Nephrol 32:685–695
Tjaden LA, Noordzij M, van Stralen KJ, Kuehni CE, Raes A, Cornelissen EAM, O’Brien C, Papachristou F, Schaefer F, Groothoff JW, Jager KJ (2016) Racial disparities in access to and outcomes of kidney transplantation in children, adolescents and young adults: results from the ESPN/ERA- EDTA. Am J Kidney Dis 67:293–301
Dittmer I, Wilkinson M (2014) Racial disparities in pediatric kidney transplantation in New Zealand. Pediatr Transplant 18:689–697
Israel Central Bureau of Statistics. Monthly Bulletin of Statistics – April 2020. https://www.cbs.gov.il/he/publications/doclib/2020/yarhon0420/b1.pdf. Accessed 16 Jan 2021
Israel Center for Disease Control. Ministry of Health. ESRD Registry. https://www.health.gov.il/English/MinistryUnits/ICDC/disease_Registries/Pages/Alternative_kidney_treatment.aspx. Accessed 16 Jan 2021
Jamieson NV (2005) A 20-year experience of combined liver/kidney transplantation for primary hyperoxaluria (PH1): the European PH1 transplant registry experience 1984-2004. Am J Nephrol 25:282–289
Collaborative Transplant Study. https://www.ctstransplant.org/public/participants/regionMes.shtml. Accessed 16 Jan 2021
Smith JM, Martz K, Blydt-Hansen TM (2013) Pediatric kidney transplant practice patterns and outcome benchmarks, 1987-2010: a report of the North American Pediatric Renal Trials and Collaborative Studies. Pediatr Transplant 17:149–157
Rees L, Shroff R, Hutchinson C, Fernando ON, Trompeter RS (2007) Long-term outcome of paediatric renal transplantation: follow-up of 300 children from 1973 to 2000. Nephron Clin Pract 105:c68–c76
Groothoff JW, Cransberg K, Offringa M, van de Kar NJ, Lilien MR, Davin JC, Heymans HAS, Dutch cohort study (2004) Long-term follow-up of renal transplantation in children: a Dutch Cohort Study. Transplantation 78:453–460
Tangeraas T, Bjerre A, Lien B, Kyte A, Monn E, Cvancarova M, Leivestad T, Reisaeter AV (2008) Long-term outcome of pediatric renal transplantation: the Norwegian experience in three eras 1970–2006. Pediatr Transplant 12:762–768
Hart A, Smith JM, Skeans MA, Gustafson SK, Wilk AR, Castro S (2020) OPTN/SRTR 2018 Annual Data Report: Kidney. Am J Transplant 20(Suppl s1):20–130
Holmberg C, Jalanko H (2016) Long term effects of pediatric kidney transplantation. Nat Rev Nephrol 12:301–311
Jaber L, Halpern GJ (2006) Consanguinity among the Arab and Jewish populations in Israel. Pediatr Endocrinol Rev Suppl l3:437–446
Na'amnih W, Romano-Zelekha O, Kabaha A, Rubin LP, Bilenko N, Jaber L, Honovich M, Shohat T (2015) Continuous decrease of consanguineous marriages among Arabs in Israel. Am J Hum Biol 27:94–98
Andreoni KA, Forbes R, Andreoni RM (2013) Age-related kidney transplant outcomes: health disparities amplified in adolescence. JAMA Intern Med 173:1524–1532
Cohen J, Ashkenazi T, Katvanc E, Singera P (2012) Brain death determination in Israel: the first two years experience following changes to the brain death law—opportunities and challenges. Am J Transplant 12:2514–2518
Lavee J, Ashkenazi T, Stoler A, Cohen J, Beyar R (2013) Preliminary marked increase in the national organ donation rate in Israel following implementation of a new organ transplantation law. Am J Transplant 13:780–785
Drukker A, Feinstein S, Rinat C, Rotem-Braun A, Frishberg Y (2003) Cadaver-Donor renal transplantation of children in Israel (1990-2001): racial disparities in health care delivery? Pediatrics 112:341–344
Darnidharka VR, Selfert ME (2015) Kidney transplant results in children: progress made, but blacks lag behind. Kidney Int 87:492–494
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All authors approved the final draft of the manuscript and agree to be accountable for all aspects of the work.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study was approved by the Institutional Research Ethics Board of Rabin Medical Center and Schneider Children’s Medical Center of Israel.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Davidovits, M., Reisman, L., Cleper, R. et al. Long-term outcomes during 37 years of pediatric kidney transplantation: a cohort study comparing ethnic groups. Pediatr Nephrol 36, 1881–1888 (2021). https://doi.org/10.1007/s00467-020-04908-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04908-6