Abstract
Background
Being one of the core techniques of magnetic surgery, magnetic compression technique (MCT) has been used for digestive tract anastomosis reconstruction in experimental studies. This study verified the feasibility of gastroenteric anastomosis through natural orifice using MCT in rats.
Methods
The parent and daughter magnets were designed and manufactured for oral and anal insertion in 20 Sprague‐Dawley rats. After anesthesia, the parent magnet was inserted into the colon spleen area through the anus, and the daughter magnet was inserted into the stomach through the mouth. Then the two magnets were positioned to attract each other and bind together. The position of the two magnets was monitored using X-ray. The time required for the formation of the anastomosis and expulsion of the magnets were recorded. 2 weeks later, the animal was sacrificed and the anastomotic specimen was obtained which was observed under naked eye and microscope.
Results
The gastroenteric anastomosis was successfully performed via natural orifices in 18 out of 20 rats. The mean time to construct the anastomosis was 3.78 ± 0.88 min. X-ray examination showed that the magnets were in the appropriate position in 17 rats. The magnets were excreted in 9.47 ± 1.62 days after surgery. The gross and microscopic examination of the specimen showed that the anastomoses were patent and the mucosa at the anastomotic was smooth. The mean bursting pressure of the anastomosis was 136.94 ± 6.79 mmHg.
Conclusion
It is feasible to perform gastroenteric anastomosis through natural orifices by MCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastroenteric anastomosis is one of the most important surgical techniques for digestive tract reconstruction for upper gastrointestinal tract diseases. It is routinely performed in oncological, reconstructive and bariatric surgeries [1]. It is an important palliative procedure to improve the quality of life of patients with locally advanced malignant gastroduodenal obstruction in whom radical surgery cannot be performed and endoscopic stenting is not feasible. Moreover, these patients are frail. Hence, the focus of the gastroenterologists has been to develop endoscopic techniques to perform gastrointestinal anastomosis with minimal trauma.
Magnetic surgery is an emerging discipline that utilizes specially designed magnetic medical instruments or equipments to transform the non-contact magnetic force of magnetic objects into a force to perform important functions such as tissue compression, organ anchoring, lumen navigation, gap expansion, controllable tracer and magnetic drive to help in the clinical practice. Magnetic surgery is a broad concept that includes different technologies such as magnetic compression, navigation, anchor, levitation, and many others [2]. Magnetic compression technique (also known as magnamosis) is the most widely used technique of magnetic surgery. At present, magnamosis has been applied for esophageal anastomosis [3,4,5,6], gastrointestinal anastomosis [7,8,9] and intestinal anastomosis [10,11,12,13]. In addition, it can also be used for vascular anastomosis [14,15,16,17,18], rectovaginal fistula repair [19], and tracheoesophageal fistula model preparation [20].
In previous studies, magnamosis was found to be feasible, safe and effective [21]. However, the procedure of magnamosis was mostly performed by laparotomy. In clinical practice, this technique is likely to be more beneficial if performed by natural orifice transluminal endoscopic surgery with minimal trauma in patients with malignant gastrointestinal obstruction. Therefore, we developed the technique of magnamosis to perform gastroenteric anastomosis through natural orifices in the rat model.
Materials and methods
Animals
Twenty Sprague‐Dawley rats (10 males and 10 females) weighing between 200 to 300 g were obtained from the Experimental Animal Center, College of Medicine, Xi’an Jiaotong University. Since the purpose of this experiment was to explore the feasibility of the new technique, all 20 rats were included in the study group and no control group was set. This experiment was approved by the Biomedical Ethics Committee of Xi’an Jiaotong University (No. 2021–1534). The whole experiment process met the ethical requirements of experimental animals.
Magnets
All the magnets used in this study were rectangular in shape. The parent (length 10 mm, width 4 mm, thickness 2 mm) and daughter (length 10 mm, width 3 mm, thickness 2 mm) magnets were designed according to the anatomical characteristics of the esophagus and colon of rats for this experiment (Fig. 1). The magnet was made of N42 sintered Ndfeb and its surface was galvanized. The parent magnet (PM) and daughter magnet (DM) weighed 0.572 g and 0.423 g, respectively. The surface field intensity of the PM and DM was 2590 GS (PM) and 2460 GS (DM), respectively.
Surgical procedures
All rats were adaptively fed for 1 week and were fed a slag-free diet 2 days before surgery. The experimental animals were anesthetized with 10% chloral hydrate (350 mg/kg) by intraperitoneal injection. After induction of anesthesia, the rat was fixed in supine position on the operating table of small animals and placed in the head low position. After lubricating the anus with paraffin oil, the PM was inserted through the anus. Then, PM was pushed into the colon up to the splenic flexure near the body of the stomach with the 8Fr nasogastric tube (Fig. 2A). Then the rat was placed in reverse Trendelenburg position at 60–70°. Titanium alloy tissue tweezer was used to place the DM into the esophagus and 8Fr nasogastric tube was used to push it into the stomach (Fig. 2B). The position of PM and DM was adjusted under fluoroscopy until they engaged automatically (Fig. 2C).
Schematic diagram of the surgical procedure. A Insertion of the parent magnet through the anus in to the colon. B Insertion of the daughter magnet through the mouth in to the stomach. C The daughter and parent magnets get attracted together. D After the anastomosis was formed, the magnets were expelled into the colon
Postoperative care
After the operation, the rats were raised in a single cage. Subsequently, the rats were fed normally. The animals underwent an X-ray examination every day to observe the position of the magnets. Due to the compression between the two magnets, the gastro-colonic anastomosis would be formed. Once the anastomosis is formed, the magnets fell off and get discharged naturally through the anus (Fig. 2D). The time when the magnets were expelled from the body was recorded.
Calculation of the anastomosis time
Anastomosis time was defined as the time from the initial insertion of magnets to the attraction of the two magnets in vivo.
Bursting pressure
2 weeks after surgery, the rats were euthanized with excessive chloral hydrate. The gastroenteric anastomosis specimens were resected, including the stomach, 8 cm of the colonic segment, a small section of esophagus and duodenum. The open ends of esophagus, duodenum and the proximal colon were closed with silk thread, and a catheter was introduced through the open end of the distal colon which was then ligated with a single silk suture. The entire anastomotic specimen was immersed in 0.9% normal saline and the pressure in the lumen was slowly increased. The sphygmomanometer was used to measure the bursting pressure of the anastomosis. The intraluminal pressure at which the first bubble emerged from the anastomosis was recorded as the bursting pressure of the anastomosis.
Histological analyses
Anastomotic sections of sufficient length were cut and soaked overnight in 10% buffered formalin. After fixation, the anastomosis bearing segment was embedded in paraffin and 4-µm thick sections were cut at the anastomotic site. Sections were stained with hematoxylin and eosin (H&E) or Masson’s trichrome stain and examined under a bright field microscope.
Statistical analysis
The SPSS version 18.0 was used for data analysis. Quantitative data are expressed as mean ± standard deviation.
Results
Survival rate and postoperative complications
The survival rate was 90% (18/20). One rat died due to anesthetic overdose, and the other died of asphyxia after a failed attempt to place the DM through the esophagus. In another rat, the side of the PM in the colon got attracted to the bottom of the DM in the stomach, forming a smaller anastomosis. The remaining 17 rats had good anastomosis and no complications.
Procedural parameters
The gastroenteric anastomosis was successfully performed in 18 rats. The mean anastomosis time in 18 rats was 3.78 ± 0.88 min. X-ray examination of 17 rats showed that the magnets were in the appropriate position (Fig. 3A–D). In one rat, the side of the PM in the colon got attracted to the bottom of the DM in the stomach (Fig. 4). The patency of the anastomosis was confirmed by gastrointestinal radiography after the magnets fell off (Fig. 3E, F).
X-ray examination. A The parent magnet (white arrow) was inserted into the colon through the anus. B The daughter magnet (black arrow) was inserted orally into the stomach. C Anteroposterior radiograph of two magnets attached together (red arrow). D Lateral radiograph of two magnets attached together. E Anteroposterior gastrointestinal radiography showed anastomosis was unobstructed. F Lateral gastrointestinal radiography (Color figure online)
Timing of expulsion of the magnets
The mean time for the magnets to expel from the anus was 9.47 ± 1.62 days (range 6–12 days).
Bursting pressure
The mean blast pressure was 136.94 ± 6.79 mmHg at 2 weeks postoperatively (Fig. 5A).
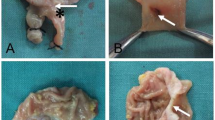
The gross appearance of anastomoses. A Measurement of the bursting pressure at the anastomotic site. B The whole specimen of the anastomosis and a pair of expelled magnets. C The appearance of the anastomosis from the colonic side. D The appearance of the anastomosis from the gastric side. E The anastomosis was dissected along the longitudinal axis. (“⋆” is the colon, “*” is the esophagus, “▲” is the stomach, “x” is the duodenum)
Gross and histological appearance of anastomosis
The gross specimen obtained 2 weeks after the operation showed that the anastomoses were patent and the mucosa at the anastomotic site was smooth (Fig. 5B–E). HE and Masson’s staining showed that the mucosa at the anastomosis healed with good integrity (Fig. 6).
Discussion
The gastroenteric anastomosis can be achieved either by hand-sewn sutures or by the mechanical application of metal staplers [22]. Magnamosis is a third technique to perform a gastroenteric anastomosis. Due to the characteristic of “power from a distance” of the magnets, no foreign body can penetrate the tissue to be anastomosed during the digestive tract reconstruction by magnamosis. The “sandwich” structure of “magnet-tissue-magnet” causes the magnetic force to compress the tissues between the magnets at the anastomotic site. Due to the continuous compression of magnetic force, the pressed tissues between the magnets were subjected to ischemia, necrosis and shedding, while the adjacent tissues underwent the pathological changes of adhesion, repair and healing. After the anastomosis was formed, the PM along with the DM migrated into the distal colon and was expelled spontaneously through the anus. For magnamosis, the anastomotic stoma is not established after the attraction of the parent and daughter magnets, and the anastomotic stoma can be established only after the magnets fall off, which is the inherent characteristic of the magnamosis mode. Therefore, we believe that gastrointestinal magnamosis is suitable for situations where there is no immediate need to establish anastomotic access, such as gastrointestinal bypass surgery.
Magnamosis provides an excellent technique for gastrointestinal anastomosis using endoscopy. Due to the lack of suitable endoscopic system for rats, we had to put the magnet into the stomach by direct push method through the mouth. The parent magnets were also pushed directly through the anus as far as possible in the colon. But, due to the shape of the colon and absence of appropriate endoscope for rats, the magnets could not be placed in the small intestine to perform gastrojejunal or gastroileal anastomosis which is the required anastomosis in clinical practice. However, in clinical practice, the magnets can be placed at the desired place more conveniently with the help of gastroscope, enteroscope or colonoscope. In this experiment, we confirmed the feasibility of a novel method for gastrocolonic anastomosis using magnamosis. On the basis of this study, future studies on large animals such as pigs and beagles can be conducted using endoscopic systems such as gastroscope, colonoscope and enteroscope and confirm the feasibility of magnamosis in constructing gastroenteric anastomosis.
In the previous animal experiments of magnetic anastomosis, the magnets were ring-shaped. But in this experiment, cuboid magnets were used. In order to facilitate the insertion or immediate opening of anastomosis, the magnets used for end-to-end anastomosis of gastrointestinal tract, biliary tract and esophagus are generally cylindrical or ring-shaped [23,24,25,26,27]. In this study, there was no need to establish an immediate intraoperative anastomosis. At the same time, considering the maneuverability of the magnet, the cross-sectional area of magnet should be as small as possible but sufficient enough to form a wide anastomosis. Based on the above factors, the cuboid magnet was designed. It should be noted that after the placement of the PM in the colon, the distance between the two magnets should be always paid attention to in order to avoid the non-anastomotic surface of the two magnets attracting each other when the DM was inserted in the stomach. Otherwise, the anastomosis would be too small or the magnets cannot be discharged. To ensure that the magnets are attracted in the right way, the magnets in the stomach or colon are attracted by a large anchor magnet outside the abdominal wall to adjust their relative positions. The slight movement of the external magnet can attract the inner magnets to move through the gastrointestinal, making the daughter magnet and the parent magnet attractive to each other.
This experiment proved the feasibility of gastrocolonic magnamosis without the need for laparotomy. This novel technique can fasten the recovery and reduce the incidence of abdominal complications. In addition, there was no invasive damage to the gastrointestinal after this method, so normal food and water can be taken after anesthesia. Postoperative gross and histology examination of the resected specimen showed that the gastroenteric anastomosis was well formed, unobstructed with smooth mucosa.
Conclusion
This study demonstrated that it is feasible to perform gastrocolonic anastomosis through natural orifices without laparotomy. Gastrointestinal anastomoses through endoscopic systems need to be performed in large animals to confirm the feasibility of this technique and further optimize magnet design before studying in humans. The significance of this paper lies in providing a new idea and method for the endoscopy of gastrointestinal noninvasive anastomosis.
References
Kopelman D, Hatoum OA, Kimmel B, Monassevitch L, Nir Y, Lelcuk S, Rabau M, Szold A (2007) Compression gastrointestinal anastomosis. Expert Rev Med Devices 4(6):821–828
Bai J, Huo X, Ma J, Lv Y, Yan X (2018) Magnetic compression technique for colonic anastomosis in rats. J Surg Res 231:24–29
Muensterer OJ, Sterlin A, Oetzmann von Sochaczewski C, Lindner A, Heimann A, Balus A, Dickmann J, Nuber M, Patel VH, Manfredi MA, Jennings RW, Smithers CJ, Fauza DO, Harrison MR (2020) An experimental study on magnetic esophageal compression anastomosis in piglets. J Pediatr Surg 55(3):425–432
Bruns NE, Glenn IC, Craner DR, Schomisch SJ, Harrison MR, Ponsky TA (2019) Magnetic compression anastomosis (magnamosis) in a porcine esophagus: proof of concept for potential application in esophageal atresia. J Pediatr Surg 54(3):429–433
Parlak E, Eminler AT, Koksal AS, Toka B, Uslan MI, Sokmensuer C, Guven M (2019) A new method for lumen restoration in a patient with aphagia: oro-oesophageal through-the-scope magnetic compression anastomosis. Clin Otolaryngol 44(6):1214–1217
Sterlin A, Evans L, Mahler S, Lindner A, Dickmann J, Heimann A, Sahlabadi M, Aribindi V, Harrison MR, Muensterer OJ (2021) An experimental study on long term outcomes after magnetic esophageal compression anastomosis in piglets. J Pediatr Surg S0022–3468(21):00646–00651
Ryou M, Cantillon-Murphy P, Azagury D, Shaikh SN, Ha G, Greenwalt I, Ryan MB, Lang JH, Thompson CC (2011) Smart Self-Assembling MagnetS for ENdoscopy (SAMSEN) for transoral endoscopic creation of immediate gastrojejunostomy (with video). Gastrointest Endosc 73(2):353–359
Watanabe R, Barberio M, Kanaji S, Lapergola A, Ashoka AH, Andreiuk B, Guerriero L, Pizzicannella M, Seeliger B, Saida Y, Kaneko H, Worreth M, Saadi A, Marescaux J, Klymchenko AS, Diana M (2020) Hybrid fluorescent magnetic gastrojejunostomy: an experimental feasibility study in the porcine model and human cadaver. Surg Endosc 34(3):1393–1400
An Y, Zhang Y, Liu H, Ma S, Fu S, Lv Y, Yan X (2018) Gastrojejunal anastomosis in rats using the magnetic compression technique. Sci Rep 8(1):11620
Schlottmann F, Ryou M, Lautz D, Thompson CC, Buxhoeveden R (2021) Sutureless duodeno-ileal anastomosis with self-assembling magnets: safety and feasibility of a novel metabolic procedure. Obes Surg 31(9):4195–4202
Ryou M, Aihara H, Thompson CC (2016) Minimally invasive entero-enteral dual-path bypass using self-assembling magnets. Surg Endosc 30(10):4533–4538
Ma F, Ma J, Ma S, Fu S, Zhang Y, Liu H, Lv Y, Wu R, Yan X (2019) A novel magnetic compression technique for small intestinal end-to-side anastomosis in rats. J Pediatr Surg 54(4):744–749
Chen H, Ma T, Wang Y, Zhu HY, Feng Z, Wu RQ, Lv Y, Dong DH (2020) Fedora-type magnetic compression anastomosis device for intestinal anastomosis. World J Gastroenterol 26(42):6614–6625
Yan X, Fan C, Ma J, Li J, Dong D, Wang H, Ma F, Zheng X, Lv Y (2013) Portacaval shunt established in six dogs using magnetic compression technique. PLoS ONE 8(9):e76873
Yan XP, Liu WY, Ma J, Li JP, Lv Y (2015) Extrahepatic portacaval shunt via a magnetic compression technique: a cadaveric feasibility study. World J Gastroenterol 21(26):8073–8080
Wang HH, Ma J, Wang SP, Ma F, Lu JW, Xu XH, Lv Y, Yan XP (2019) Magnetic anastomosis rings to create portacaval shunt in a canine model of portal hypertension. J Gastrointest Surg 23(11):2184–2192
Wang SP, Yan XP, Xue F, Dong DH, Zhang XF, Ma F, Wang HH, Lv Y (2015) Fast magnetic reconstruction of the portal vein with allogeneic blood vessels in canines. Hepatobiliary Pancreat Dis Int 14(3):293–299
Falk V, Walther T, Stein H, Jacobs S, Walther C, Rastan A, Wimmer-Greinecker G, Mohr FW (2003) Facilitated endoscopic beating heart coronary artery bypass grafting using a magnetic coupling device. J Thorac Cardiovasc Surg 126(5):1575–1579
She ZF, Yan XP, Ma F, Wang HH, Yang H, Shi AH, Wang L, Qi X, Xiao B, Zou YL, Lv Y (2017) Treatment of rectovaginal fistula by magnetic compression. Int Urogynecol J 28(2):241–247
Gao Y, Wu RQ, Lv Y, Yan XP (2019) Novel magnetic compression technique for establishment of a canine model of tracheoesophageal fistula. World J Gastroenterol 25(30):4213–4221
Ye D, Zhang MM, Shi AH, Chen WW, Gao HM, Zhang JH, Shen WC, Lyu Y, Yan XP (2021) Construction of esophagogastric anastomosis in rabbits with magnetic compression technique. J Gastrointest Surg 25(12):3033–3039
Li NN, Zhao WT, Wu XT (2016) Can a nickel-titanium memory-shape device serve as a substitute for the stapler in gastrointestinal anastomosis? A systematic review and meta-analysis. J Surg Res 201(1):82–93
Fan C, Yan XP, Liu SQ, Wang CB, Li JH, Yu L, Wu Z, Lv Y (2012) Roux-en-Y choledochojejunostomy using novel magnetic compressive anastomats in canine model of obstructive jaundice. Hepatobiliary Pancreat Dis Int 11(1):81–88
Zhang H, Tan K, Fan C, Du J, Li J, Yang T, Lv Y, Du X (2017) Magnetic compression anastomosis for enteroenterostomy under peritonitis conditions in dogs. J Surg Res 208:60–67
Lu G, Li J, Ren M, Ma F, Sun X, Lv Y, He S (2021) Endoscopy-assisted magnetic compression anastomosis for rectal anastomotic atresia. Endoscopy 53(12):E437–E439
Liu XM, Li Y, Zhang HK, Ma F, Wang B, Wu R, Zhang XF, Lv Y (2019) Laparoscopic magnetic compression biliojejunostomy: a preliminary clinical study. J Surg Res 236:60–67
Liu XM, Li Y, Xiang JX, Ma F, Lu Q, Guo YG, Yan XP, Wang B, Zhang XF, Lv Y (2019) Magnetic compression anastomosis for biliojejunostomy and pancreaticojejunostomy in Whipple’s procedure: an initial clinical study. J Gastroenterol Hepatol 34(3):589–594
Funding
This work was supported by the Innovation Capability Support Plan of Shaanxi Province (Grant No. 2020KJXX-022) and the Key Research & Development Program-Social Development of Shaanxi Province (Grant No. 2021SF-163).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
During the conduct of this work, Miaomiao Zhang, Yixing Li, Min Pan, Shuqin Xu, Jingci Gai, Hanzhi Zhang, Yingfeng An, Aihua Shi, Yi Lyu and Xiaopeng Yan have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, M., Li, Y., Pan, M. et al. Creation of gastroenteric anastomosis through natural orifice in rats by magnetic compression technique. Surg Endosc 36, 8170–8177 (2022). https://doi.org/10.1007/s00464-022-09257-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09257-z