Abstract
Background
Clinical care decisions to treat chronic kidney disease (CKD) in a growing child must often be made without the benefit of evidence from clinical trials. We used observational data from the Chronic Kidney Disease in Children cohort to estimate the effectiveness of renin–angiotensin II–aldosterone system blockade (RAAS) to delay renal replacement therapy (RRT) in children with CKD.
Methods
A total of 851 participants (median age: 11 years, median glomerular filtration rate [GFR]: 52 ml/min/1.73 m2, median urine protein to creatinine ratio: 0.35 mg/mg) were included. RAAS use was reported at annual study visits. Both Cox proportional hazards models with time-varying RAAS exposure and Cox marginal structural models (MSM) were used to evaluate the effect of RAAS use on time to RRT. Analyses were adjusted or weighted to control for age, male sex, glomerular diagnosis, GFR, nephrotic range proteinuria, anemia, elevated blood pressure, acidosis, elevated phosphate and elevated potassium.
Results
There were 217 RRT events over a 4.1-year median follow-up. At baseline, 472 children (55 %) were prevalent RAAS users, who were more likely to be older, have a glomerular etiology, have higher urine protein, be anemic, have elevated serum phosphate and potassium, take more medications, but less likely to have elevated blood pressure, compared with non-users. RAAS use was found to reduce the risk of RRT by 21 % (hazard ratio: 0.79) to 37 % (hazard ratio: 0.63) from standard regression adjustment and MSM models, respectively.
Conclusions
These results support inferences from adult studies of a substantial benefit of RAAS use in pediatric CKD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children represent a small proportion of patients with chronic kidney disease (CKD), a disease estimated to affect 16 % of the general US population [1]. Small numbers of children with CKD contribute to the relative paucity of epidemiological and clinical trial data about progression and optimal treatment of CKD in this patient population. Clinicians are frequently left with little evidence to guide clinical decision-making.
Randomized controlled trial data in adults with CKD suggests that renin–angiotensin II–aldosterone system (RAAS) blockers, such as angiotensin-converting enzyme inhibitors (ACE-I) or angiotensin II receptor blockers (ARB), may slow CKD progression through blood pressure (BP) control and other BP-independent mechanisms [2–5]. To our knowledge, there are no comparable large-scale prospective studies in children to assess the efficacy of RAAS blockers in a pediatric CKD setting. Pediatric BP management guidelines for CKD patients recommend that an ARB or ACE-I be used in children for whom treatment with BP-lowering drugs is indicated, irrespective of the level of proteinuria [6]. However, the authors acknowledge that, “…limited direct evidence from clinical trials is available with which to assess the efficacy of RAAS in children with CKD.” The often-cited Effect of Strict Blood Pressure Control and ACE Inhibition on the Progression of Chronic Renal Failure in Pediatric Patients (ESCAPE) trial provided participants in both arms of the trial with a standardized dose of an ACE-I, and randomized participants to different levels of blood pressure control achieved with non-RAAS blockers [7]. Results from ESCAPE suggest that intensified BP control slowed the rate of progression to end-stage renal disease (ESRD); the effect of ACE-I/ARB use on the outcome was not directly assessed and was assumed to be beneficial.
The dearth of clinical trial data on RAAS blocker efficacy in children with CKD will likely persist, as a clinical trial that withholds ACE-I/ARB therapy would likely be considered unethical in the current era. This lack of direct evidence of continued benefit in patients with advanced stages of CKD leaves clinicians with little guidance on ACE-I/ARB therapy continuation for a pediatric patient when an increase in creatinine or serum potassium level is observed. Thus, additional evidence of benefit is needed and assessing the effectiveness of RAAS blockade in observational studies may provide the best available source to inform clinical care decisions and guideline development.
There are unique challenges in quantifying the effect of therapy in an observational study setting. Non-comparability of treated and untreated groups and dynamic use of therapy over time can introduce bias into analytical results. Facing these challenges, we examined the range of potential benefit associated with ACE-I/ARB therapy on time to the endpoint of dialysis or transplant in a large pediatric CKD cohort using both traditional adjustment and marginal structural models.
Materials and methods
Study sample
The Chronic Kidney Disease in Children (CKiD) study design and cohort characteristics have been described previously [8, 9]. In brief, patients 1–16 years of age with an estimated glomerular filtration rate (GFR) of 30 to 90 ml/min per 1.73 m2 were enrolled from 54 participating centers in North America.
Ascertainment of ACE-I/ARB use
As part of each annual study visit, children (and/or their parent or guardian) reported all prescribed medications taken by the child in the previous 30 days, including the frequency of each medication dose. Parents or guardians were asked to bring the child’s medications to the study visit for confirmation of medications by study staff. Use of ACE-I/ARBs between annual study visits was assumed to be consistent with that reported at the previous visit. Comparisons of ACE-I/ARB discontinuers with continued users was defined based on reported ACE-I/ARB status at the last contributing visit under observation, among those with at least one prior visit at which ACE-I/ARB use was reported.
Covariate measurement and definitions
Kidney function was assessed by determining GFR from plasma iohexol disappearance curves at study entry, 1 year later, and every other year thereafter using previously reported methods [10]. When GFR was not directly measured, it was estimated using published equations derived from the CKiD population [11]. In either case, GFR was scaled to body surface area (BSA) using the Haycock equation [12]. CKD-related biomarkers were determined at the central CKiD laboratory at the University of Rochester, whereas complete blood count and serum CO2 were measured locally. Serum creatinine (enzymatic), BUN and renal function panel (serum sodium, potassium, calcium and phosphorus) were analyzed on a Bayer Advia 2400 analyzer (Siemens Diagnostics, Tarrytown, NY, USA) and cystatin C was determined by nephelometry (Siemens Diagnostics). Details of the techniques used to measure the first morning urine protein/creatinine ratio (uP/C) have previously been published [13]. BP was determined at each study visit as the average of three auscultatory measurements obtained with an aneroid sphygmomanometer [14]. The CKD diagnoses were reviewed by the members of the CKiD Steering Committee and categorized as either glomerular or nonglomerular etiology. Nephrotic range proteinuria was defined as uP/C > 2.0 mg/mg. Anemia was defined as hemoglobin < 5th percentile using age- and sex-specific norms [15]. Elevated blood pressure was defined as systolic or diastolic BP > the 90th percentile for age, sex, and height [16], whereas high normal BP was defined as systolic or diastolic BP between the 50th and 90th percentile. Elevated serum phosphate was defined as > 6.5 mg/dL for children <13 years old and > 4.5 mg/dL for children > 13 years [17]. Elevated serum potassium was defined as > 5.2 mEq/L and acidosis was defined as serum CO2 < 22 mEq/L [18]. Self-reported annual income was categorized into ≤ $30,000, $30,001 to $75,000, and > $75,000. Family size was categorized as three or fewer family members versus more than three family members. The study also collected self-reported health insurance status (yes/no) and occurrence of an emergency room visit in the past year (yes/no). Past values of covariates were carried forward to fill in missing values.
Definition of outcome
Development of end-stage kidney disease was considered the initiation of renal replacement therapy (RRT; dialysis or transplant). Time to RRT was defined as the time from the baseline visit of the CKiD study to RRT, loss to follow-up, or 31 October 2015. Deaths, which were rare events in this pediatric cohort, were censored.
Statistical analysis
Cox proportional hazards models were used to evaluate the unadjusted and adjusted associations between time-varying covariate levels and time to RRT. Analyses were adjusted or weighted to control for the confounding effects of age (per year), male sex, glomerular diagnosis, GFR (per ml/min), nephrotic range proteinuria, anemia, elevated blood pressure, elevated potassium, elevated phosphate and acidosis, on the relationship between ACE-I/ARB use and time to RRT. Race was not included as a possible confounder, as race was not associated with ACE-I/ARB use in the current study. Previous work on CKD progression in the CKiD cohort was used to guide selection of potential confounders [19].
In a traditionally adjusted analysis, the time to RRT was regressed on the time-varying factors age, GFR, nephrotic range proteinuria, anemia, elevated blood pressure, elevated potassium, elevated phosphate, acidosis, and ACE-I/ARB use, all lagged by one visit relative to the outcome assessment; male sex and glomerular diagnosis status were time-fixed. Exploratory analyses were also carried out in subgroups defined by age (≤10 years versus >10 years), race (black race versus nonblack race), diagnosis (glomerular versus nonglomerular) and duration of reported ACE-I/ARB use during the study (<3 years versus ≥3 years) to assess the potential for the heterogeneity of the ACE-I/ARB effect.
In an inverse probability-of-treatment (IPT) weighted marginal structural (MSM) model, the time to RRT was regressed on time-varying ACE-I/ARB use, with stabilized IPT weights [20], used to address confounding by age, GFR, nephrotic range proteinuria, anemia, elevated blood pressure, elevated potassium, elevated phosphate, and acidosis. IPT weights were estimated from two pooled logistic models (one for visits before initiation of ACE-I/ARB and one for visits after initiation), treating each visit as an observation and including a time-dependent intercept. For visits before initiation, the logistic IPT weight models included only age, anemia, nephrotic range proteinuria, elevated blood pressure, elevated potassium, elevated phosphate, and acidosis. For visits after initiation, logistic IPT weight models included, in addition to the aforementioned factors, GFR, an indicator for ACE-I/ARB use at the previous visit, and a count of the number of past visits when on ACE-I /ARBs. IPT weight truncation at the 99th percentile was used to avoid undue influence of extreme weights [21, 22]. Inverse probability of censoring (IPC) weights were also estimated and used to control for differential loss to follow-up. IPC weight models included age, GFR, an indicator for ACE-I/ARB use at the previous visit, income level, family size, and occurrence of emergency room visits. Weights were estimated and applied using established methods [20]. No subgroup analyses were run using Cox MSM models to avoid possible weight instability.
Analyses were performed in SAS version 9.2 (SAS Institute) and in R 2.15.2 [23]. All tests were two-tailed and a p value < 0.05 was considered statistically significant.
Results
Study sample
A total of 851 participants (588 whose CKD had a nonglomerular etiology and 263 whose CKD had a glomerular etiology) contributed time and events to the analysis, which represented 96 % of the full CKiD cohort. Among those, 217 children experienced RRT, 179 children were lost to follow-up during the period of observation, 6 children died, and 449 were administratively censored because they remained RRT-free at the end of observation. Participants contributed a median follow-up time of 4.1 years (interquartile range [IQR]: 2.8, 7.8). Covariate values were missing at 26 % of visits, no variable was missing at more than 14 % of the visits, and clinical variables were missing no more than 5 % of the time.
Baseline characteristics by exposure to ACE-I/ARB
At baseline, 472 children were prevalent users of ACE-I/ARBs, with 90 % on an ACE-I. The most commonly used ACE-Is were enalapril (Vasotec) and lisinopril (Prinivil, Zestril), which accounted for 46 % of users each. ACE-I/ARB user groups differed with regard to many characteristics that are predictive of progression [19]. Users were more likely to be older, have a glomerular etiology of CKD, have a higher uP/C, be anemic, have elevated serum phosphate, have elevated serum potassium, and take more medications. They were less likely to have elevated blood pressure, compared with non-users (Table 1). Children with glomerular etiology, who comprised a disproportionately large proportion of ACE-I/ARB users at baseline (45 % of users, but 31 % of the overall cohort), were predominantly diagnosed with focal segmental glomerulosclerosis (29 %), hemolytic uremic syndrome (19 %), systemic immunological disease including SLE (14 %), chronic glomerulonephritis (8 %), familial nephritis (Alport syndrome; 7 %), IgA nephropathy (Berger’s, 6 %), or membranoproliferative glomerulonephritis type I (4 %).
Traditionally adjusted analysis of ACE-I/ARB and time to RRT
Switching occurred over time with ACE-I/ARB use. The median duration of reported ACE-I/ARB exposure under observation was three visits (approximately 3 years) among those with baseline use and two visits (approximately 2 years) among initiators who were naïve at baseline. Treating ACE-I/ARB use as time-varying to account for switching and lagging exposure by 1 year, the univariate association with time to RRT was 0.51 (95 % CI: 0.39, 0.67), suggesting a strongly protective effect of recent ACE-I/ARB such that recent users had a 49 % lower hazard of RRT compared with non-users (Table 2). Standard regression adjustment for time-varying demographic and clinical predictors of progression attenuated the effect, however, yielding an estimated hazard ratio of 0.79 (95 % CI: 0.59, 1.07), suggesting a weaker nonsignificant protective effect of recent ACE-I/ARB use on the risk of RRT (21 % lower hazard of RRT compared with non-users).
Discontinuation of ACE-I/ARB use and MSMs
Table 1 shows a comparison of ACE-I/ARB discontinuers and continuers among children who had a previous history of ACE-I/ARB use (N = 611, where 472 had baseline use and 139 initiated use under observation) at the last study visit. Discontinuers were more likely to have a lower GFR, higher uP/C ratio, be anemic, have elevated blood pressure, have elevated phosphate levels, and take more medications, but their kidney disorder was less likely to have a glomerular etiology. The use of IPT weighting to balance covariate profiles on characteristics that influence both the choice to initiate ACE-I/ARBs and to discontinue ACE-I/ARBs yielded an estimate of the effect of continuous use of ACE-I/ARB of 0.63 (95 % CI: 0.46, 0.87) versus never use in comparable groups, assuming all relevant confounders were measured and appropriately specified (Table 2). This estimate suggests that maintaining children on ACE/ARBs might reduce the hazard of RRT by 37 % compared with children never put on ACE-I /ARBs for the control of hypertension and proteinuria. As the model also included IPC weights, the final estimate should also be free of any selection bias resulting from informative dropout under the assumption that measured covariates sufficiently controlled for factors related to differential loss from the study.
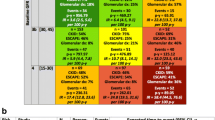
Subgroup analyses of ACE-I/ARB and time to RRT
Using traditionally adjusted analysis of ACE-I/ARB and time to RRT, we found some qualitative differences in the estimated effect of ACE-I/ARB use by subgroup. The adjusted hazard ratios for RRT assessing the effect of recent ACE-I/ARB use among subgroups were as follows: 1.24 (95 % CI: 0.48, 3.20) for children 10 years and younger in the cohort versus 0.78 (95 % CI: 0.57, 1.07) for children older than 10 years; 0.53 (95 % CI: 0.29, 0.98) for children of black race versus 0.87 (95 % CI: 0.61, 1.25) for white or another race; 1.36 (95 % CI: 0.75, 2.48) for children with glomerular diagnosis versus 0.62 (95 % CI: 0.44, 0.89) for children with nonglomerular diagnosis; 0.87 (95 % CI: 0.57, 1.35) for children reporting ACE-I/ARB use for less than 3 years versus 0.55 (95 % CI: 0.32, 0.96) for children reporting use for 3 or more years.
Discussion
In this analysis, we used two approaches to estimating the effect of ACE-I/ARB therapy on CKD progression in the CKiD observational data. From the time-varying exposure Cox model and the MSM Cox model, we estimated that the use of RAAS blockade reduces the risk of ESRD by 21 % (hazard ratio: 079) to 37 % (hazard ratio: 0.63) in a pediatric CKD cohort. These estimates are consistent with findings in adults. Drawz and Rosenberg [24] suggested that, “The magnitude of these beneficial effects of RAAS blockade is estimated to be about a 20 % risk reduction…”, which echoes results from the RENAAL and AASK trials [5, 25]. Other adult studies have reported effect sizes within the range 40–70 % for ESRD and serum creatinine doubling endpoints [2, 3, 26, 27].
Our range of estimated risk protection represents uncertainty both with regard to how best to achieve appropriate comparability between treatment groups in an observational study, but also how best to characterize exposure to ACE-I/ARBs given dynamic treatment strategies. The estimate of benefit associated with continuous ACE-I/ARB use from the MSM Cox model may not be reflective of how ACE-I/ARBs are used in clinical practice, and thus may not be achievable. However, there are possible insights from the estimate, which is similar to what one could obtain from a well-run clinical trial.
First, there appears to be benefit associated with continuing use across the full spectrum of disease severity in our study. This has important clinical implications as clinicians caring for children with CKD often observe a reduction in estimated GFR resulting from commencing ACE-I/ARB use, which may prompt them to discontinue the therapy. Although evidence suggests that this phenomenon might not result in long-term harm, analyses of RENAAL trial data indicated better long-term outcomes in those with an initial fall in GFR [28], reductions in GFR are concerning and our results suggest that clinicians choose to maintain residual kidney function by discontinuing ACE-I /ARBs. Side effects of ACE-I /ARB use, such as hyperkalemia or hypotension, were not evident among discontinuers.
Second, the analysis suggests that ACE-I/ARB use is beneficial in a general pediatric CKD population that includes both hypertensive and normotensive participants. In the CKiD cohort, approximately 70 % of patients have blood pressure less than the 90th percentile and approximately 20 % have blood pressure less than the 50th percentile. The MSM Cox estimate of benefit, which assesses the benefit of continual use in everyone in the cohort, lends support to findings from the Collaborative Study Group that the benefits of ACE-I/ARB use extend beyond blood pressure control [2].
However, our estimate must also be interpreted with caution. The dynamics of treatment decisions can make evaluations of therapy effectiveness challenging in observational data. MSM models try to get around the problem of estimating an effect of a dynamic treatment in the presence of time-varying confounders that are themselves affected by previous treatment, a problem that has been well described [29, 30], but may or may not be biasing the standard regression adjustment analysis in the current study. MSM models depend upon the accurate and complete capture of all factors that confound the treatment–outcome relationship, in addition to correct specification of the IPT weight model. Many measured and unmeasured factors likely influence clinician decisions and the incorrect or incomplete specification of the IPT model could have resulted in bias in either direction. In point of fact, we found that the clinical covariates in the weighting models were not strongly predictive of ACE-I/ARB initiation or continuation and the continuation/discontinuation groups remained unbalanced, suggesting that the MSM Cox estimate might be optimistic.
In contrast, the time-varying ACE-I/ARB use status and standard regression adjustment methods address the more relevant question of the effect of recent therapy status on the risk of RRT given the reality of dynamic treatment histories. However, adjusting for time-varying factors that are affected by previous ACE-I/ARB treatment could have attenuated the effect estimate if those factors themselves are a means of slowing progression (e.g., reductions in blood pressure achieved by previous use of ACE-I/ARBs). In that case, a 21 % reduction in RRT risk would be a conservative estimate.
Exploratory subgroup analyses suggest some differences between strata. It is possible that true differences exist; however, it is also possible that these findings are due to chance. Several factors such as black race and glomerular disease represent only 20–30 % of the sample and thus there is a danger of spurious results. The width of the confidence intervals in the younger age strata suggests that this estimate may not be robust potentially because of too few events or less ACE-I/ARB use. For assessing duration of ACE-I/ARB use, many children entering CKiD were in CKD care for years before active observation in the study, and thus the history of RAAS therapy use is unknown. Therefore, the subgroup estimates should only serve to suggest targets for further research.
There are substantial limitations to our analysis that deserve discussion. As the majority of ACE-I/ARB users were on ACE-Is, we could not assess the relative benefits of ACE-I use versus ARB use in this cohort. Further, the current analysis does not suggest a mechanism through which ACE-I/ARBs act to reduce risk, although both elevated blood pressure and proteinuria are established risk factors for progression in children [7, 31–33]. The assessment of ACE-I/ARB use is made at each annual visit and therefore, switching in between visits cannot be accounted for in the current analysis. However, after adjusting for GFR and indicators of disease severity, it is unlikely that between visit changes in ACE-I/ARB use would be differential by outcome status. Therefore, switching on and off ACE-I/ARBs in between visits would most likely add random measurement error to the assessment of ACE-I/ARB exposure and attenuate estimates. We could not adjust for clinical site differences in ACE-I/ARB use or outcome risk as most sites contribute relatively few children; thus, confounding by clinical site could have introduced bias into the analysis. We chose to focus on the outcome of time to RRT rather than a composite outcome that incorporated GFR decline to simplify causal interpretation. Future investigation into the effect of ACE-I/ARB use focusing on GFR decline could be done using MSMs for repeated measures data, which have also been developed and described [34]. Finally, our estimates may be biased to the extent that important predictors of either ACE-I/ARB use or time to RRT were not captured or included in the MSM Cox models or standard regression adjusted Cox models, respectively. Although predictors of the time to RRT have been well characterized in the CKiD study [19], factors affecting clinical decisions regarding ACE-I/ARB use are less well understood and therefore the estimate from the MSM Cox model is most at risk for residual confounding bias.
Our results in a pediatric setting, where to our knowledge no direct clinical trial data exist, provide evidence that the benefit of ACE-I/ARB use noted in adult CKD patients extends to children with moderate to severe CKD, providing a reduction in the risk of RRT of approximately 21–37 %.
References
US Renal Data System: USRDS (2013) Annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda
Lewis EJ, Hunsicker LG, Bain RP, Rohde RD (1993) The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The collaborative study group. N Engl J Med 329:1456–1462
Ruggenenti P, Perna A, Gherardi G, Garini G, Zoccali C, Salvadori M, Scolari F, Schena FP, Remuzzi G (1999) Renoprotective properties of ACE-inhibition in non-diabetic nephropathies with non-nephrotic proteinuria. Lancet 354:359–364
Ruggenenti P, Perna A, Gherardi G, Benini R, Remuzzi G (2000) Chronic proteinuric nephropathies: outcomes and response to treatment in a prospective cohort of 352 patients with different patterns of renal injury. Am J Kidney Dis 35:1155–1165
Wright JT Jr, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, Cheek D, Douglas-Baltimore JG, Gassman J, Glassock R, Hebert L, Jamerson K, Lewis J, Phillips RA, Toto RD, Middleton JP, Rostand SG (2002) Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 288:2421–2431
Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group (2012) KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl 2:337–414
Wuhl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, Zurowska A, Testa S, Jankauskiene A, Emre S, Caldas-Afonso A, Anarat A, Niaudet P, Mir S, Bakkaloglu A, Enke B, Montini G, Wingen AM, Sallay P, Jeck N, Berg U, Caliskan S, Wygoda S, Hohbach-Hohenfellner K, Dusek J, Urasinski T, Arbeiter K, Neuhaus T, Gellermann J, Drozdz D, Fischbach M, Moller K, Wigger M, Peruzzi L, Mehls O, Schaefer F (2009) Strict blood-pressure control and progression of renal failure in children. N Engl J Med 361:1639–1650
Furth SL, Abraham AG, Jerry-Fluker J, Schwartz GJ, Benfield M, Kaskel F, Wong C, Mak RH, Moxey-Mims M, Warady BA (2011) Metabolic abnormalities, cardiovascular disease risk factors, and GFR decline in children with chronic kidney disease. Clin J Am Soc Nephrol 6:2132–2140
Furth SL, Cole SR, Moxey-Mims M, Kaskel F, Mak R, Schwartz G, Wong C, Munoz A, Warady BA (2006) Design and methods of the chronic kidney disease in children (CKiD) prospective cohort study. Clin J Am Soc Nephrol 1:1006–1015
Schwartz GJ, Abraham AG, Furth SL, Warady BA, Munoz A (2010) Optimizing iohexol plasma disappearance curves to measure the glomerular filtration rate in children with chronic kidney disease. Kidney Int 77:65–71
Schwartz GJ, Schneider MF, Maier PS, Moxey-Mims M, Dharnidharka VR, Warady BA, Furth SL, Muñoz A (2012) Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int 82:445–453
Haycock GB, Schwartz GJ, Wisotsky DH (1978) Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr 93:62–66
Wong CS, Pierce CB, Cole SR, Warady BA, Mak RH, Benador NM, Kaskel F, Furth SL, Schwartz GJ (2009) Association of proteinuria with race, cause of chronic kidney disease, and glomerular filtration rate in the chronic kidney disease in children study. Clin J Am Soc Nephrol 4:812–819
Flynn JT, Mitsnefes M, Pierce C, Cole SR, Parekh RS, Furth SL, Warady BA (2008) Blood pressure in children with chronic kidney disease: a report from the chronic kidney disease in children study. Hypertension 52:631–637
Hollowell JG, van Assendelft OW, Gunter EW, Lewis BG, Najjar M, Pfeiffer C (2004) Hematological and iron-related analytes—reference data for persons aged 1 year and over: United States, 1988–94. Vital Health Stat 11:1–156
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
KDOQI (2005) Clinical practice guidelines for bone metabolism and disease in children with chronic kidney disease. Am J Kidney Dis 46:S1–S122
KDOQI (2009) Clinical practice guideline for nutrition in children with CKD: 2008 update. Executive summary. Am J Kidney Dis 53:S11–S104
Warady BA, Abraham AG, Schwartz GJ, Wong CS, Munoz A, Betoko A, Mitsnefes M, Kaskel F, Greenbaum LA, Mak RH, Flynn J, Moxey-Mims MM, Furth S (2015) Predictors of rapid progression of glomerular and nonglomerular kidney disease in children and adolescents: the chronic kidney disease in children (CKiD) cohort. Am J Kidney Dis 65:878–888
Hernan MA, Brumback B, Robins JM (2000) Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology 11:561–570
Cole SR, Hernan MA (2008) Constructing inverse probability weights for marginal structural models. Am J Epidemiol 168:656–664
Xiao Y, Abrahamowicz M, Moodie EE (2010) Accuracy of conventional and marginal structural Cox model estimators: a simulation study. Int J Biostat 6:Article 13
R Core Team (2012) A language and environment for statistical computing [Internet]. In: R Foundation for Statistical Computing. Available from: http://www.R-project.org/
Drawz PE, Rosenberg ME (2013) Slowing progression of chronic kidney disease. Kidney Int Suppl (2011) 3:372–376
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S (2001) Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 345:861–886
Tokunaga M, Kabashima N, Serino R, Shibata T, Matsumoto M, Miyamoto T, Miyazaki M, Furuno Y, Nakamata J, Fujimoto Y, Takeuchi M, Abe H, Okazaki M, Otsuji Y, Tamura M (2010) Renoprotective effects of telmisartan in patients with advanced chronic kidney disease. Clin Nephrol 73:139–146
Hou FF, Zhang X, Zhang GH, Xie D, Chen PY, Zhang WR, Jiang JP, Liang M, Wang GB, Liu ZR, Geng RW (2006) Efficacy and safety of benazepril for advanced chronic renal insufficiency. N Engl J Med 354:131–140
Holtkamp FA, de Zeeuw D, Thomas MC, Cooper ME, de Graeff PA, Hillege HJ, Parving HH, Brenner BM, Shahinfar S, Lambers Heerspink HJ (2011) An acute fall in estimated glomerular filtration rate during treatment with losartan predicts a slower decrease in long-term renal function. Kidney Int 80:282–287
Robins JM, Hernán MA, Brumback B (2000) Marginal structural models and causal inference in epidemiology. Epidemiology 11:550–560
Cole SR, Platt RW, Schisterman EF, Chu H, Westreich D, Richardson D, Poole C (2010) Illustrating bias due to conditioning on a collider. Int J Epidemiol 39:417–420
Ardissino G, Testa S, Daccò V, Viganò S, Taioli E, Claris-Appiani A, Procaccio M, Avolio L, Ciofani A, Dello Strologo L, Montini G, Ital Kid Project (2004) Proteinuria as a predictor of disease progression in children with hypodysplastic nephropathy. Data from the Ital Kid Project. Pediatr Nephrol 19:172–177
Wingen AM, Fabian-Bach C, Schaefer F, Mehls O (1997) Randomised multicentre study of a low-protein diet on the progression of chronic renal failure in children. European study group of nutritional treatment of chronic renal failure in childhood. Lancet 349:1117–1123
Litwin M (2004) Risk factors for renal failure in children with non-glomerular nephropathies. Pediatr Nephrol 19:178–186
Hernán MA, Brumback BA, Robins JM (2002) Estimating the causal effect of zidovudine on CD4 count with a marginal structural model for repeated measures. Stat Med 21:1689–1709
Acknowledgements
The authors acknowledge the contributions of all investigators and coordinators in the CKiD Study (www.statepi.jhsph.edu/ckid), in addition to all participating patients and their families. Data in this manuscript were collected by the CKiD prospective cohort study with clinical coordinating centers (principal investigators) at the Children’s Mercy Hospital and the University of Missouri–Kansas City (Bradley A. Warady, MD) and the Children’s Hospital of Philadelphia (Susan Furth, MD, PhD), the Central Biochemistry Laboratory at the University of Rochester Medical Center (George J. Schwartz, MD), and the data coordinating center at the Johns Hopkins Bloomberg School of Public Health (Alvaro Muñoz, PhD). The CKiD Study is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, with additional funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Heart, Lung and Blood Institute (grants U01-DK-66143, U01-DK-66174, U01DK-082194, and U01-DK-66116).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
The study design and conduct was approved by the internal review board of each participating center and by an external advisory committee appointed by the National Institutes of Health. Written informed consent/assent was obtained from all participants/families according to local requirements.
Competing financial interests
The authors declare that they have no other relevant financial interests.
Rights and permissions
About this article
Cite this article
Abraham, A.G., Betoko, A., Fadrowski, J.J. et al. Renin–angiotensin II–aldosterone system blockers and time to renal replacement therapy in children with CKD. Pediatr Nephrol 32, 643–649 (2017). https://doi.org/10.1007/s00467-016-3512-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3512-4