Abstract
Little is known about the role of proteinuria in the progression of childhood renal diseases. We analyzed the decline in creatinine clearance (C Cr) and kidney survival in 225 children (185 males) with chronic renal failure (CRF) due to isolated hypodysplasia or hypodysplasia associated with urological abnormalities. The data were based on the information available in the Italian Pediatric Registry of CRF (ItalKid Project), which includes patients from all of Italy aged <20 years with C Cr levels of <75 ml/min per 1.73 m2. Patients aged <2 years and those with C Cr levels of <20 ml/min per 1.73 m2 or a follow-up of <1 year were excluded from the analysis, as were those receiving angiotensin-converting enzyme inhibitors. At baseline, the patients had a mean age of 7.8±4.2 years, a mean C Cr of 50±16.3 ml/min per 1.73 m2, a median urinary protein/urinary creatinine (uPr/uCr) ratio of 0.38 (range 0.02–7.21), and a mean duration of follow-up of 3.5±1.1 years. The patients were divided into three groups on the basis of their baseline proteinuria levels: group A normal (uPr/uCr <0.2) n=83; group B low (uPr/uCr 0.2–0.9) n=71; and group C mild (uPr/uCr >0.9) n=71. Patients in groups A and B showed a significantly slower decline in C Cr than those in group C (slope +0.16±3.64 and −0.54±3.67 vs. −3.61±5.47, P<0.0001) and a higher rate of kidney survival after 5 years (96.7% and 94.1% vs. 44.9%, P<0.01). By multivariate analysis, the baseline uPr/uCr ratio (P<0.01) and age (P<0.0001) correlated with a faster decline in C Cr irrespective of baseline C Cr. There was no correlation with mean arterial blood pressure. We conclude that proteinuria is an independent predictor of progression to end-stage renal failure also in children whose renal impairment is due to congenital hypodysplasia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal diseases in both children and adults progress to end-stage renal failure (ESRF) despite the removal of the initial cause of renal injury [1, 2]. Their progressive nature and the loss of filtration function have been related to focal nephron loss with subsequent hypertrophy, and hyperfiltration in the remaining glomeruli. These compensatory adaptations are almost invariably associated with the development of glomerulosclerosis [1, 3, 4] and glomerular capillary hypertension, leading to an increase in the transglomerular filtration of plasma proteins [5]. A number of animal and human studies have shown that the proteins filtered by the glomerulus are responsible for further tubulo-interstitial injury that leads to parenchymal damage, renal scarring and, ultimately, functional impairment [6, 7, 8].
In adult patients with diabetic or non-diabetic nephropathies, the rate of urinary protein excretion correlates with the rate of decline in the glomerular filtration rate (GFR) and progression to ESRF [9, 10, 11, 12, 13, 14, 15]. On the basis of these findings, it has recently been proposed that antiproteinuric treatment with angiotensin-converting enzyme inhibitors (ACEi) may reduce the progression of renal disease [16].
The primary causes of chronic renal failure (CRF) in children are very different from those in adults, and there is little information concerning the role of proteinuria in declining renal function [17].
Reproducing the methodology used by Ruggenenti et al. [18] in a previous study of adults, the aim of this study was to investigate the role of urinary protein excretion in predicting the decline in renal function in a large cohort of children with CRF due to hypodysplasia with or without urinary malformations.
Patients and methods
The study was based on the data available in the Italian Pediatric Registry of CRF (ItalKid), which includes all of the patients in Italy diagnosed as having pre-dialysis CRF {creatinine clearance (C Cr) of <75 ml/min per 1.73 m2 according to Schwartz [19]} before the age of 20 years.
Registration was started in 1990, when all of the Italian centers potentially involved in caring for children and adolescents with renal diseases (pediatric nephrology, pediatrics, pediatric urology, pediatric surgery, and adult nephrology units) were invited to report index cases on an annual basis. The general methodology of the ItalKid Project (its organizational structure, reporting procedures, and data quality control) is described in detail elsewhere [20]. As of 1 January 2001, 1,197 children attending 112 centers had been registered.
For the purposes of this study, we selected 732 patients with CRF due to hypodysplasia with or without urological abnormalities. The exclusion criteria were: (1) baseline C Cr of ≤20 ml/min per 1.73 m2 (n=80); (2) treatment with ACEi (n=131); (3) a follow-up of ≤1 year (n=88); and (4) unreported baseline urinary protein excretion (n=161). All of the observations in patients aged younger than 2 years were also excluded because of the increased GFR commonly found in very young patients with congenital renal diseases due to compensatory hypertrophy (particularly hypodysplasia), and the difficulty in identifying the most appropriate “k” value to apply to the Schwartz formula during the first 2 years of life. The final analysis was therefore based on 225 subjects (185 males). The primary renal diseases responsible for CRF were hypodysplasia with associated urological abnormalities (n=171) [vesicouretheral reflux (n=104), posterior urethral valves (n=45), other urinary abnormalities (n=22)], and isolated hypodysplasia (n=54).
The considered clinical variables were age, gender, and systolic, diastolic, and mean blood pressure. Blood pressure was analyzed as an age- and gender-specific standard deviation score (SDS) using the reference values of the Task Force on Blood Pressure Control in Children—1987 [21]. The biochemical parameters were C Cr and the urinary protein/urinary creatinine ratio [uPr (mg/dl)/uCr (mg/dl)]. The primary outcome measure was the rate of progression of CRF, calculated as the C Cr slope throughout the follow-up period.
The patients were divided into three groups on the basis of their baseline proteinuria levels: group A (normal urinary protein excretion uPr/uCr <0.2, upper normal limit [22]), group B (low proteinuria uPr/uCr 0.2–0.9), and group C (mild proteinuria uPr/uCr >0.9). A uPr/uCr of 0.9 (the cut-off point between groups B and C) was identified as the median abnormal uPr/uCr. The start of renal replacement therapy was used as the end-point for the survival curves.
Data quality control
An annual follow-up form requesting updated clinical and biochemical data was issued by the National Coordinating Center for each registered patient, identified by name, date of birth, gender, and diagnosis. This allowed the reporting center to check for any previous incorrect reporting, thus increasing the accuracy of the stored data and enhancing the likelihood that the follow-up data would be reported. A fixed series of internal validity checks was made at the end of each year, and all inconsistencies were discussed with the reporting center.
A quality control survey involving a sample of 20% of the participating laboratories (covering more than 80% of the registered patients) was carried out in order to assure the reliability of the definition of CRF and the decline in renal function based on locally determined serum creatinine (sCr) levels. Three human serum samples taken from pools of sera in the normal, high, and very high sCr range were sent to the selected laboratories. At sCr levels of 76, 172, and 304 μmol/l, the observed coefficients of variation were respectively 13.0%, 7.6%, and 6.0%.
Statistical analysis
Unless otherwise specified, the data are expressed as mean values±SD. The uPr/uCr ratio is expressed as median values and ranges because it is not normally distributed. The slope of C Cr over time was calculated for each patient using all of the available C Cr determinations obtained during the follow-up. The between-group differences at baseline were assessed by means of ANOVA. The contingency table was analyzed using the χ 2 test. The survival analysis was based on the Kaplan-Meyer method, and the between-group differences in survival rates in the life-table analysis were evaluated using log-rank statistics. Survival was adjusted for baseline proteinuria and C Cr levels. The univariate correlations between the continuous baseline variables and the decline in C Cr were analyzed using Pearson’s correlation coefficient (r). The multivariate analysis was performed using the General Linear Model with the decline in C Cr (slope) as the dependent variable, and age, gender, the uPr/uCr ratio, systolic, diastolic, and mean arterial blood pressure, and baseline C Cr as independent variables. A P value of <0.01 was considered statistically significant.
The patients were defined as having progressive or non-progressive disease depending on whether the decrease in C Cr was more or less than −3 ml/min per 1.73 m2 per year, as previously defined by Wingen et al. [17].
Results
The mean uPr/uCr ratio in the population as a whole was 0.88±1.23; only 5.3% of the patients had severe proteinuria (uPr/uCr >3.5). Table 1 shows the baseline clinical and laboratory parameters in the population as a whole, and in the three groups divided on the basis of their uPr/uCr ratio. The distributions of gender, age, blood pressure (systolic, diastolic, and mean SDS) and the prevalence of antihypertensive treatment were comparable in the three groups. Baseline C Cr was significantly higher in the patients with normal (group A) and low proteinuria levels (group B) than in those with mild proteinuria (group C).
The mean follow-up was 3.5±1.1 years, with no significant difference between the groups. Follow-up blood pressure was similar in the three groups: the mean systolic and diastolic SDS were 0.24±0.76 and 0.27±0.81 in group A, 0.21±0.88 and 0.29±0.91 in group B, and 0.23±0.86 and 0.43±0.85 in group C.
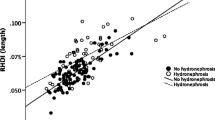
The mean rate of C Cr decline (C Cr slope over time) in the population as a whole was −1.25 ± 4.58. As shown in Fig. 1, the patients with normal and low urinary protein excretion levels (groups A and B) showed a non-significant loss of renal function, with a mean slope of respectively +0.16±3.64 and −0.54±3.67, and a percentage of progressive patients of 15.7% and 19.7% (NS). The rate of decline in renal function was significantly faster in the subjects with mild proteinuria (group C), mean slope −3.61±5.4 (P<0.0001 vs. groups A and B). As many as 46.5% of the patients in group C progressed during the follow-up period (P<0.0001 vs. groups A and B, Table 2). The primary disease (vesicoureteral reflux, posterior urethral valves, other urinary tract abnormalities, isolated hypodysplasia) did not account for any statistically significant difference in the uPr/uCr ratio (median values 0.39, 0.23, 0.59, and 0.56) or C Cr slope (mean values −0.6±4.0, −1.7±4.7, −1.5±5.8, and −2.0±5.0).
Analysis of the correlations between the C Cr slope and baseline variables in the population as a whole showed that age, C Cr, and the uPr/uCr ratio were all significantly associated with a faster decline (P<0.0001). However, the only baseline parameters significantly predictive of a faster decline in C Cr by multivariate analysis were age (P<0.0001) and uPr/uCr (P<0.01) (Table 3).
When the progression of renal damage was analyzed in terms of kidney survival (Fig. 2), only the patients with mild proteinuria (group C) showed a significantly higher risk of ESRF (P<0.01) after 5 years of follow-up.
Discussion
It has been increasingly recognized over the last decade that urinary protein excretion is a reliable predictor and possible cause of a poor outcome (risk of progression to ESRF) in both diabetic and non-diabetic adult patients with proteinuric renal diseases, but there is little information concerning the role of urinary protein excretion in renal diseases peculiar to children.
The primary causes of CRF during development are very different from those in adulthood. More than 60% of the cases of CRF acquired during the first 20 years of life are due to congenital hypodysplasia, with or without urinary tract abnormalities. These patients do not have overt proteinuria, and the role of urinary protein excretion in the progression of renal damage has not been extensively investigated. The results of our study provide important clues concerning the natural course of chronic, primarily non-proteinuric kidney diseases in children.
Our main finding is that proteinuria is a strong predictor of progression in children with CRF due to hypodysplasia. As the estimate of GFR by means of C Cr is insufficiently accurate, progression was studied by means of three different indicators: (1) the C Cr slope over time, (2) the percentage of progressive patients (slope <−3), and (3) kidney survival.
Proteinuria was measured in terms of the uPr/uCr, which has been shown to be as reliable as 24-h urinary protein excretion in adults [22, 23]. Furthermore, in our study, 24-h urine collection would have two possible sources of inaccuracy: (1) the difficulty of obtaining precise urine collections in children and (2) the incompleteness of urine output in patients with associated vesicoureteral reflux (>40% of our study population).
The decline in C Cr was faster in the patients with mild urinary protein excretion at the beginning of the observation period than in those with a normal or low uPr/uCr ratio (respectively 7 and 20 times faster). Furthermore, after 5 years of follow-up, kidney survival in the patients with normal and low proteinuria was more than 50% higher than in those with mild proteinuria.
It is noteworthy that, even when abnormal, the proteinuria in our population was never severe. The median uPr/uCr ratio in the patients defined as having mild proteinuria (group C) was 1.79, which is far from nephrotic levels (>3.5) [22].
It is also interesting to note that the risk of progression did not increase linearly with the uPr/uCr ratio. Although the patients in group B had abnormal proteinuria, their progression patterns were similar to those of patients in group A (normal proteinuria) in terms of the mean C Cr slope (−0.54±3.67 vs. 0.16±3.64), the proportion of clearly progressive patients (19.7% vs. 15.7%), and 5-year kidney survival (94.1% vs. 96.7%).
Baseline proteinuria was a strong predictor of progressive renal disease, but our data are insufficient to establish a cause-effect relationship between proteinuria and progression. However, previous experimental [7, 8] and clinical [24] observations support the existence of such a relationship. Increased glomerular filtration induces the tubular reabsorption of proteins and their accumulation in the cytoplasm of proximal tubular cells. The toxic effect of this protein overload breaks the basement membrane and releases the cell contents into the interstitium, thus triggering an inflammatory reaction and consequent tubulointerstitial and glomerular damage.
A number of studies of adults [25] and children [17] have clearly demonstrated that poor blood pressure control is another important risk factor for the progression of kidney diseases, and it may seem surprising that we did not find such a relationship. However, it is well known [26] that patients with CRF due to hypodysplasia who develop hypertension do so at very low GFR levels and during the late phase of the disease. Our analysis excluded patients with C Cr levels of <20 ml/min per 1.73 m2, and therefore only 3.6% had a mean arterial blood pressure of >97th percentile. Moreover, it should be noted that in the ItalKid database blood pressure is recorded as a single office measurement that may not accurately reflect true blood pressure. It is becoming increasingly clear that 24-h blood pressure recording may be necessary to describe the individual blood pressure patterns. This better predicts the risk of organ damage, including renal damage and its progression to ESRF [27, 28, 29, 30, 31].
The population of the present study can be considered fairly homogeneous because, when present, the uropathies associated with hypodysplasia (vesicoureteral reflux, posterior urethral valves, etc.) did not account for any differences in either the uPr/uCr ratio or progression.
It is important to emphasize that multivariate analysis excluded any relationship between baseline C Cr and progression, although the patients with a mild uPr/uCr ratio (group C) had a significantly lower baseline C Cr level (Table 3).
The only baseline parameter other than proteinuria that significantly correlated with a faster progression was age. A previous analysis of ItalKid Project data [32] indicated a unique pattern of CRF progression in children, characterized by a faster decline in renal function during puberty and early post puberty.
In conclusion, our results show that irrespective of hypertension the uPr/uCr ratio can predict the risk of progression not only in glomerular diseases, but also in a model of primarily non-proteinuric chronic renal disease, such as renal hypodysplasia (which is by far the leading cause of CRF in children). This may be helpful in establishing the so far unpredictable long-term prognosis of these patients and identifying those who may benefit from antiproteinuric treatment with ACEi. The results indirectly support the strategy of treating proteinuria regardless of the underlying primary renal disease and at any stage of CRF.
References
Brenner BM, Meyer TW, Hostetter TH (1982) Dietary protein intake and the progressive nature of kidney disease: the role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis. N Engl J Med 307:652–659
Brown DM, Andres GA, Hostetter TH, Mauer SM, Price R, Venkatachalam MA (1981) Hyperfiltration in remnant nephrons: a potentially adverse response to renal ablation. Am J Physiol 241:F85–F93
Yamamoto T, Noble NA, Miller DE, Border WA (1994) Sustained expression of TGF-beta 1 underlies development of progressive kidney fibrosis. Kidney Int 45:916–927
Ketteler M, Noble NA, Border WA (1995) Transforming growth factor-beta and angiotensin II: the missing link from glomerular hyperfiltration to glomerulosclerosis? Annu Rev Physiol 57:279–295
Anderson S, Meyer TW, Rennke HG, Brenner BM (1985) Control of glomerular hypertension limits glomerular injury in rats with reduced renal mass. J Clin Invest 76:612–619
Remuzzi G (1995) Abnormal protein traffic through the glomerular barrier induces proximal tubular cell dysfunction and causes renal injury. Curr Opin Nephrol Hypertens 4:339–342
Remuzzi G, Bertani T (1990) Is glomerulosclerosis a consequence of altered glomerular permeability to macromolecules? Kidney Int 38:384–394
Eddy AA (1989) Interstitial nephritis induced by protein-overload proteinuria. Am J Pathol 135:719–733
D’Amico G, Gentile MG, Fellin G, Manna G, Cofano F (1994) Effect of dietary protein restriction on the progression of renal failure: a prospective randomized study. Nephrol Dial Transplant 9:1590–1594
Klahr S, Levey AS, Beck GJ, Caggiula AW, Hunsicker L, Kusek JW, Striker G (1994) The effects of dietary protein restriction and blood pressure control on the progression of chronic renal disease. Modification of Diet in Renal Disease Study Group. N Engl J Med 330:877–884
Locatelli F, Alberti D, Graziani G, Buccianti G, Redaelli B, Giangrande A, Marcelli D, Francucci BM (1992) Factors affecting chronic renal failure progression: results from a multicentre trial. Miner Electrolyte Metab 18:295–302
Perna A, Remuzzi G (1996) Abnormal permeability to proteins and glomerular lesions: a meta-analysis of experimental and human studies Am J Kidney Dis 27:34–41
Rossing P, Hommel E, Smidt UM, Parving HH (1993) Impact of arterial blood pressure and albuminuria on the progression of diabetic nephropathy in IDDM patients. Diabetes 42:715–719
Breyer JA, Bain RP, Evans JK, Nahman NS Jr, Lewis EJ, Cooper M, McGill J, Berl T (1996) The Collaborative Study Group: predictors of the progression of renal insufficiency in patients with insulin-dependent diabetes and overt diabetic nephropathy. Kidney Int 50:1651–1658
Peterson JC, Adler S, Burkart JM, Greene T, Hebert LA, Hunsicker LG, King AJ, Klahr S, Massry SG, Seifter JL for the modification of diet in renal disease (MDRD) Study Group (1995) Blood pressure control, proteinuria, and the progression of renal disease. Ann Intern Med 123:754–762
The GISEN Group (1997) Randomized placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. Lancet 349:1857–1863
Wingen AM, Fabian-Bach C, Schaefer F, Mehls O, for the European Study Group for Nutritional Treatment of Chronic Renal Failure in Childhood (1997) Randomised multicentre study of a low-protein diet on the progression of chronic renal failure in children. Lancet 349:1117–1123
Ruggenenti P, Perna A, Mosconi L, Matalone M, Pisoni R, Gaspari F, Remuzzi G on behalf of the “Gruppo Italiano di Studi Epidemiologici in nefrologia” (GISEN) (1997) Proteinuria predicts end-stage renal failure in non-diabetic chronic nephropathies. Kidney Int 52:S54–S57
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 34:571–590
Ardissino G, Daccò V, Testa S, Bonaudo R, Claris-Appiani A, Taioli E, Marra G, Edefonti A, Sereni F (2003) Epidemiology of chronic renal failure in children: data from the ItalKid Project. Pediatrics 111:382–387
Task Force on Blood Pressure Control in Children (1987) Report of the Second Task Force on Blood Pressure Control in Children. Pediatrics 79:1–25
Ginsberg JM, Chang BS, Matarese RA, Garella S (1983) Use of single voided urine samples to estimate quantitative proteinuria. N Engl J Med 309:1543–1546
Ruggenenti P, Gaspari F, Perna A, Remuzzi G (1998) Cross-sectional longitudinal study of spot morning urine protein:creatinine ratio, 24-hour urine protein excretion rate, glomerular filtration rate, and end stage renal failure in chronic renal disease in patients without diabetes. BMJ 316:504–509
Wehrmann M, Bohle A, Bogenschutz O, Eissele R, Freislederer A, Ohlschlegel C, Schumm G, Batz C, Gartner HV (1989) Long-term prognosis of chronic idiopathic membranous glomerulonephritis: an analysis of 334 cases with particular regard to tubulo-interstitial changes. Clin Nephrol 31:67–76
Klag MJ, Whelton PK, Randall BL, Neaton JD, Brancati FL, Ford CE, Shulman NB, Stamler J (1996) Blood pressure and end-stage renal disease in men. N Engl J Med 334:13–18
Ingelfinger JR (1992) Hypertension. In: Edelmann CM (ed) Pediatric kidney disease. Little Brown, Boston, pp 1889–1908
Marolf AP, Hany S, Battig B, Vetter W (1987) Comparison of casual, ambulatory and self-determined blood pressure measurements. Nephron 47:S142–S145
Staessen JA, Thijs L, Fagard R, O′Brien ET, Clement D, Leeuw PW de, Mancia G, Nachev C, Palatini P, Parati G, Tuomilehto J, Webster J (1999) Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA 282:539–546
Sokolow M, Werdegar D, Kain HK, Hinman AT (1966) Relationship between level of blood pressure measured casually and by portable recorders and severity of complications in essential hypertension. Circulation 34:279–298
Pessina AC, Palatini P, Sperti G, Cordone L, Libardoni M, Mos L, Mormino P, Di Marco A, Dal Palu C (1985) Evaluation of hypertension and related target organ damage by average day-time blood pressure. Clin Exp Hypertens A7:267–278
Opshal JA, Abraham PA, Halstenson CE, Keane WF (1988) Correlation of office and ambulatory blood pressure measurements with urinary albumin and N-acetyl-β-d-glucosaminidase excretions in essential hypertension. Am J Hypertens 1:117S–120S
Dacco V, Testa S, Claris-Appiani A, Ardissino G on behalf of the ItalKid (1998) Natural history of renal function in childhood chronic renal insufficiency (abstract). J Am Soc Nephrol 9:145A
Acknowledgements
The ItalKid project is supported by a research grant from the “Associazione per il Bambino Nefropatico”. We would like to thank the following for their valuable cooperation: Ms. S. Loi (Secretary of the ItalKid Project) for data management, Dr. C.A. Ferrero (Istituto Scientifico H.S. Raffaele, Laboratorio Standardizzazione) for the laboratory quality control program, Mr. P. Marchetto for computer assistance, and Mr. K. Smart (Link Srl) for his linguistic help in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was written on behalf of all the members of the ItalKid Project whose contribution has been essential. Members of the ItalKid Project:
G. Aceto (Bari), G. Airoldi (Borgomanero), G. Amici (Ancona), A. Ammenti (Parma), B. Andretta (Padova), G. Ardissino (Milano), F. Ardito (Bologna), B. Assael (Verona), L. Avolio (Pavia), S. Bassi (Montichiari), F. Battaglino (Vicenza), R. Bellantuono (Bari), A. Bettinelli (Merate), C. Bigi (Lecco), S. Binda (Varese), C. Bini (Como), D. Bissi (Gallarate), R. Boero (Torino), R. Bonaudo (Torino), A. Bordugo (Pordenone), M. Borzani (Milano), M. Bosio (Milano), A. Bottelli (Varese), G. Bovio (Pavia), A. Bracone (Bra), G. Capasso (Napoli), M. Capizzi (Milano), D. Caringella (Bari), I. Carnera (Siracusa), M.R. Caruso (Bergamo), D. Cattarelli (Brescia), V. Cecchetti (Milano), M. Cecconi (Ancona), V. Cecinati (Bari), A. Ciofani (Pescara), A. Claris-Appiani (Milano), R. Coppo (Torino), F. Corona (Milano), A. Corsini (Bentivoglio), R. Costanzo (Ragusa), P. Cussino (Savigliano), M. D’Agostino (Bergamo), V. Daccò (Milano), G. Daidone (Siracusa), R. Dall’Amico (Thiene), L. Dardanelli (Cuneo), R. De Castro (Bologna), V. De Cristofaro (Sondrio), M. De Gennaro (Roma), S. De Pascale (Bergamo), N. De Santo (Napoli), D. Delfino (R. Calabria), C.A. Dell’Agnola (Milano), L. Dello Strologo (Roma), L. Dertenois (Genova), A. Dessanti (Sassari), A. Di Benedetto (Catania), A. Di Leone (Cosenza), F. Di Lorenzo (Bologna), P. Di Turi (Bologna), A. Edefonti (Milano), W. Erckert (Silandro), A. Fabris (Verona), V. Fanos (Verona), C. Fede (Messina), A. Fella (Napoli), R. Ferraro (Scorrano), M.T. Ferrazzano (Anzio), R. Ferré (Breno), A. Ferretti (Napoli), B. Fogazzi (Brescia), P. Formentin (Cittadella), C. Fortini (Ferrara), E. Fossali (Milano), G. Fossati Bellani (Milano), M. Gaido (Torino), R. Galato (Milano), G. Gargano (Modena), V. Georgacopulo (Ferrara), L. Ghio (Milano), R. Giachino (Ivrea), M. Giani (Milano), S. Gianni (Siracusa), B. Gianoglio (Torino), M. Girodano (Bari), V. Goj (Milano), F. Grancini (Milano), G. Grott (Chieri), S. Guez (Milano), R. Gusmano (Genova), A. Iovino (Napoli), C. Isimbaldi (Lecco), A. La Manna (Napoli), G. Lama (Napoli), R. Landoni (Cinisello B.), S. Li Volti (Catania), A. Liardo (Caltagirone), V. Lotti (Cesena), R. Lubrano (Roma), I. Luongo (Napoli), E. Mancini (Bologna), N. Manganaro (Messina), M. Marangella (Torino), C. Marchesoni (Trento), K. Marenzi (Segrate), S. Maringhini (Palermo), G. Marra (Milano), E. Marras (Torino), V. Mei (Bologna), F. Menni (Milano), N. Miglietti (Brescia), R. Mignani (Rimini), P. Minelli (Bologna), R. Moioli (Milano), P. Molinari (Bologna), G. Montini (Padova), M. Montis (Cagliari), G. Mosiello (Roma), L. Murer (Padova), G. Nebbia (Milano), M. Neunhauserer (Brunico), P. Nitsch (Parma), M. Noto (Palermo), C. Oppezzo (Milano), F. Paolillo (Lodi), T. Papalia (Cosenza), R. Parini (Milano), L. Parola (Magenta), F. Passione (Foggia), L. Pavanello (CastelfrancoV.), C. Pecoraro (Napoli), M. Pedron (Bolzano), I. Pela (Firenze), A. Pellegatta (Busto Arsizio), P. Pelliccia (Chieti), M. Pennesi (Trieste), C. Pennetta (Manduria), R. Penza (Bari), L. Peratoner (Pordenone), F. Perfumo (Genova), G. Perino (Torino), C. Pesce (Vicenza), L. Pisanello (Padova), M. Pitter (Mirano), L. Pontesilli (Roma), M. Porcellini (Torino), A. Pota (Napoli), R. Prandini (Bologna), F. Puteo (Bari), I. Ratsch (Ancona), E. Ravaioli (Rimini), G. Remuzzi (Bergamo), G. Riccipetitoni (Cosenza), G. Ripanti (Pesaro), G. Rizzoni (Roma), N. Roberto (Milano), A. Rosini (Ancona), M. Rossi Doria (Bologna), S. Rota (Bergamo), M. Ruzza (Milano), D. Scorrano (Belluno), A. Selicorni (Milano), G. Selvaggio (Milano), F. Sereni (Milano), O. Sernia (Savigliano), C. Setzu (Cagliari), C. Sforzini (Milano), L. Stallone (S. Giovanni Rotondo), M. Tagliaferri (Treviglio), L. Tampieri (Lugo), A. Testagrossa (Messina), A. Turrisi (Trapani), G. Vallini (Cinisello Balsamo), E. Verrina (Genova), S. Viola (Pavia), G. Visconti (Palermo), A. Voghenzi (Ferrara), G. Zacchello (Padova)
Rights and permissions
About this article
Cite this article
Ardissino, G., Testa, S., Daccò, V. et al. Proteinuria as a predictor of disease progression in children with hypodysplastic nephropathy. Pediatr Nephrol 19, 172–177 (2004). https://doi.org/10.1007/s00467-003-1268-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-003-1268-0