Abstract
Background/Aim
Endoscopic treatments of colorectal neoplasms have yet to be standardized. This study aimed to compare efficacy and tolerability of different endoscopic resection methods for colorectal epithelial tumors.
Methods
Patients with non-pedunculated colorectal tumors undergoing endoscopic treatments were consecutively enrolled, and their medical records were reviewed retrospectively. The resection methods were classified into three groups: endoscopic mucosal resection with circumferential precutting (EMR-P), endoscopic submucosal dissection with snaring (ESD-S), and endoscopic submucosal dissection alone (ESD). We compared en bloc resection, pathological complete resection, and complications associated with these methods.
Results
Overall, 206 lesions from 203 patients were included in the study (mean size 25.2 ± 10.1 mm). The number of lesions treated with EMR-P, ESD-S, and ESD was 91 (44.2 %), 57 (27.7 %), and 58 (28.2 %), respectively. There was a significant difference in both the en bloc resection rates (EMR-P, 61.5 %; ESD-S, 64.9 %; ESD, 96.6 %; p = 0.001) and complete resection rates (EMR-P, 51.6 %; ESD–S, 54.4 %; ESD, 75.9 %; p = 0.009). Bleeding and perforation were less frequently observed in the EMR-P group. In the subgroup-analysis of lesions less than 20 mm, however, these differences were not observed.
Conclusions
All endoscopic resection methods, including EMR-P, ESD-S, and ESD, were effective and safe for the treatment of colorectal neoplasms. Technically demanding ESD with high en bloc and complete resection rate should be reserved for the suspicious cancer lesion, which requires the precise histological evaluation. EMR-P with good feasibility can be considered an alternative to ESD for the lesions less than 20 mm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conventional endoscopic mucosal resection (EMR), simple snaring after submucosal solution injection, is one of the effective treatments for colorectal epithelial lesions [1]. For lesions larger than 2 cm, however, the rate of piecemeal resection obviously increases with EMR, leading to a high frequency of local recurrence [2]. In addition, the piecemeal-resected specimen makes precise histologic evaluation difficult [2]. Therefore, endoscopic submucosal dissection (ESD) has been increasingly used to overcome the disadvantage of EMR in the gastrointestinal tract. ESD was originally developed for the treatment of large or ulcerative gastric epithelial neoplasm [3] and provides more favorable outcomes regarding en bloc resection, irrespective of lesion size [4]. However, this technique has a number of shortcomings, such as the technical difficulty of the procedure, long procedure time, and high frequency of complications, compared to the conventional EMR. Furthermore, ESD requires more technical skill when used to treat lesions in the colorectal area because of the unique anatomical characteristics of the colon, including the thin wall, sparse muscle layer, and tortuous folds. Therefore, ESD has not yet been accepted as a standard therapeutic alternative for treating colorectal neoplastic lesions [5].
EMR after circumferential precutting (EMR-P) was first introduced to overcome the drawbacks of EMR, with an attempt to allow en bloc resection of the large gastric epithelial neoplastic lesions [6, 7]. ESD with snaring (ESD-S) was known as a simplified modification to ESD, using a snare at the final stage to grasp and to quickly remove the undissected submucosal tissue that remained after standard submucosal dissection with the electric knives [8]. We assumed that these modified resection methods, i.e., EMR-P and ESD-S, might be located in between conventional EMR and ESD, in terms of both technical difficulty grade and favorable outcomes, such as en bloc resection. Although several studies have compared the efficacy and complication rate between two endoscopic resection methods, such as conventional EMR or ESD, a comparison of outcomes between other different endoscopic resection methods in the colorectum has not been previously reported. Thus, the aim of this study was to compare the efficacy and tolerability of different endoscopic resection methods including EMR-P, ESD-S, and ESD, for the treatment of colorectal epithelial tumors.
Patients and Methods
Patients and Study Design
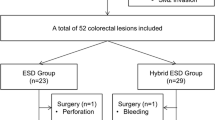
Between March 2007 and March 2011, the records of 264 consecutive patients with non-pedunculated colorectal tumors who underwent endoscopic resection procedures at the Keimyung University Dongsan Hospital in Daegu, South Korea, were reviewed. Patients with carcinoid tumors (n = 29) or inflammatory polyps (n = 13), or those who were managed with only conventional EMR (n = 19) were excluded, and a total of 203 patients were enrolled in this study (Fig. 1). Written informed consent was obtained from all patients before the procedure. We retrospectively analyzed the medical records of the participants, including demographic and clinicopathologic features, and compared en bloc resection, pathologic complete resection, complications, and local recurrence rates, according to the different endoscopic resection methods. This study protocol was approved by the Institutional Review Board of Keimyung University Dongsan Hospital.
Endoscopic Examinations
Endoscopic Procedure and Techniques
Colonoscopy was performed after bowel preparation with 4 l of polyethylene glycol solution (Taejun Pharm, Seoul, South Korea). Conscious sedation was achieved with intravenous administration of 0.1 mg/kg midazolam (Bukwang Pharm, Seoul, South Korea) and 50 mg of meperidine (Jeil Pharm, Seoul, South Korea). The procedure was mainly performed with a single-channel lower gastrointestinal endoscope (CF Q260AI; Olympus Optical Co., Tokyo, Japan). In routine practice, a solution of 0.9 % normal saline with epinephrine (1:10,000) was injected into the submucosal layer to facilitate and sustain submucosal elevation. Small amounts of indigo carmine were added to the solution to improve the visibility of the submucosal layer. The main electrosurgical knives used were a flex knife (Kachu Technology, Seoul, South Korea) and a hook knife (Olympus, Tokyo, Japan). We used the flex knife to make a circumferential incision. For more difficult cases, the hook knife was used in combination with the flex knife. The electrosurgical unit used in this study was an ICC200 or VIO300D high-frequency generator (Erbe Elektromedizin, Tübingen, Germany), which generated a special cutting current with the ENDOCUT mode (effect 3, cut duration 2, cut interval 6) and dissection current with the swift mode (effect 4, max Watts 45). Endoscopic treatments were performed by three experienced endoscopists (K.B.C., K.S.P., and E.S.K.) who had performed more than 3,000 cases of colonoscopic procedures prior to this study.
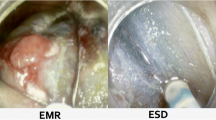
The resection methods used in this study were classified into three groups: endoscopic mucosal resection with circumferential precutting (EMR-P), endoscopic submucosal dissection with snaring (ESD-S), and endoscopic submucosal dissection alone (ESD). The selection of the method was at the endoscopist’s discretion. EMR-P was mainly used to treat lesions for which either the simple snaring technique or conventional EMR was impractical, due to a tumor size larger than the diameter of the snare or difficult location. Mucosal incision (i.e., precutting) was carried out with the flex knife all around the lesion. Then, the snare (Mei-glove, Achenmühle, Germany) was applied to this circumferential incision line around the lesion. After making sure of grasping the lesion, we removed the tumor in the same manner as with the standard snare polypectomy technique (Fig. 2). We described the ESD method previously [9]. Briefly, after submucosal layer elevation with injection, the flex knife was used to make a circumferential incision. Dissection started at the lateral edges and proceeded through the lifted submucosal layer until the lesion was resected in one piece (Fig. 3). If there was difficulty due to poor submucosal elevation, we used the hook knife for safer dissection under direct observation. ESD-S involved the resection of tumors by snaring at the final stage, where the remnant attached submucosal tissue was less than a quarter after circumferential submucosal dissection method progressed (Fig. 4). The main indications of this method were the possible cases of fast resection for which snaring of the remnant undissected submucosal area seemed easy or the cases that required prompt completion of the procedure, especially when complications, such as perforation or bleeding, developed during submucosal dissection. This method was also used to complete the resection in lesions where it was difficult to further dissect because of location or accompanying submucosal fibrosis, which could have resulted in a higher risk for complication with ESD [10, 11].
A case treated by endoscopic mucosal resection with precutting (EMR-P) method. a A polypoid lesion 20 mm in diameter is seen in the proximal rectum. b After submucosal injection, a circumferential mucosal incision is performed to separate the lesion from the surrounding non-neoplastic mucosa. c The lesion is ensnared and resected using the snare. d The resected specimen fixed at a plate
A case treated by endoscopic submucosal dissection (ESD) method. a A laterally spreading tumor (LST)—granular (G) type over 40 mm in size is seen in the rectum. b, c The lesion is being dissected through submucosal layer after injection with indigo carmine dye. d The resected specimen fixed at a plate
A case treated by endoscopic mucosal dissection with snaring (ESD-S) method. a A 30-mm laterally spreading tumor (LST)—granular (G) type is seen in the sigmoid colon. b The dissection is performed after submucosal injection. c The lesion with remnant submucosal area less than a quarter after submucosal dissection is ensnared. d The resected specimen fixed at a plate
After the tumor was resected, hemostatic forceps (SDB2422, Pentax or FD-410LR, Olympus) and argon plasma coagulation (APC) were used to prevent delayed bleeding. Simple abdominal X-rays and laboratory testing were performed in all patients immediately after ESD and on the following day.
Tumor Definition and Location
The endoscopic appearance of the tumor was classified according to the Japanese Research Society criteria [12]. Laterally spreading tumors (LST) were defined as lesions 10 mm in size or larger with a low vertical axis and extending laterally along the interior luminal wall [13]. Macroscopically, the tumors were divided into protruding large tumors (type O–I) and two subtypes of LST of granular and non-granular type, according to Kudo’s classification [14]. Tumor locations were classified as the right colon (cecum to ascending colon), left colon (transverse colon and descending colon), and rectosigmoid area, based on the Japanese Classification of Colorectal Carcinoma [12]. The lesion size was estimated using the open biopsy forceps as a reference.
Histological Examination
Each resected specimen was stretched and pinned to a 5-mm-thick polystyrene foam plate. The specimen was fixed with 10 % formalin, cut into 2-mm-wide strips perpendicular to the base and embedded in paraffin. Each strip was cut into 3-μm-thick sections, which were subsequently stained. Histological diagnoses of the lesions were made by a pathologist, based on the Vienna classification [15]. En bloc resection was defined as the removal of the lesion in a single piece. Extension of tumor cells into the resected margin was evaluated. Pathologic complete resection was defined when the tumor cells were not identified within at least 1 mm from the lateral and deep resection margins (en bloc resection was essential).
Patient Follow-Up
Patients were allowed to sip water followed by a light meal, if symptoms, laboratory findings, and abdominal X-ray were unremarkable. Follow-up colonoscopy or sigmoidoscopy was usually preformed about 3–6 months after endoscopic resection to confirm that post-procedure ulcers were healing and to exclude the presence of residual tumors. Annual colonoscopy was recommended to check for local recurrence or secondary primary tumors. Patients with histologically confirmed adenocarcinoma were regularly followed-up for surveillance with chest X-ray and abdomino-pelvic CT scans to monitor for either regional or distant metastasis.
Statistical Analysis
Data management and statistical analyses were performed with SPSS software version 15.0 (SPSS, Inc., Chicago, IL, USA). Rates and proportions were calculated to determine categorical variables. Statistical analysis among groups was performed using the Fisher’s exact or Chi-square (χ2) test. To compare continuous variables among groups, ANOVA test was used as appropriate. p values <0.05 were considered to indicate statistically significant differences.
Results
Patients and Clinical Characteristics
Procedures were performed on a total of 206 colorectal epithelial lesions from 203 consecutive patients. The mean age was 62.0 years (range, 31–87 years). There were 122 men (60.7 %) and 81 women (39.3 %). The number of lesions treated with EMR-P, ESD-S, and ESD method was 91 (44.2 %), 57 (27.7 %), and 58 (28.2 %), respectively. Laterally spreading tumors were the most common tumor type (156/206, 75.7 %) followed by polypoid tumors (50/206, 24.3 %). The overall mean size of the tumors was 25.2 ± 10.1 mm and the mean size of tumors treated with ESD was the largest (30.6 ± 10.6 mm; range, 10–64 mm), followed by those treated with ESD-S (26.4 ± 9.8 mm; range, 10–62 mm) and EMR-P (20.9 ± 7.9 mm; range, 10–42 mm) (p = 0.001). Based on the analysis of tumor location according to the methods, ESD was mainly performed in the rectosigmoid area (84.5 %). One hundred and fifteen (55.8 %) lesions were adenoma and 91 (44.2 %) were adenocarcinoma. Among the lesions of adenocarcinoma, 67 (32.5 %) lesions invaded only into the mucosal layer, whereas 24 (11.7 %) extended into the submucosal layer. There was no significant difference in the histopathological diagnosis between different endoscopic procedures (Table 1).
Procedure-Related Outcomes
Procedure time of ESD was significantly longer than those of the other groups and procedure time decreased in order of ESD, ESD-S, and EMR-P method (65.93 ± 43.8, 63.9 ± 43.1, and 30.0 ± 30.5 min, respectively, p = 0.001) (Table 2).
The overall en bloc resection rate was 72.3 %. The en bloc resection rate of ESD was the highest among groups and it decreased stepwise in order of ESD-S and EMR-P (96.6, 64.9, and 61.5 %, respectively, p = 0.001). There was also a significant difference in the pathological complete resection rate of ESD, ESD-S, and EMR-P (75.9, 54.4, and 51.6 %, respectively, p = 0.009), with the overall complete resection rate 59.2 %.
Table 3 summarizes the en bloc and complete resection rates of the different methods according to lesion size. For lesions equal to or less than 20 mm, there was no significant difference in en bloc and complete resection rates between the three groups.
Complication Rates
The main complications of ESD were perforation and bleeding, as previously reported [5]. Complications occurred during the procedure in 37 lesions (17.9 %) with bleeding in 12 (5.8 %) and perforation in 25 (12.1 %). The bleeding and perforation rates of ESD, ESD-S, and EMR-P were 8.6 and 15.5, 10.5 and 19.3, and 1.1 and 5.5 %, respectively. The complication rate of ESD, especially ESD–S, was significantly higher than that of EMR-P (Table 4).
However, in the subgroup analysis of the lesion size equal to or less than 20 mm, these differences were not observed between different endoscopic method groups.
Bleeding was managed by hemostatic forceps and metal clips (Olympus, Tokyo, Japan). No patient developed massive hemorrhage requiring blood transfusion. All perforation cases were able to be conservatively managed. Perforation confirmed during the procedure was treated by application of metal clips, with nothing per mouth and intravenously administered antibiotics. When perforation was confirmed by CT of X-ray after the procedure, patients were under close observation with nothing per mouth and intravenously administered nutrients and antibiotics.
Follow-Up
For all the lesions, we successfully obtained information about local recurrence with colonoscopy, which was performed more than 6 months after the initial procedures. The median time between the procedure and final colonoscopy was 19.6 months (interquartile range 6–60 months). During the follow-up period, we found no evidence of local recurrence in any case. However, there was one case of regional lymph node metastasis from the ESD group diagnosed 30 months after the resection procedure.
Discussion
Traditionally, surgical resection has been used to treat colorectal tumors. Advances in endoscopic instruments and techniques have increased the rates of the detection of early colorectal carcinoma or precancerous lesions, and have led to a large increase in the number of endoscopically resected lesions [14, 16]. Although typical endoscopic resection methods are represented by EMR and ESD, a wide range of endoscopic resection techniques (e.g., cap-associated EMR [EMR-C], EMR with ligation [EMR-L], EMR-P, and ESD-S) have been introduced for the management of epithelial neoplasms in the gastrointestinal tract [17]. Among them, EMR-P was used for the treatment of gastric neoplasia to deal with the disadvantages of the conventional EMR method, such as high rate of piecemeal or incomplete resection. EMR-P showed the clear benefit of relatively high rate of en bloc resection, compared with the conventional EMR method, for the treatment of gastric tumors [7]. Although ESD has the great advantage of a considerably high rate of both en bloc and complete resection, allowing precise histopathologic evaluation of the resected specimen, it shows its own shortcomings, including technical difficulty, prolonged procedure time, and high complication rate, particularly when performed in the colorectal area. To address these issues, ESD-S, a simplified modification technique to ESD, has been introduced. ESD-S showed shorter procedure time than the ESD method for the treatment of colorectal neoplasms, while ESD had still a significantly higher rate of en bloc resection than ESD-S [8]. To the best of our knowledge, this is the first study to compare clinical outcomes of these different endoscopic resection methods, including EMR-P, ESD-S, and ESD, for the management of colorectal neoplasm. The present study demonstrated that there was a significant difference between these methods regarding en bloc resection rate, complete resection rate, and complication rate. In the lesions ≤20 mm, however, this difference was not observed.
There have been several reports in the literature comparing the outcomes of different endoscopic resection methods. Toyonaga et al. [18] reported comparative results of three different endoscopic methods for colorectal tumor treatments, i.e., EMR with small incision (EMR with SI), simplified ESD (similar to ESD-S of our study), and ESD. They introduced a new method, EMR with SI, which was different from EMR-P in that only a small mucosal incision was made on the oral side of the lesion for the fixed anchoring of the tip of snare, instead of a circumferential incision surrounding the lesion. In their study, the en bloc resection rate increased stepwise in the order of EMR with SI, simplified ESD and ESD (83.3, 90.9, and 98.9 %, respectively), while the procedure time increased in the same order (19, 27, and 60 min, respectively). They conducted EMR with SI and simplified ESD only when reliable snaring was possible in the lesion. This potential selection bias might explain the higher en bloc resection rate of EMR with SI and simplified ESD in their study, compared to EMR-P and ESD-S in our study. Another study by Byeon et al. [8], comparing ESD-S and ESD for the treatment of colorectal neoplasms, revealed that the en bloc resection rate of ESD was higher than that of ESD-S (87 vs. 64 %, p < 0.01), and that this difference between ESD and ESD-S groups was not observed for lesions of <20 mm, which was consistent with our results. They reported that complication rates were not different between the ESD and ESD-S groups. In the present study, the complication rate was significantly lower in the EMR-P group, compared with ESD-S and ESD groups (bleeding rates of EMR-P, ESD-S, and ESD were 1.1, 10.5, and 8.6 %, respectively, p = 0.033; perforation rates of EMR-P, ESD-S, and ESD were 5.5, 19.3, and 15.5 %, respectively, p = 0.028) (Table 4). Interestingly, the complication rate of ESD-S was higher than that of ESD group, and this finding might be attributed to the fact that we changed the ESD-S technique by using a snare to complete the procedure quickly, when complications developed during submucosal dissection. However, this difference in the complication rate between the investigated groups disappeared for the lesions ≤20 mm. All cases with complication could be managed conservatively.
There was no case of local recurrence during the follow-up period. Unexpectedly, we found one case of regional lymph node metastasis in the ESD group, detected by abdomino-pelvic CT scan 30 months after the procedure, without any remnant lesion at the resection site. This lesion had been removed completely as en bloc resection by ESD method and histologically confirmed as differentiated adenocarcinoma confined to the mucosa layer (within lamina propria). There was no angiolymphatic invasion. We reported this case briefly as a case report [19].
In our study, the en bloc resection rate of EMR-P was higher than those of conventional EMR of other studies [2, 20]. In addition, we found the stepwise increase in en bloc resection, complete resection, and procedure time in the order of EMR-P, ESD-S, and ESD. In this context, we postulate that modified resection methods, i.e., EMR-P and ESD-S, might be located in between conventional EMR and ESD, in terms of both technical difficulty grade and favorable outcome, such as en bloc resection. Indeed, ESD is undoubtedly an ideal method for achieving en bloc resection, as described in other reports [5, 21–23]. However, considering the risks and benefits, ESD should be reserved for highly suspicious cancer lesions, particularly larger than 20 mm in size, which require precise histological evaluation. The present study revealed that both the en bloc and complete resection rates of EMR-P were not different from ESD for the lesions ≤20 mm. Therefore, we believe that the method might be an alternative option to ESD technique, which accommodates the difference between conventional EMR and ESD, and should also be considered as a nice step toward ESD. In line with the opinion of the present study, Matsuda et al. [17] reported that the prevalence of suitable lesions for colorectal ESD among all neoplastic lesions was lower than expected. They collected and analyzed a total of 11,488 colorectal neoplasms to clarify the prevalence of “definite indication for colorectal ESD, including potential candidates”. The prevalence of suitable lesions for ESD among all neoplastic lesions and all early cancers was not high (1.0 and 5.0 %, respectively), when considering problems such as the technical difficulty of this procedure, higher complication rates, and a relatively long procedure time. In addition, Fujishiro et al. [24] reported on suitable endoscopic options according to tumor characteristics. They suggested that piecemeal EMR might be more appropriate for some groups of large flat neoplasm, whereas ESD might be considered as the first-line treatment of lateral spreading tumor-non-granular-pseudodepressed (LST-NG-PD) lesions or those with submucosal fibrosis, so as not to leave tumor cells in the submucosa.
In clinical practice, it is important to select resection techniques depending on the status and characteristics of the lesion, the operator’s technical skill, calculated and required time for the procedure, and facilities in each hospital [13, 25]. To establish clinical standardization and safety guidelines for various endoscopic resection methods to direct endoscopists in the treatment of colorectal tumors, large randomized controlled comparative studies will be needed.
There are a few limitations to the present study. As design of study was retrospective, not randomized, the selection bias of the resection method could be present. In addition, the difference in the lesion size between groups may have influenced the outcomes of each procedure. Large-size lesions were mostly treated by ESD because resection methods with snare could not technically remove lesions >2 cm in one piece. The large size of lesions, therefore, resulted in longer procedure time and more complications in the ESD group than the EMR-P group. The size of lesions is one of the independent risk factors for complications of ESD in colorectal neoplasia [9]. Furthermore, due to the different enrolled population in this study, comparison of these three different methods might be less meaningful. As the data sample was relatively small and from a single tertiary teaching hospital, it was difficult to ensure consistency. A randomized comparative study with the large sample should be needed to confirm the results of this study.
In conclusion, endoscopic resection for the treatment of colorectal adenoma and early colorectal cancers may be a safe and effective modality. Technically demanding ESD with high en bloc and complete resection rate should be reserved for the suspicious cancer lesions, which requires precise histological evaluation. EMR-P with good feasibility may take a transitional role before performing ESD and be considered an alternative to ESD for lesions less than 20 mm.
References
Bergmann U, Beger HG. Endoscopic mucosal resection for advanced non-polypoid colorectal adenoma and early stage carcinoma. Surg Endosc. 2003;17:475–479.
Conio M, Repici A, Demarquay JF, et al. EMR of large sessile colorectal polyps. Gastrointest Endosc. 2004;60:234–241.
Fujishiro M. Endoscopic submucosal dissection for stomach neoplasms. World J Gastroenterol. 2006;12:5108–5112.
Gotoda T, Yamamoto H, Soetikno RM. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006;41:929–942.
Toyanaga T, Man IM, Ivanov D, et al. The results and limitations of endoscopic submucosal dissection for colorectal tumors. Acta Chir Iugosl. 2008;55:17–23.
Muto M, Miyamoto S, Hosokawa A, et al. Endoscopic mucosal resection in the stomach using the insulated-tip needle-knife. Endoscopy. 2005;37:178–182.
Min BH, Lee JH, Kim JJ, et al. Clinical outcomes of endoscopic submucosal dissection (ESD) for treating early gastric cancer: comparison with endoscopic mucosal resection after circumferential precutting (EMR-P). Dig Liver Dis Off J Italian Soc Gastroenterol Italian Assoc Study Liver. 2009;41:201–209.
Byeon JS, Yang DH, Kim KJ, et al. Endoscopic submucosal dissection with or without snaring for colorectal neoplasms. Gastrointest Endosc. 2011;74:1075–1083.
Kim ES, Cho KB, Park KS, et al. Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy. 2011;43:573–578.
Goto O, Fujishiro M, Kodashima S, et al. Feasibility of electrocautery snaring as the final step of endoscopic submucosal dissection for stomach epithelial neoplasms. Dig Liver Dis Off J Italian Soc Gastroenterol Italian Assoc Study Liver. 2009;41:26–30.
Nishiyama H, Isomoto H, Yamaguchi N, et al. Endoscopic submucosal dissection for colorectal epithelial neoplasms. Dis Colon Rectum. 2010;53:161–168.
[Anonymous]. General rules for clinical and pathological studies on cancer of the colon, rectum and anus. Part II. Histopathological classification. Japanese Research Society for Cancer of the Colon and Rectum. Japanese J Surg. 1983; 13:574–598.
Uraoka T, Saito Y, Matsuda T, et al. Endoscopic indications for endoscopic mucosal resection of laterally spreading tumours in the colorectum. Gut. 2006;55:1592–1597.
Kudo S. Endoscopic mucosal resection of flat and depressed types of early colorectal cancer. Endoscopy. 1993;25:455–461.
Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–255.
Iishi H, Tatsuta M, Narahara H, et al. Endoscopic resection of large pedunculated colorectal polyps using a detachable snare. Gastrointest Endosc. 1996;44:594–597.
Matsuda T, Gotoda T, Saito Y, et al. Our perspective on endoscopic resection for colorectal neoplasms. Gastroenterol Clin Biol. 2010;34:367–370.
Toyonaga T, Man IM, Morita Y, et al. The new resources of treatment for early stage colorectal tumors: EMR with small incision and simplified endoscopic submucosal dissection. Dig Endosc Off J Japan Gastroenterol Endosc Soc. 2009;21:S31–S37.
Seo HJ, Kim YJ, Cho KB, et al. Nodal metastasis after successful endoscopic submucosal dissection for colorectal mucosal cancer. Endoscopy. 2011;43:E374–E375.
Watanabe K, Ogata S, Kawazoe S, et al. Clinical outcomes of EMR for gastric tumors: historical pilot evaluation between endoscopic submucosal dissection and conventional mucosal resection. Gastrointest Endosc. 2006;63:776–782.
Zhou PH, Yao LQ, Qin XY. Endoscopic submucosal dissection for colorectal epithelial neoplasm. Surg Endosc. 2009;23:1546–1551.
Puli SR, Kakugawa Y, Saito Y, et al. Successful complete cure en bloc resection of large nonpedunculated colonic polyps by endoscopic submucosal dissection: a meta-analysis and systematic review. Ann Surg Oncol. 2009;16:2147–2151.
Fujishiro M. Endoscopic submucosal dissection for colorectal neoplasms. World J Gastrointest Endosc. 2009;1:32–38.
Fujishiro M, Yahagi N, Kakushima N et al. Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2007; 5:678–683 (quiz 645).
Tanaka S, Oka S, Kaneko I, et al. Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc. 2007;66:100–107.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yun Jung Kim and Eun Soo Kim contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kim, Y.J., Kim, E.S., Cho, K.B. et al. Comparison of Clinical Outcomes Among Different Endoscopic Resection Methods for Treating Colorectal Neoplasia. Dig Dis Sci 58, 1727–1736 (2013). https://doi.org/10.1007/s10620-013-2560-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-013-2560-x