Abstract
Background
There are currently three distinct autosomal recessive inherited types of primary hyperoxaluria (PH: PHI, PHII, and PHIII), all characterized by the endogenous overproduction of oxalate. The PH type is difficult to differentiate by clinical features alone. In addition to universal general characteristics to all hyperoxaluria subtypes, specific urinary metabolites can be detected: glycolate in PHI, L-glyceric acid in PHII, and hydroxy-oxo-glutarate (HOG) in PHIII. PHIII is considered to be the most benign form and is characterized by severe recurrent urolithiasis in early life, followed by clinical remission in many, but not all patients. We examined urinary HOG (UHOG) excretion as a diagnostic marker and its correlation to progression of the clinical course of PHIII.
Methods
UHOG was analyzed by combined ion chromatography/mass spectrometry (IC/MS) in urine samples from 30 PHIII and 68 PHI/II patients and 79 non-PH hyperoxaluria patients.
Results
Mean UHOG excretion was significantly higher in patients with PHIII than in those with PHI/II and in non-PH patients(51.6 vs. 6.61 vs. 8.36 μmol/1.73 m2/24 h, respectively; p<0.01).
Conclusions
Significantly elevated UHOG excretion was exclusively seen in PHIII patients and showed a 100 % consensus with the results of hydroxy-oxo-glutarate aldolase (HOGA1) mutational analysis in newly diagnosed patients. However, UHOG excretion did not correlate with clinical course on follow-up and could not be used to discriminate between active stone formers and patients with a clinically uneventful follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary hyperoxaluria (PH) is a severe kidney stone disease that frequently results in recurrent stone formation, renal failure, and multisystemic disease [1, 2]. Three types of PH have been identified to date (PHI, PHII, PHIII), with all types characterized by defective glyoxylate metabolism that results in significant endogenous overproduction of oxalate and thus elevated urinary excretion of oxalate. The clinical hallmarks of the disease are recurrent urolithiasis and/or progressive nephrocalcinosis [3,4,5]. Although each type of PH differs in terms of clinical and laboratory features, there is a large overlap of symptoms and signs which makes differentiation on clinical and biochemical bases alone challenging.
The genetic basis of PHIII (OMIM 613616) is loss of function mutations in the hydroxy-oxo-glutarate aldolase 1 gene (HOGA1) that codes for an enzyme which plays an important role in hydroxyproline metabolism in liver mitochondria [6,7,8]. The lack of HOGA1 enzymatic activity leads to a high amount of hydroxy-oxo-glutarate (HOG), which leaks from the mitochondria into the cytosol, where it is believed to inhibit the action of glyoxylate-reductase/hydroxypyruvate reductase (GRHPR; defective in PHII). Inhibition of GRHPR makes more glyoxlyate precursor available for oxalate generation, thus leading to significant hyperoxaluria (>1 mmol/1.73 m2/day) [6, 7, 9].
Patients with PHIII typically present with (severe) recurrent kidney stone passages, often as soon as in early infancy [4, 5, 8, 9], which frequently lead to invasive stone removal procedures. The clinical difference between PHIII and the two other forms of PH is the decline in severity of clinical symptoms over time [1, 4, 5, 8]. Moreover, to date only one patient with PHIII with end stage renal disease (ESRD) has been reported to date [10], which is quite different to PHI (with patients having approx. a 100 % risk of ESRD over time) [3, 7, 9] and PHII (approx. 20% risk of ESRD) [11].
Next to the clinical course, urinary excretion parameters may better help to differentiate between types. In PHI (OMIM 259900), which is caused by a lack of liver-specific alanine:glyoxylate aminotransferase [2, 12], urinary glycolate excretion is also elevated in most patients [4]. PHII (OMIM 260000) patients have a reduced activity of glyoxylate/hydroxypyruvate reductase, leading to an elevated urinary excretion of L-glyceric acid in most patients [4, 13]. Although urinary calcium excretion is typically low in patients with PHI/II, this may not be the case in those with PHIII who may demonstrate levels in the upper normal range or even hypercalciuria, while hyperuricosuria is occasionally observed [6, 7, 14].
It has been reported that both urinary hydroxy-oxo-glutarate (UHOG) and glutamate concentration and excretion are increased in patients with PHIII [6, 15, 16]. In the study reported here we examined UHOG concentrations to establish a diagnostic marker for PHIII in our laboratory. We also looked at whether changes in the UHOG excretion pattern could possibly serve as a prognostic marker.
Materials and methods
A total of 30 patients with PHIII, 65 with PHI, and three with PHII, as well as a control group of 79 non-PH-patients with secondary or unclassified hyperoxaluria, were enrolled in this study. All patients had been completely genotyped for the three known PH genes: AGXT, GRHPR, and HOGA1 by Sanger sequencing. We analyzed the first urine samples collected after presentation in our outpatient clinic for HOG as well as the follow-up urine samples for all PHIII patients. In total, 280 urine samples (88 spot urine samples and 192 twenty-four-hour urine samples) of 177 patients were collected and analyzed using an ion chromatography/mass spectroscopy (IC/MS) method: 69 samples from PHI/II patients, 110 samples from PHIII patients, and 101 urine samples from non-PH patients. Long-term follow-up data were available for 29 PHIII patients. Mean patient age was 16.6, 6.8, and 9.3 years for patients with PHI and II, patients with PHIII, and non-PH patients.
Adequate urine preservation was necessary to ensure the stability of UHOG over time. Preparation of urine specimens (24-h urine samples, spot urine samples) included acidification with HCl to a pH of <1.5 directly after collection. The acidified samples were frozen promptly after preparation if not directly analyzed. For analysis, samples were diluted 100× with 0.20 M boric acid solution. The IC/MS system used (ICS 3100 ion chromatography system and MSQ+ mass spectrometer; Thermo Fisher Scientific, Waltham, MA) was equipped with an analytical column (AS11, high efficiency) and a guard column (AG11) as the stationary phase. For the mobile phase, KOH (Thermo Fisher Scientific; 3 KOH eluent generator cartridge) with a gradient of 5 mM gradually ramping to 100 mM was used in the IC. The flow rate was set at 0.3 ml/min and the ramping included the following steps: 5 mM concentration until min 5.9, followed by a linear gradient from 5 to 52.5 mM until min 21; thereafter a 100 mM concentration was set until min 24.2 after which, the concentration went back to 5 mM until 38 min.
The system was calibrated using five standards of increasing concentrations of HOG (0.05, 0.125, 0.25, 0.4, and 0.5 μmol). The HOG used for calibration was purchased from Santa Cruz Biotechnology (Dallas, TX). The M/S was calibrated to a span of 0.30 m/z at 161 m/z, negative polarity, dwell time of 0.5s, cone voltage of 25V, and a probe temperature of 450°C for optimal HOG detection.
Statistical analysis was performed using SPSS statistics (IBM Corp., Armonk, NY). A p value of <0.05 was considered to be significant.
Results
Our IC/MS assay allowed a rapid identification of the metabolite HOG in urine samples with a between-run coefficient of variation for urine HOG analysis of 0.15, repeated 100 times. Multiple evaluations of individual samples revealed a high degree of reproducibility. Multiple determinations of samples + added HOG concentrations (1, 2, and 5 μmol/l) yielded showed complete agreement with the added measured concentrations. The lower limit of detection was 0.03 μmol/l.
UHOG concentrations and especially UHOG excretion and the HOG/creatinine ratio enabled PHIII patients to be discriminated from PHI and PHII patients, and non-PH patients. The Mean UHOG excretion from all primary urine samples of PHIII patients taken at first presentation [68.91 (range 9.29–340.09) μmol/1.73 m2/24 h] was substantially higher than those of PHI/II patients [6.61 (range 0.64–14.93) μmol/1.73 m2/24 h] and non-PH patients with hyperoxaluria [mean 8.73 (range 0.06–24.11) μmol/1.73 m2/24 h (p < 0.01) (Table 1).
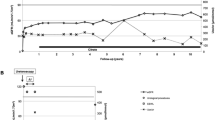
For the 24-h urine samples in the follow-up examinations (n = 139), mean UHOG excretion was 6.61 μmol/1.73 m2/day in patients with PHI/II (n = 34 samples) and 8.34 μmol/1.73 m2/day for non-PH patients (n = 58 samples). In PHIII patients, mean UHOG excretion was fivefold higher (51.6 μmol/1.73 m2/24 h; p < 0.01, n=47 samples), as graphically demonstrated in Fig. 1a.
a Hydroxy-oxo-glutarate (HOG) excretion for the different patient groups (PH1, PH2, PH3 primary hyperoxaluria types I, II, and III, non-PH non-PH patients) on log scale for 24-h urine samples. b HOG/creatinine ratio (n = 79; in μmol/μmol) for PHI/II and PHIII patients and non-PH patients on log scale for spot urine samples
As occurs with many urinary metabolites, we observed heterogeneity in HOG excretion in PHIII and non-PH patients (range 0.063–340.09 μmol/1.73 m2/24 h), such that low UHOG excretion in PHIII patients overlapped with comparatively high UHOG excretion in PHI/II and non-PH patients. The lower HOG values measured in PHIII patients were obtained at follow-up and not at the time of diagnosis.
We calculated the HOG/creatinine ratio (μmol/μmol) of all spot urine samples (n = 79 with available creatinine levels). It was over tenfold higher in PHIII patients (3.73, range <0.01-25.68) than in PH I/II patients (0.27, range 0.05–1.0) or in non-PH patients (0.05–0.52), respectively (p < 0.05). The mean HOG/creatinine ratio for all urine samples (spot and 24-h urine samples) for which HOG and creatinine levels were available(n = 224) were also substantially higher in PHIII patients (2.1, range <0.001-25.68) than in PHI/II patients (0.11; range 0.007–1.0) and in non-PH patients (< 0.001–0.52), respectively (p < 0.05 (Fig. 1b).
Sensitivity for UHOG concentration as a screening parameter in the urine samples was 76.7% for a cutoff value of 10 μmol/l, and the specificity was 100% tested for all first urine samples collected after first presentation (positive predictive value: 100%; negative predictive value: 94.7%). UHOG excretion with a cutoff value of 24 μmol/1.73 m2/24 h showed a specificity of 99% and a sensitivity of 75%; for a HOG/creatinine ratio with a cut-off value of 0.3 μmol/μmol, the results were comparable with a sensitivity of 66% and a specificity of 95%.
The receiver operating characteristic (ROC) curve analysis showed an area under the curve of 0.92 for HOG excretion, 0.89 for UHOG concentration (μmol/l) and 0.89 for the HOG/creatinine ratio (Fig. 2). UHOG concentration in our follow-up PHIII cohort (n = 29) ranged from 3.58 to 116.41 (median 17.0) μmol/l, and the HOG/creatinine ratio (n = 25) ranged from 0.11 to 8.31 (mean value 1.12) μmol/μmol. There was no correlation between UHOG concentrations and urinary oxalate concentration in the same urine samples (log Pearson-correlation 0.138), nor between UHOG and patient age (Fig. 3).
There were no significant changes in the results when the cohort was divided into active stone former (AS), i.e., those patients who either showed ongoing stone passages or developed new stones, as shown in imaging procedures (urolithiasis, n = 8), and patients in clinical remission (CR; completely asymptomatic or asymptomatic stones in situ, n=21). UHOG excretion levels in 24-h urine samples were analyzed in 18 PHIII patients in follow-up consultations, with levels ranging from 16.8 to 340.1 μmol/1.73 m2/24 h. There was no significant difference in HOG excretion levels among AS and CR patients (p = 0.14), although the mean UHOG in AS was 146.25 μmol/1.73 m2/24 h (n = 6) compared to 39.54 μmol/1.73 m2/24 h in CR patients (n = 12) (Fig. 4).
Analysis of the HOG/creatinine ratio (n = 25) also did not reveal any significant difference between AS and CR patients (mean ratio 1.4 vs. 0.99 μmol/μmol, respectively, p = 0.5). Mean estimated glomerular filtration rate (eGFR) was comparable between groups (105.2 ml/min in AS vs. 118.4 ml/min in CR).
Within our PHIII cohort we detected five new HOGA1 mutations (c.206T>G [p.F69C], c.580G>A [p.G194S], c.209G>C [p.R70P], c.110G>A [p.G37D], c.634A>C [p.Thr212Pro], and c.661G>C [p.Ala221Pro] on the same parental allele) and reconfirmed some of the previously identified private mutations from other groups. Initial complaints of the follow-up cohort (n = 29) were urolithiasis or suspected urinary tract infection in most of the patients. In the long-term follow up (mean 6.04 years, range 1–17 years) 55% of patients showed complete clinical remission. The main stone removal procedure was lithotripsy, which was frequently performed multiple times (Table 2).
Four patients developed chronic kidney disease (CKD) stages 2–3 (GFR 53-89 ml/min per 1.73 m2, calculated by the Schwartz formula), which may be due to the underlying severe hyperoxaluria per se. However, all four patients underwent repeated stone removal procedures, mostly lithotripsies (between >2 and 16 times), which normally is regarded as an obsolete method in a patient with PH. Overt nephrocalcinosis was not found in any of these patients. All other patients in the follow-up with a better eGFR (range 95–185 ml/min), had only undergone ≤2 stone removal procedures.
Discussion
We successfully established an easy and reliable urine screening test to better evaluate patients with PHIII in our laboratory. We were able to prove that analysis of UHOG provided significant evidence for type III PH, which was later verified by genetic testing in all patients. Based on these results, increased UHOG can be regarded as a very useful parameter in addition to clinical signs (in our cohort mostly recurrent urolithiasis) and symptoms and other urinary excretion parameters (e.g. higher calcium and uric acid values) that may point to a diagnosis of PHIII [6]. In particular, the specificity of the analysis was high, suggesting a solid screening parameter. Therefore we now include UHOG in our random urine hyperoxaluria panel (in addition to oxalate, glycolate, and glyceric acid). However, there was no specific correlation of UHOG with urinary oxalate excretion, age of patients, clinical severity and especially follow-up.
We observed a HOG excretion threshold of 24 μmol/1.73 m2/24 h and a HOG/creatinine ratio of 0.3 to be a very conservative (cutoff) values for the diagnosis of PHIII.
In two asymptomatic siblings of an index case, UHOG excretion data provided evidence of subclinical PHIII, which was then genetically proven. In two new patients, HOG/creatinine ratios of 4 and 21 led us to suspect PHIII, which was then also proven by genetic testing.
Taking the different therapeutic regimens and prognosis for each PH type into consideration, a more rapid and disease-specific intervention is possible with adequate diagnostic evaluation. In PH type I disease, vitamin B6 medication leads to a decrease in endogenous oxalate production in around 30 % of patients [17, 18]. This, however, is not a therapeutic option in patients with PH type III disease and might even lead to severe side effects (neurologic, acne and, recent personal experience, depression) in these patients. In patients with PHIII a high fluid intake and measures to increase urinary solubility, such as by alkaline citrate, are currently the only treatment options [19, 20].
In our cohort of 29 patients with a long-term follow up, four patients developed CKD stages 2–3 (GFR 53–89 ml/min per 1.73 m2, calculated by the Schwartz formula), but no ESRD. All of these patients had undergone repeated stone removal procedures (mostly lithotripsies, with up to 16 lithotripsies in a young boy and 13 in a young girl), but no overt nephrocalcinosis was observed in the imaging procedures. This is in context to a recently published study by Allard et al. who also reported GFR impairment in two out of seven PHIII patients (GFR 77 and 83 ml/min per 1.73 m2) [21]. It has to be kept in mind that lithotripsy is normally regarded as an obsolete maneuver for stone removal in patients with PH, even if no problematic nephrocalcinosis is seen on ultrasound scans.
The first PHIII patient with ESRD was recently reported [10, 22], suggesting that PHIII may not be as clinically benign as previously thought. However, the underlying reason of the decline in kidney function remains unclear. Speculatively speaking, it may not be hyperoxaluria or urolithiasis per se, but the repeated stone removal procedures [10, 21]. Therefore, we suggest that each stone removal procedure should be carefully evaluated and discussed to avoid potential additional damage.
We did not find sound evidence that the level of UHOG excretion relates to the clinical course and serves as a first prognostic marker of why most of the patients remain clinically silent in the long run. Nevertheless, in some patients consistently higher UHOG values were observed with ongoing urolithiasis, while other patients who were in complete clinical remission demonstrated low UHOG levels. However, this was not the case in all patients. Also, we did not find a significant difference in UHOG between those patients with ongoing development of kidney stones and/or repeated stone passages (= acute stone formers) and those in clinical remission (no further stone development in imaging studies, no passage of stones).
It can be speculated that differences in nutrition may be the most important parameter leading to a change in clinical severity of the disease, as the hydroxyproline (animal protein) metabolism is hampered [23]. However, the persisting hyperoxaluria in all PH patients, mostly in the same range over all age groups and independent of the change in diet from early infancy to young adulthood, may make further evaluations necessary.
In conclusion, if urine specimens are adequately preserved directly after collection, UHOG levels provide the first evidence that the patient with recurrent kidney stones and severe hyperoxaluria may have PHIII. However, neither a true correlation of UHOG with clinical follow-up nor a differentiation between active stone formers and patients with a clinically silent follow-up was apparent in our patient cohort, which is the largest cohort of PHIII patients studied to date. The clinical outcome of PHIII is—keeping in mind that data are available from only a limited number of patients over a relatively short period of time—mainly favorable although significant hyperoxaluria persists [3, 6,7,8]. However, a potential impairment in kidney function has also been observed, thereby providing evidence that PHIII is clearly not as unproblematic in the long run as previously thought [10, 21].
Change history
10 April 2018
The unit of the HOG-creatinine ratio presented in this article is calculated in μmol/mg creatinine instead of the demonstrated unit of μmol/μmol. This applies to the parameter in the text of the article and the labeling of Figs. 1, 2b and 3c.
References
Hoppe B, Beck BB, Milliner DS (2009) The primary hyperoxalurias. Kidney Int 75:1264–1271
Archer HE, Dormer AE, Scowen EF, Watts RW (1957) Primary hyperoxaluria. Lancet 273:320–322
Hoppe B (2012) An update on primary hyperoxaluria. Nat Rev Nephrol 8:467–475
Milliner DS, Harris PC, Lieske JC (2015) Primary hyperoxaluria type 3. In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH, Bird TD, Ledbetter N, Mefford HC, Smith RJH, Stephens K (eds) Gene reviews, University of Washington, Seattle
Cochat P, Rumsby G (2013) Primary hyperoxaluria. N Engl J Med 369:649–658
Monico CG, Rossetti S, Belostotsky R, Cogal AG, Herges RM, Seide BM, Olson JB, Bergstrahl EJ, Williams HJ, Haley WE, Frishberg Y, Milliner DS (2011) Primary hyperoxaluria type III gene HOGA1 (formerly DHDPSL) as a possible risk factor for idiopathic calcium oxalate urolithiasis. Clin J Am Soc Nephrol 6:2289–2295
Belostotsky R, Seboun E, Idelson GH, Milliner DS, Becker-Cohen R, Rinat C, Monico CG, Feinstein S, Ben-Shalom E, Magen D, Weissman I, Charon C, Frishberg Y (2010) Mutations in DHDPSL are responsible for primary hyperoxaluria type III. Am J Hum Genet 87:392–399
Beck BB, Baasner A, Buescher A, Habbig S, Reintjes N, Kemper MJ, Sikora P, Mache C, Pohl M, Stahl M, Toenshoff B, Pape L, Fehrenbach H, Jacob DE, Grohe B, Wolf MT, Nürnberg G, Yigit G, Salido EC, Hoppe B (2013) Novel findings in patients with primary hyperoxaluria type III and implications for advanced molecular testing strategies. Eur J Hum Genet 21:162–172
Belostotsky R, Pitt JJ, Frishberg Y (2012) Primary hyperoxaluria type III—a model for studying perturbations in glyoxylate metabolism. J Mol Med (Berl) 90:1497–1504
Hopp K, Cogal AG, Bergstralh EJ, Seide BM, Olson JB, Meek AM, Lieske JC, Milliner DS, Harris PC (2015) Rare kidney stone consortium phenotype-genotype correlations and estimated carrier frequencies of primary hyperoxaluria. J Am Soc Nephrol 26:2559–2570
Kemper MJ, Conrad S, Muller-Wiefel DE (1997) Primary hyperoxaluria type 2. Eur J Pediatr 156:509–512
Danpure CJ, Jennings PR, Watts RW (1987) Enzymological diagnosis of primary hyperoxaluria type 1 by measurement of hepatic alanine: glyoxylate aminotransferase activity. Lancet 1:289–291
Milliner DS, Wilson DM, Smith LH (2001) Phenotypic expression of primary hyperoxaluria: comparative features of types I and II. Kidney Int 59:31–36
Jacob DE, Grohe B, Geßner M, Beck BB, Hoppe B (2013) Kidney stones in primary hyperoxaluria: new lessons learnt. PLoS One 8:e70617
Pitt JJ, Willis F, Tzanakos N, Belostotsky R, Frishberg Y (2015) 4-hydroxyglutamate is a biomarker for primary hyperoxaluria type 3. JIMD Rep 15:1–6
Riedel TJ, Knight J, Murray MS, Milliner DS, Holmes RP, Lowther WT (2012) 4-Hydroxy-2-oxoglutarate aldolase inactivity in primary hyperoxaluria type 3 and glyoxylate reductase inhibition. Biochim Biophys Acta 1822:1544–1552
Toussaint C (1998) Pyridoxine-responsive PH1: treatment. J Nephrol 11[Suppl 1]:49–50
Milliner DS, Eickholt JT, Bergstralh EJ, Wilson DM, Smith LH (1994) Results of long-term treatment with orthophosphate and pyridoxine in patients with primary hyperoxaluria. N Engl J Med 331:1553–1558
Leumann E, Hoppe B, Neuhaus T (1993) Management of primary hyperoxaluria: efficacy of oral citrate administration. Pediatr Nephrol 7:207–211
Hamm LL (1990) Renal handling of citrate. Kidney Int 38:728–735
Allard L, Cochat P, Leclerc AL, Cachat F, Fichtner C, De Souza VC, Garcia CD, Camoin-Schweitzer MC, Macher MA, Acquaviva-Bourdain C, Bacchetta J (2015) Renal function can be impaired in children with primary hyperoxaluria type 3. Pediatr Nephrol 30:1807–1813
Zhao F, Bergstralh EJ, Mehta RA, Vaughan LE, Olson JB, Seide BM, Meek AM, Cogal AG, Lieske JC, Milliner DS (2016) Predictors of incident ESRD among patients with primary hyperoxaluria presenting prior to kidney failure. Clin J Am Soc Nephrol 11(1):119–126
Knight J, Jiang J, Assimos DG, Holmes RP (2006) Hydroxyproline ingestion and urinary oxalate and glycolate excretion. Kidney Int 70(11):1929–1934
Acknowledgments
We thank Przemyslaw Sikora (Lublin, Poland), Katarzyna Jobs (Warzaw, Poland), Marcin Zaniew, Lars Pape (Hannover, Germany), Burkhard Tönshoff (Heidelberg, Germany), Martin Bald (Stuttgart, Germany), Martin Pohl (Freiburg, Germany), Bärbel Lange-Sperandio (Munich, Germany), and Markus J. Kemper (Hamburg, Germany) for providing us with patient information and urine samples. We also thank B. Bär and D. Armborst (Germany) and F. Blanco (Spain) for extensive laboratory support. The work was partially supported by a grant from the German-Israeli Foundation (GIF) to (Bodo B. Beck & Bernd Hoppe)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the local ethics committee and all material was obtained after written informed consent.
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ventzke, A., Feldkötter, M., Wei, A. et al. Systematic assessment of urinary hydroxy-oxo-glutarate for diagnosis and follow-up of primary hyperoxaluria type III. Pediatr Nephrol 32, 2263–2271 (2017). https://doi.org/10.1007/s00467-017-3731-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3731-3