Abstract
Background
Endoscopic submucosal dissection (ESD) is the treatment of choice for colorectal neoplasms in Japan. ESD can completely peel off the lesion and is associated with a significantly lower recurrence rate of colorectal cancers than EMR and is widely used to treat gastrointestinal tumors. This study aimed to evaluate in vivo traction in endoscopic submucosal dissection (ESD) of proximal colon lesions.
Methods
This retrospective study included patients with lesions in the proximal colon who received ESD treatment at Qilu Hospital of Shandong University from June 2018 to December 2020. Patients were divided into two groups according to the in vivo traction method (orthodontic ring or elastic ring) during operation. The operation time, dissection time, proportion of complete resection of lesions, and complications were compared between the two groups.
Results
There were 28 patients in this study. In the orthodontic ring group (n = 10), the average lesion diameter was 2.0–2.5 cm, and the average operation and dissection times were 26.5 ± 7.47 and 21.5 ± 7.47 min, respectively. In the elastic ring group (n = 18), the average lesion diameter was 2.5–5.5 cm, and the average operation and dissection times were 27.39 ± 11.83 and 22.39 ± 11.83 min, respectively. All lesions were completely resected in a single operation, and no wound perforation and delayed bleeding occurred.
Conclusion
In vivo traction-assisted ESD can be used to resect proximal colon lesions in selected patients (precancerous lesions and early colon cancer limited to the mucosa or with a submucosa infiltration depth of < 1000 µm).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic submucosal dissection (ESD) is the treatment of choice for colorectal neoplasms in Japan. ESD has evolved from endoscopic mucosal resection (EMR) [1]. ESD can completely peel off the lesion and is associated with a significantly lower recurrence rate of colorectal cancers than EMR and is widely used to treat gastrointestinal tumors [2]. As a result, there has been an increase in the medical facilities that offer ESD. Unlike EMR, however, ESD has high technical requirements with a long operation time, and it is associated with more complications than EMR, such as hemorrhage, perforation, lumen stenosis, and postoperative infection. As ESD requires more technical skills, mastering this technology requires a long time, and the strict admission standards limit its widespread application [3]. However, the thinner colonic walls, particularly in the proximal colon, the presence of flexures and folds, and peristaltic movements of the colon render colorectal ESD particularly challenging compared to ESD of cancers in other anatomic locations [4, 5].
Along with other advances in devices and techniques of ESD in recent years, several traction devices have been developed to overcome the challenges encountered in this procedure. Some traction techniques used for colorectal ESD were limited to sigmoid-rectal lesions [6]. In 2011, dental floss traction assistance was used in the ESD of gastric tumors to obtain good operational vision in Taiwan [7]. In 2014, “dental floss” traction assistance was found to shorten operation time in animal experiments [8] effectively. However, this dental floss traction technique, which is commonly used, requires the repetitive back-and-forth movement of the endoscope. The proximal colon is far from the anus, and such repetitive movement of the endoscope can lead to intestinal spasms, prolonging operation time. Since 2018, our center has begun to use orthodontic ring traction to assist ESD, and the submucosa can be satisfactorily exposed under endoscopy. However, for large lesions, orthodontic ring traction cannot continuously assist in exposing the submucosa.
In 2011, Matsumoto et al. designed a medical ring to assist during ESD [9]. It is an inert elastic band that can be passed through the instrument channel of a standard endoscope. This ring is easy to mount and use for maintaining a direct vision of the resected site while performing ESD. We performed ESD with the aid of an elastic ring, and the elastic ring could be retracted to expose the submucosa throughout the procedure.
Generally, ESD is considered complex because of the inability to lift the mucosa due to the absence of counter traction. If traction is used to lift the mucosa intraoperatively, the surgeons can obtain clear visibility of the submucosa of the colon. The enhanced visibility will help greatly reduce the difficulty of performing ESD. Therefore, traction devices aim to provide better visibility and shorten operation time, and consequently, complications in ESD are minimized. Therefore, in the present study, we intended to analyze the effects and complications of ESD for proximal colon lesions performed with the aid of orthodontic ring traction and elastic ring traction.
Materials and methods
Patients
This retrospective study included patients with lesions in the proximal colon who underwent ESD at the Department of Gastroenterology, Qilu Hospital of Shandong University, Qingdao, China, from June 2018 to December 2020.
The inclusion criteria were as follows: (1) patients were over 18 years of age; (2) patients had large sessile colorectal polyps or laterally spreading tumors in the proximal colon; (3) the lesions were > 2.0 cm in diameter; (4) patients received ESD with an orthodontic ring or elastic ring traction assistance.
Patients with abnormal coagulation function, incomplete clinical data, or those who showed poor cooperation during colonoscopy were excluded from the study.
Grouping
The patients were divided into two groups based on the traction mode used during the operation: orthodontic ring (Supplementary Figure S1) or elastic ring. In the present study, the orthodontic ring traction approach was used to assist ESD in patients with smaller lesions (≤ 2.5 cm), while the elastic ring traction was used to assist ESD in patients with larger lesions (> 2.5 cm). The elastic ring device traction can also be used to assist ESD in smaller lesions, but the orthodontic ring cannot be used for larger lesions. In our institution, once elastic ring traction was used to assist ESD, the use of orthodontic ring traction in ESD was discontinued.
ESD procedure
ESD surgery was performed for all patients by the same surgeon, a deputy chief physician who has 6 years of experience in ESD surgery.
The following devices were used for the surgery: Pentax i-5000 main machine, Pentax EG29-i10 endoscope, and a Q-Dual knife from Japan Olympus Company; a Micro-Tech rotatable soft tissue clip with repetitive open-close function (Nanjing Minimally Invasive Company, China), an elastic ring (patent number: ZL 2020 2 0,016,729.9); and a VIO-200S high-frequency electric knife (ERBE Company, Germany).
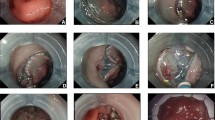
The lesion boundary was identified after staining the lesion and subsequently magnifying the endoscopic images. Epinephrine and methylene blue saline (1:10,000) were injected submucosally at the root of the lesion to lift the lesion fully. The mucosa around the lesion was resected. A tissue clamp was used to clamp the orthodontic ring or elastic ring, sent into the intestinal cavity via the biopsy channel, and fixed on the anal side of the lesion (orthodontic ring traction was applied for lesions ≤ 2.5 cm, and elastic ring traction was applied for lesions > 2.5 cm). Another tissue clamp was applied to clamp and tighten the free end of the orthodontic ring or elastic ring. It was fixed on the mucosa on the opposite side of the lesion as the patient inhaled, and the lesion was pulled up to expose the submucosa. The lesion was then completely resected. Then, electrothermal hemostatic forceps were used to manage vascular stump bleeding. An endoloop or hot hemostatic forceps was used to assist in releasing from the orthodontic ring or traction ring to completely resect the lesion (Figs. 1 and 2 and Video 1).
Laterally developed tumor in the hepatic flexure of the colon (1.5 × 1.8 cm). A Visual field under the endoscope; B The orthodontic rings are fixed on one side of the lesion; C Another tissue clip is used to fix the orthodontic ring on the opposite mucosa when the patient inhaled, exposing the submucosa after traction; D dissection process; E wound surface after dissection; F Dissected lesion tissue (2.0 × 2.0 cm)
Data collection
Demographic data, lesion information (location, diameter, pathological diagnosis, and morphology), operation time, dissection time, and proportion of complete resection by once were collected and compared between the two groups. Complications were assessed, including perforation and delayed bleeding (within 72 h after operation). Six months postoperatively, the patients returned to the outpatient department and underwent follow-up colonoscopic assessment. The patients were followed up until May 2021 (Tables 1 and 2).
Statistical analysis
Data were statistically analyzed using SPSS 20.0 (IBM, Armonk, NY, USA). Continuous variables were tested for normality. Normally distributed variables were expressed as means ± standard deviation, and an independent-sample t test was used to compare the two groups. Data with non-normal distribution were expressed as medians (range), and the Mann–Whitney U test was used to compare the two groups. The classification variables were expressed as n (%), and the two groups were compared by chi-square test or Fisher exact test. P < 0.05 was considered statistically significant.
Results
This study included 28 patients ranging from 45 to 72 years of age who underwent ESD for lesions in the proximal colon. The patients were divided into two groups depending on the type of traction used: 10 patients were placed in the orthodontic ring group and 18 in the elastic ring group.
In the orthodontic ring group, two of the lesions were located in the ascending colon, three in the transverse colon, two in the hepatic flexure of the colon, and three in the cecum. The average lesion diameter was 2.0–2.5 cm. The mean operation time was 26.5 ± 7.5 min, and the mean dissection time was 21.5 ± 7.5 min. Results of the pathological analysis revealed that there were two cases of hyperplastic polyps, three villous adenomas, one lipoma, and four tubular adenomas.
In the elastic ring group, five cases were located in the ascending colon, seven in the transverse colon, three in the hepatic flexure of the colon, and three in the cecum. The average lesion diameter was 2.5–5.5 cm. The mean operation time was 27.4 ± 11.8 min, and the mean dissection time was 22.4 ± 11.8 min. Pathological results revealed nine cases of tubular adenoma, five cases of villous adenoma, three cases of traditional serrated adenoma, and one case of hyperplastic polyp.
All the lesions were completely resected in a single operation, and no wound perforation and delayed bleeding occurred in any of the cases in both groups.
Discussion
In the present study, we presented a comparative analysis of ESD assisted with orthodontic ring traction and elastic ring traction. Our results found that the operation and dissection times were both slightly shorter in the orthodontic ring group than in the elastic ring group. Furthermore, there were no complications among the patients regardless of the type of traction used. ESD of patients with proximal colon lesions using both the traction devices tested in this study (orthodontic ring traction and elastic ring traction) resulted in good outcomes. Of note, this study only included patients with precancerous lesions, colon cancers limited to the mucosa, or colon cancers with a submucosa infiltration depth of < 1000 µm.
In the present study, the orthodontic ring traction approach was used to assist ESD in patients with smaller lesions, while the elastic ring traction was used to assist ESD in patients with larger lesions. The elastic ring device traction can also be used to assist ESD in smaller lesions, but the orthodontic ring cannot be used for larger lesions. In Qilu Hospital of Shandong University, once elastic ring traction was used to assist ESD, the use of orthodontic ring traction in ESD was discontinued.
Like traditional surgical treatment, a good surgical field of vision is a prerequisite for the safety of endoscopic surgery. In the process of ESD treatment of colonic lesions, operators need to have a careful judgment of submucosa. Blind cutting will only increase the risk of perforation and hemorrhage. In ESD surgery, a transparent cap is routinely used against the submucosa for peeling [10,11,12]. For improved exposure of the submucosa, it is necessary to master skills such as the direction of gravity of the lesion. Furthermore, surgeons need to be cautious due to the relatively thin colorectal walls, which increase the risk of perforation during ESD surgery. Undoubtedly, it is an ESD site featuring relatively high difficulty.
Several traction devices and techniques have been developed for use in colorectal ESD. These include S–O clips [13], ring-thread counter traction [14], cross-counter technique [15], clip-and-snare [16], and clip flap [17]. However, due to the heterogeneities of the inclusion eligibility of the lesions and traction devices, it is difficult to perform a meta-analysis of the data.
Floss traction can more clearly expose the submucosa while displaying the submucosal blood vessels. Thus, using floss traction with ESD can help avoid complications such as bleeding and perforation. Floss traction technology has obvious advantages in shortening the ESD operation time, reducing complications such as bleeding and perforation, and improving the en bloc resection rate and complete resection rate [18]. ESD surgery is often performed with the aid of external floss traction both in China and internationally [19,20,21]. During the operation, it is necessary to conduct repeated withdrawal and entry of the endoscope. External traction can be conveniently applied to esophageal, stomach, and left colon lesions. After the repeated entry and withdrawal in the floss traction technique, an intestinal spasm will occur in lesions of the proximal colon, increasing the difficulty of entry, prolonging the operation time, and increasing the operation complications. The internal traction of the orthodontic ring can save the step of endoscope entry and withdrawal, directly sending the orthodontic ring into the intestinal cavity through the endoscopic biopsy hole, better exposing the submucosa through the internal traction, thereby ensuring the safety of the ESD surgery and improving the stripping efficiency. However, since orthodontic ring traction cannot continuously maintain traction force with the expansion of stripping range in larger lesions, the elastic traction ring is more advantageous compared to the orthodontic ring due to its elastic retraction capability, with which it can continuously maintain traction force, which is beneficial to ESD surgery, particularly for large lesions. In addition, the cost of an elastic ring is relatively low (USD 0.5/ring), which does not increase the economic burden on the patients.
This study has several limitations. First, it was performed retrospectively. In the future, prospective, randomized studies are required to obtain further insights into the safety and efficacy of these two methods to assist ESD of proximal colon lesions. Second, this study was performed at a single center. Third, the sample size of this study is very small. Future multicenter studies with a larger sample size could validate our findings and expand upon them.
In conclusion, our findings suggest that in vivo traction-assisted ESD can be used for the resection of lesions of the proximal colon. This study only included patients with precancerous lesions, colon cancers limited to the mucosa, or colon cancers with a submucosa infiltration depth of < 1000 µm. Therefore, in vivo traction-assisted ESD should be used in selected patients.
References
Kaimakliotis PZ, Chandrasekhara V (2014) Endoscopic mucosal resection and endoscopic submucosal dissection of epithelial neoplasia of the colon. Expert Rev Gastroenterol Hepatol 8:521–531
Kim YJ, Kim ES, Cho KB, Park KS, Jang BK, Chung WJ, Hwang JS (2013) Comparison of clinical outcomes among different endoscopic resection methods for treating colorectal neoplasia. Dig Dis Sci 58:1727–1736
Tsuji Y, Fujishiro M, Kodashima S, Niimi K, Ono S, Yamamichi N, Koike K (2014) Desirable training of endoscopic submucosal dissection: further spread worldwide. Annal of Translat Med 2:27
Saito Y, Otake Y, Sakamoto T, Nakajima T, Yamada M, Haruyama S, So E, Abe S, Matsuda T (2013) Indications for and technical aspects of colorectal endoscopic submucosal dissection. Gut Liver 7:263–269
Abe S, Wu SYS, Ego M, Takamaru H, Sekiguchi M, Yamada M, Nonaka S, Sakamoto T, Suzuki H, Yoshinaga S, Matsuda T, Oda I, Saito Y (2020) Efficacy of current traction techniques for endoscopic submucosal dissection. Gut Liver 14:673–684
Uraoka T, Ishikawa S, Kato J, Higashi R, Suzuki H, Kaji E, Kuriyama M, Saito S, Akita M, Hori K, Harada K, Ishiyama S, Shiode J, Kawahara Y, Yamamoto K (2010) Advantages of using thin endoscope-assisted endoscopic submucosal dissection technique for large colorectal tumors. Digestive Endosc 22:186–191
Li C-H, Chen P-J, Chu H-C, Huang T-Y, Shih Y-L, Chang W-K, Hsieh T-Y (2011) Endoscopic submucosal dissection with the pulley method for early-stage gastric cancer (with video). Gastrointest Endosc 73:163–167
Aihara H, Kumar N, Ryou M, Abidi W, Ryan MB, Thompson CC (2014) Facilitating endoscopic submucosal dissection: the suture-pulley method significantly improves procedure time and minimizes technical difficulty compared with conventional technique: an ex vivo study (with video). Gastrointest Endosc 80:495–502
Matsumoto K, Nagahara A, Sakamoto N, Suyama M, Konuma H, Morimoto T, Sagawa E, Ueyama H, Takahashi T, Beppu K, Shibuya T, Osada T, Yoshizawa T, Ogihara T, Watanabe S (2011) A new traction device for facilitating endoscopic submucosal dissection (ESD) for early gastric cancer: the “medical ring.” Endoscopy 43(Suppl 2):E67–E68
Wang J, Lin S, Qiao W, Liu S, Zhi F (2021) Clinical outcomes of cap-assisted endoscopic resection for small rectal subepithelial tumors. Gastroenterol Hepatol 44:418–423
Zhang D-G, Luo S, Xiong F, Xu Z-L, Li Y-X, Yao J, Wang L-S (2019) Endoloop ligation after endoscopic mucosal resection using a transparent cap: A novel method to treat small rectal carcinoid tumors. World J Gastroenterol 25:1259–1265
Zheng Z, Jiao G, Wang T, Chen X, Wang B (2016) Ligation-Assisted Endoscopic Enucleation for the Resection of Gastrointestinal Tumors Originating from the Muscularis Propria: Analysis of Efficacy and Facility. Dig Surg 33:488–494
Sakamoto N, Osada T, Shibuya T, Beppu K, Matsumoto K, Mori H, Kawabe M, Nagahara A, Otaka M, Ogihara T, Watanabe S (2009) Endoscopic submucosal dissection of large colorectal tumors by using a novel spring-action S-O clip for traction (with video). Gastrointest Endosc 69:1370–1374
Mori H, Kobara H, Nishiyama N, Fujihara S, Matsunaga T, Masaki T (2017) Novel effective and repeatedly available ring-thread counter traction for safer colorectal endoscopic submucosal dissection. Surg Endosc 31:3040–3047
Okamoto K, Muguruma N, Kitamura S, Kimura T, Takayama T (2012) Endoscopic submucosal dissection for large colorectal tumors using a cross-counter technique and a novel large-diameter balloon overtube. Dig Endosc 24(Suppl 1):96–99
Yamada S, Doyama H, Ota R, Takeda Y, Tsuji K, Tsuji S, Yoshida N (2016) Impact of the clip and snare method using the prelooping technique for colorectal endoscopic submucosal dissection. Endoscopy 48:281–285
Yamamoto K, Hayashi S, Saiki H, Indo N, Nakabori T, Yamamoto M, Shibuya M, Nishida T, Ichiba M, Inada M (2015) Endoscopic submucosal dissection for large superficial colorectal tumors using the “clip-flap method.” Endoscopy 47:262–265
Jeon WJ, You IY, Chae HB, Park SM, Youn SJ (2009) A new technique for gastric endoscopic submucosal dissection: peroral traction-assisted endoscopic submucosal dissection. Gastrointest Endosc 69:29–33
Zeng C, Zhu Y, Shu X, Lv N, Cai Q, Chen Y (2019) Endoscopic resection of gastric submucosal masses by a dental floss traction method. Can J Gastroenterol Hepatol 2019:1083053
Nomura T, Kamei A, Sugimoto S, Oyamada J (2018) Colorectal endoscopic submucosal dissection using the “dental floss with rubber band method.” Endoscopy 50:E78–E80
Yoshida M, Takizawa K, Ono H, Igarashi K, Sugimoto S, Kawata N, Tanaka M, Kakushima N, Ito S, Imai K, Hotta K, Matsubayashi H (2016) Efficacy of endoscopic submucosal dissection with dental floss clip traction for gastric epithelial neoplasia: a pilot study (with video). Surg Endosc 30:3100–3106
Acknowledgements
None.
Funding
This study was supported by Qingdao Municipal Medical Research Guidance Plan in 2019 (Grant No.2019-WJZD161).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Aijun Zhang, Yanjun Song, Xiangdan Cui, Baihui Wang, and Ruyuan Li have no conflict of interest to disclose.
Ethical approval
This study was approved by the Ethics Committee of Qilu Hospital of Shandong University [No: KYLL-2020043], and the need for informed consent was waived by the review board due to the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
464_2022_9266_MOESM1_ESM.docx
Supplementary file1 Figure S1. The traction orthodontic ring. The large hole has a diameter of 8 mm. The small hole has a diameter of 2 mm (DOCX 2519 kb)
Supplementary file2 Video 1 In vivo traction-assisted resection of a proximal colon lesion (MP4 400489 kb)
Rights and permissions
About this article
Cite this article
Zhang, A., Song, Y., Cui, X. et al. Application of in vivo traction-assisted resection of proximal colon lesions: a case series (with video). Surg Endosc 36, 8231–8236 (2022). https://doi.org/10.1007/s00464-022-09266-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09266-y