Abstract
Background
Endoluminal functional lumen imaging probe (EndoFLIP) provides an objective measure of the distensibility index (DI) during different parts of hiatal hernia repair. However, the absolute DI measure above a cut-off after creating a barrier alone has not shown a relationship to dysphagia after surgery. We wanted to determine if the change in DI with volume change is associated with dysphagia.
Methods
We included patients who had hiatal hernia repair with EndoFLIP values, including two values taken at the end of the surgical case with different volumes of fluid in the balloon (30 mL and 40 mL). We compared the absolute and change in DI during hiatal hernia repair and performed an analysis to determine if there was a correlation with short-term clinical outcomes.
Results
A total of 103 patients met the inclusion and exclusion criteria. Most of the patients underwent Toupet fundoplication (n = 56, 54%), followed by magnetic sphincter augmentation (LINX, n = 28, 27%) and Nissen fundoplication (n = 19, 18%). There was a significant reduction in the DI from the initial DI taken after mobilization of the hiatus (3 mm2/mmHg) and after the creation of the barrier (1.4 mm2/mmHg, p < 0.001). A minority of patients had a decrease or no change in the DI with an increase in balloon volume increased from 30 to 40 mL (n = 37, 36%). Overall, after 1 month, there was a significant decrease in the GERD-HRQL score from 23 to 4 (p < 0.001) and bloat score from 3 to 2 (p = 0.003) with a non-significant decrease in the dysphagia score from 1 to 0 (p = 0.11). Patients who had a decreased or unchanged DI with an increase in the balloon volume from 30 to 40 mL had a significant decrease in their dysphagia score by 2 points (p = 0.04).
Conclusion
The decreased or unchanged DI with an increase in the balloon volume on EndoFLIP is associated with a significant reduction in dysphagia after surgery. The decrease in DI denotes the esophagus’s ability to create higher pressure relative to the change in the cross-sectional area with a larger bolus across the gastroesophageal junction. This measure may be a new marker that can predict short-term outcomes in patients undergoing hiatal hernia repair.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hiatal hernia is a common condition that can cause significant symptoms, such as gastroesophageal reflux disease, dysphagia, bloating, early satiety, and extraesophageal symptoms such as cough. The goal of the surgical repair of a hiatal hernia is to restore the normal anatomy and create a barrier between the esophagus and stomach, leading to the resolution of the patient’s symptoms. This can be performed using different surgical techniques to resolve the patient’s symptoms [1, 2]. However, creating a barrier may lead to the resolution of symptoms from reflux and symptoms related to having a stomach in the chest, but it may be replaced with symptoms related to having a barrier, such as dysphagia and bloating. The incidence of dysphagia and bloating after Nissen fundoplication has been well documented in the literature as high as 30–50% [3]. Thus, with the presence of variation of surgical techniques with significant side effects after surgery, multiple groups have initiated the use of endoluminal functional lumen imaging probe (EndoFLIP) to obtain objective data during the operation [3,4,5,6,7,8].
EndoFLIP is a measuring device that provides objective quantitative data about the minimal diameter, cross-sectional area, and distensibility index when placed across the gastroesophageal junction (GEJ) and filled to different volumes [6]. The EndoFLIP uses electrical resistance or impedance to find the cross-sectional area [9, 10]. The distensibility index (DI) is the cross-sectional area of the balloon divided by the pressure generated when the balloon is filled with different volumes. Ilczyszyn et al. examined the relationship between the DI value and outcome and found that patients with a DI below or at 0.5 mm2/mmHg after fundoplication needed a revision of the fundoplication [11]. In our practice, we have shown that we can obtain objective data during the operation and then modify the operation to obtain a final DI > 0.5 mm2/mmHg at the end of the case [3, 8]. This has led to a final DI of 1.6 mm2/mmHg for a cohort of patients who had Nissen, Toupet, and MSA and led to patients avoiding significant dysphagia at the end of the case [8]. However, the key data point that was used in our previous study was the final DI after the creation of the barrier. The relative final DI was not associated with a short-term dysphagia score. The possible reason for the lack of an association is that dysphagia is a function of both tightness of the barrier and the ability of the esophagus to push food through a barrier. We postulated that we might be able to measure the ability of the esophagus to push food through a barrier using the EndoFLIP based on the amount of pressure generated by the change in the volume in the balloon. Since DI is a measure of the area over pressure, if the change in pressure is greater than the change in the area, the DI will decrease. Thus, we postulated that a decrease in the DI with an increase in volume is associated with a decrease in dysphagia since the esophagus has the ability to push through the barrier.
Materials and methods
The institutional review board at Houston Methodist Hospital Research Institute approved this study. We analyzed an EndoFLIP database for patients who underwent primary minimally invasive elective gastroesophageal reflux surgery with or without hiatal hernia repair at our institute between 2018 and 2020. Typically, patients with a large type III hiatal hernia or poor motility underwent Toupet fundoplication, while patients with good motility underwent either LINX or Nissen fundoplication procedures.
We obtained patient demographics, type of hiatal hernia, manometry results, 24-h impedance, or Bravo pH testing results. We also obtained EndoFLIP measurements of the minimal diameter (Dmin), cross-sectional area (CSA), and distensibility index (DI) after mobilization of the hiatus, crus closure, barrier creation (Nissen fundoplication, Toupet fundoplication, or magnetic sphincter augmentation (MSA)), and with the patient placed in a supine position with 30 mL in the balloon (supine 30) and 40 mL in the balloon (supine 40) after removal of insufflation of the abdomen and removal of the liver retractor. We included patients for this study if they had complete EndoFLIP measurements using an 8 cm catheter (EF-325 N, Medtronic, Dublin, Ireland) at these time points during the operation. In addition, we included patients who completed the gastroesophageal reflux disease—health-related quality of life score (GERD-HRQL) before surgery and one month after surgery. The GERD-HRQL questionnaire comprises 10 categories, each measured on a scale of 0–5. We included the specific scores for the bloating and dysphagia categories (0–5) in our analysis.
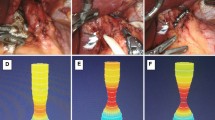
All operations were performed in a minimally invasive fashion with the Da Vinci Xi Robot System (Intuitive Surgical, Sunnyvale, CA). During robot-assisted surgery, patients were placed in a reverse Trendelenburg position, and pneumoperitoneum (15 mmHg) was established with a liver retractor when placed to expose the gastroesophageal junction. We then performed mobilization of the esophagus by dissecting and removing the hiatal hernia sac that allowed about 2–3 cm of the esophagus in the abdomen.
At this point in the surgery, we obtained EndoFLIP measurements. The EndoFLIP catheter was zeroed to atmospheric pressure and then advanced through the mouth into the stomach. The catheter was filled to 20 mL and slowly withdrawn until an hourglass was seen on the monitor. We then filled the balloon to 30 mL and adequate time was given to ensure the readings were stabilized (minimum of 30 s and up to 10 min) before recording the Dmin, DI, and CSA. (Fig. 1). We then kept the EndoFLIP inflated with 30 mL of fluid to assist with the closure of the crus. The crus was closed until there was no opening between the esophagus and crus. We then deflated the EndoFLIP to 20 mL volume and then reinflated it to 30 mL volume to take the measurement after crus closure (Fig. 1). The EndoFLIP was deflated to create the Toupet fundoplication and it was intermittently inflated for the creation of the Nissen fundoplication. The EndoFLIP was pulled back above the GEJ and placed around the esophagus for placement of the MSA according to the manufacturer’s recommendations (Johnson & Johnson, New Brunswick, NJ, USA). After creating the barrier, the EndoFLIP was placed at the GEJ and inflated to 30 mL to measure the values after the creation of the barrier (Fig. 1). Next, the patient was taken out of reverse Trendelenburg, the liver retraction was removed, and the insufflation of the abdomen was removed. We then obtained EndoFLIP measurements with a balloon filled to 30 mL (supine 30) and a balloon filled to 40 mL (supine 40).
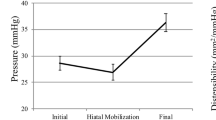
Distensibility index through different points of the operation. Median distensibility index after mobilization of the esophagus (Initial), after the closure of the crus (Crus), after the creation of the Nissen, Toupet, or LINX (Barrier), and after removal of the liver retractor and insufflation with the patient in supine position with 30 mL in the EndoFLIP balloon (Supine 30) and 40 mL in the EndoFLIP balloon (Supine 40)
Subsequently, we analyzed the relationship between EndoFLIP values after creating the barrier and after the patient is supine with the removal of insufflation with 30 mL in the balloon. We also analyzed the relationship between the absolute EndoFLIP values with patient supine measured with 30 mL and 40 mL volumes and the change in the DI with an increase in volume to short-term clinical outcomes. The change in DI was grouped into patients who had the same or decrease in DI or an increase in DI after fill volume from 30 to 40 mL. We also evaluated patients with a GERD-HRQL score > 10 at one month, dysphagia score > 3, or bloat score > 3 at one month after surgery. We then determine if any factors correlated to these scores.
Patient characteristics and EndoFLIP values were reported as frequencies and proportions for categorical variables and as median and interquartile range (IQR) for continuous variables. Differences between patients having decreased or unchanged DI and patients having increased DI from a flat 30 to a flat 40 were compared using the Chi-square or Fisher's exact test for categorical variables and the Kruskal–Wallis test for the continuous variables. Univariable generalized linear models (GLM) were used to determine the characteristics associated with GERD-HRQL score at one month > 10, dysphagia score at one month > 3, or bloating score at one month > 3. Unadjusted risk ratios and 95% confidence intervals were reported. Given the small number of events and sample size, multivariable GLM was not conducted. Pearson’s correlation test was used to evaluate the correlation of the EndoFLIP values among different time points. Box plots and bar charts were used to present the GERD-HRQL score, dysphagia score, bloating score, patient satisfaction, and heartburn medication use. Differences of these parameters at one month and before the surgery were compared using the median sign test for the equality of matched pairs. In some box plots, the extreme values (outside the range of 1st quartile minus 1.5 IQR and 3rd quartile plus 1.5 IQR) were not presented to improve the readability of the box plots. The exclusion of the outside values did not affect the comparison statistics. The frequency and proportion of patients who underwent an additional surgery or had symptom improvement were also reported. All the analyses were performed on Stata version 16.1 (StataCorp LLC, College Station, TX, USA). A p value of < 0.05 was considered statistically significant.
Results
There were 103 patients who met the inclusion criteria. The median age of the group was 64 (IQR 55, 71) years old. Patient were predominantly white (n = 95, 92.2%) and female (n = 78, 75%) with a median BMI of 29.6 (IQR 26.6, 33.6). A Type III hiatal hernia was the most common type of hernia (n = 55, 53%), followed by Type I hiatal hernia (n = 42, 41%). In patients who underwent a Bravo pH probe or 24-h impedance study, the median DeMeester score was 22.6 (IQR 10.8, 40.8). In patients who underwent manometry, the median normal swallows were 90% (IRQ 50%, 100%). The median initial GERD-HRQL score was 23 (IQR 13, 29), with a dysphagia score of 1 (IQR 0, 3) and a bloat score of 3 (IQR 1, 4). The most common operation was hiatal hernia repair (n = 98, 95.15%) with Toupet fundoplication (n = 56, 54%) followed by magnetic sphincter augmentation (MSA, n = 28, 27%). There were ten patients (9.7%) who had redo surgeries (Table 1).
The cohort of the patients had an initial median DI of 3.0 mm2/mm Hg (IQR 1.9, 4.0), which decreased to a median DI of 1.8 mm2/mm Hg after the closure of the crus (IQR 1.4, 2.5, p < 0.001). The median DI further decreased after barrier creation to 1.4 mm2/mm Hg (IQR 1.1, 1.8, p < 0.001). However, there were no significant differences between the DI after barrier formation and when the patient was supine without insufflation and liver retractor at 30 mL filled in the balloon of 1.4 mm2/mm Hg (IQR 1.1, 2.0, p = 0.17). When the balloon was filled to 40 mL with the patient in a supine position, the median DI increased to 1.7 mm2/mm Hg (IQR 1.3, 2.2, p < 0.001, Fig. 1).
There was a significant decrease in the GERD-HRQL score after surgery from a median of 23 to 4 (p < 0.001, Fig. 2A). Analysis of the bloat score showed a significant decrease from a median of 3 to 2 (p = 0.003, Fig. 2B). There was a decrease in the dysphagia score from 1 to 0 after surgery, but this was not statistically significant (p = 0.11, Fig. 2C). In this cohort of patients, 12 patients (12%) had a GERD-HRQL score > 10 at one month after surgery. There were four patients (4%) who had dysphagia scores > 3 and 16 patients (15%) who had bloat scores > 3. Univariate analysis showed that none of the patient characteristics, procedural characteristics, or the EndoFLIP values were associated with a GERD-HRQL score > 10 (Supplemental Table 1). However, univariate analysis showed that a dysphagia score > 3 at one month was associated with greater change in DI from supine 30 to supine 40 (HR 4.56 95% CI 1.02, 20.31, p = 0.047, Table 2, Supplemental Table 2). Finally, univariate analysis showed that a bloat score > 3 at one month was not associated with patient characteristics or EndoFLIP values, but it was protected by undergoing a LINX procedure (HR 0.11, 95%CI 0.01, 0.87, p = 0.04, Supplemental Table 3).
We further analyzed the change in the DI with the patient supine from 30 to 40 mL and its relationship with dysphagia. A minority of patients had a decrease or no change in DI with an increase in balloon volume from 30 to 40 mL (n = 37, 36%). There was no significant difference in the median DI after mobilization of the esophagus (initial, p = 0.1), after the closure of crus (crus closure, p = 0.84), creation of barrier (barrier creation, p = 0.95), and patient supine with 30 mL of volume (supine 30, p = 0.36) between patients who had a decrease or no change in the DI or increased in DI from supine 30 to supine 40 (Table 3). However, patients who had an increase in DI had a significantly higher median DI at supine 40 (1.9 mm2/mmHg IQR 1.4, 2.3) compared to patients who had a decrease or no change in DI (1.3 mm2/mmHg IQR 1, 1.8, p < 0.001). We discovered that the median change in dysphagia score before surgery to after surgery between patients with decrease or no change in DI (− 2, IQR − 2,0) was significantly lower compared to a patient who had an increase in DI (0, IQR − 1, 0, p = 0.04, Fig. 3, Table 4). However, there was no significant difference in absolute and change in GERD-HRQL score and bloat score (Table 4).
Discussion
The utilization of the EndoFLIP during creating a barrier (Nissen, Toupet, or LINX) with or without hiatal hernia repair provided objective data during the operation that provided overall excellent short-term clinical outcomes. Our study showed an overall decrease in the distensibility index as the crus was closed around the esophagus and the barrier was created around the esophagus. This is likely the impact of patients who underwent LINX and Nissen fundoplication compared to patients who underwent Toupet fundoplication. Our previous study showed that a subset analysis of patients who underwent LINX had a significant decrease in DI, while patients who had Toupet fundoplication did not see a significant decrease in DI compared to after crus closure [8]. This finding is similar to Su et al. recent data that showed no significant difference or increase in the post-fundoplication DI compared to the closure of the crus with 69.1% of the cohort undergoing Toupet fundoplication [12]. Our current study shows that the final DI measurement after creating the barrier is significantly decreased compared to the initial DI measurement. This outcome is similar to the finding described by other groups that showed a significant decrease in DI after fundoplication compared to after mobilization of the hiatus [7, 12, 13] or pre-insufflation [14].
Overall, patients had resolution of their symptoms without significant bloating, with a very rare group of patients having high bloat scores. There was no correlation between bloat score to either the DI value at 30 mL or 40 mL of volume in the EndoFLIP or with the dynamic DI value at the change from 30 to 40 mL. The reason for the lack of correlation is that a high bloat score is related to the ability of the stomach to process the gas and the ability of the barrier to allow the gas to escape. Since the EndoFLIP does not measure the ability of the stomach to process the gas, it is likely the reason for the lack of correlation. However, our study did confirm the findings of other studies [5] that show that LINX was associated with less bloating at short-term follow-up. A systematic review by Schizas et al. of 35 studies with 2511 MSA patients found that postoperative proton pump inhibitor cessation rates reached 100% with less bloating symptoms and a better ability to belch or vomit in comparison to fundoplication [12].
While we found no significant difference between the artificial environment of the surgery (reverse Trendelenburg, insufflation, and liver retractor) to the patient in the natural position (supine, no insufflation, and no liver retractor), Su et al. found a difference between having the artificial environment of the operating and patient in a natural state [12]. The difference seen may be due to how the measurement was made or how the data were analyzed. In our study, we left the EndoFLIP balloon inflated continuously and used the balloon inflated to close the crus, while Su et al. obtained measurement intermittently at 30 s after insufflation of the balloon [6]. This may be the reason for the difference in our findings with those of the Nathanson et al. study [15]. Nathanson et al. found an impact of EndoFLIP values with pneumoperitoneum; however, they measured different points with intermittent insufflation of the EndoFLIP [15]. In addition, Su et al. used data available, which meant that they compared two groups with different patients [12]. For example, in their analysis of reverse Trendelenburg, they had n = 65 without reverse Trendelenburg compared to n = 95 with reverse Trendelenburg, resulting in comparing different groups of patients. In contrast, our analysis had the same number of patients in each group. Our study discovered that the positioning of the patient, the presence of insufflation of the abdomen, and liver retraction did not impact the distensibility index. There was no significant difference when the DI was measured after creating the barrier to when the DI was measured at the end of the case, when the patient was supine with a liver retractor, and insufflation was removed from the abdomen. This finding implies that the values derived after creating the barrier can be used as a surrogate for the value obtained in a setting without the artificial environment of the operating room. Furthermore, we confirmed that staying above the absolute value of DI > 0.5 mm2/mmHg led to very low rates of significant dysphagia. However, both DIs measured at the end of the case with the patient in the supine position with 30 mL or 40 mL in the balloon did not significantly correlate with short-term outcomes. Thus, once again, the absolute value of DI with either 30 mL or 40 mL was not associated with dysphagia. Although there is no significant difference between the EndoFLIP values in artificial and natural positions, it has been helpful to obtain the natural position at two different volumes of fluid. This value can be beneficial in the future evaluation of the patient if there is any development of recurrence of symptoms or significant dysphagia. Those patients undergo endoscopy and EndoFLIP measurements in a natural position, and the values can be compared to the values obtained at the end of the index case without the artificial environment of the operating room.
Finally, we did discover a new marker in our analysis that was associated with the improvement of dysphagia. We discovered that when the DI decreased or did not change with the increase in the full volume from 30 to 40 mL, there was an associated decrease in dysphagia after surgery. Since DI is a measurement of cross-sectional area (CSA) over the pressure, for the DI not to change or decrease, the change in pressure has to increase more or change proportional to the change in the CSA. The likely factor that increases the pressure is the ability of the lower esophagus to generate the pressure against the volume. Our study also demonstrated that patients who had decreased or no change in the DI when the balloon was inflated from 30 to 40 mL had a statistically significant decrease in their dysphagia score. The decrease or no change in DI may be a marker of the ability of the lower esophagus above the barrier to create enough pressure to push the bolus through a barrier. Moreover, those patients who have a greater change in the DI with the change in the fill volume denote the inability for the patient to generate enough pressure through the barrier, thus leading to an increase in dysphagia. This is the first study that shows the correlation of the change in DI with fill volume having an impact on dysphagia.
The limitation of the study is that the study is a retrospective analysis of data. The EndoFLIP values were collected prospectively in a database after each case to minimize bias from a retrospective study. We also limited this study to patients who had recorded EndoFLIP values when they were supine with 30 mL and 40 mL volumes in the catheter. This limited the total number of patients in this study, but it provides a complete picture of the EndoFLIP values and their relationship to short-term outcomes. Finally, the study’s main limitation is that our research evaluated patient’s EndoFLIP values to short-term outcomes. We decided to focus on the short-term outcome since significant dysphagia usually improves over time [16]. Hypothetically, at a short-term interval, the patient should have a poorer dysphagia score, which provides a clinical data point to understand dysphagia symptom to EndoFLIP values. In addition, the long-term outcome may also relate to other factors, such as recurrence of hiatal hernia or breakdown of the wrap, which may not relate to objective measurements of the closed crus with a barrier around the esophagus at the time of surgery. However, we certainly agree that long-term outcomes are important, and we are currently collecting long-term data in this group of patients for future studies.
In conclusion, we were able to show that the artificial environment of the surgery does not lead to different EndoFLIP values, the static EndoFLIP values did not correlate with the short-term clinical outcomes, but the dynamic EndoFLIP value of the change in DI with a volume change was associated with dysphagia score. The combined information about the barrier and the function of the lower esophagus proximal to the barrier derived from EndoFLIP values are associated with dysphagia. The EndoFLIP can help avoid significant dysphagia after surgery, and it may provide predictive information about short-term outcomes after barrier formation.
References
Jarral OA, Athanasiou T, Hanna GB, Zacharakis E (2012) Is an intra-oesophageal bougie of use during Nissen fundoplication? Interact Cardiovasc Thorac Surg 14:828–833
Huttl TP, Hohle M, Wichmann MW, Jauch KW, Meyer G (2005) Techniques and results of laparoscopic antireflux surgery in Germany. Surg Endosc 19:1579–1587
Kim MP, Meisenbach LM, Chan EY (2018) Tailored fundoplication with endoluminal functional lumen imaging probe allows for successful minimally invasive hiatal hernia repair. Surg Laparosc Endosc Percutan Tech 28:178–182
Tucker E, Sweis R, Anggiansah A, Wong T, Telakis E, Knowles K, Wright J, Fox M (2013) Measurement of esophago-gastric junction cross-sectional area and distensibility by an endolumenal functional lumen imaging probe for the diagnosis of gastro-esophageal reflux disease. Neurogastroenterol Motil 25:904–910
Turner B, Helm M, Hetzel E, Gould JC (2020) Is that “floppy” fundoplication tight enough? Surg Endosc 34:1823–1828
Su B, Dunst C, Gould J, Jobe B, Severson P, Newhams K, Sachs A, Ujiki M (2020) Experience-based expert consensus on the intra-operative usage of the Endoflip impedance planimetry system. Surg Endosc 35:2731–2742
Su B, Callahan ZM, Kuchta K, Linn JG, Haggerty SP, Denham W, Ujiki MB (2020) Use of impedance planimetry (endoflip) in foregut surgery practice: experience of more than 400 cases. J Am Coll Surg 231:160–171
Nwokedi U, Nguyen DT, Meisenbach LM, Chihara R, Chan EY, Graviss EA, Kim MP (2020) Short-term outcome of routine use of EndoFLIP during hiatal hernia repair. Surg Endosc 35(7):3840–3849
Carlson DA (2016) Functional lumen imaging probe: the FLIP side of esophageal disease. Curr Opin Gastroenterol 32:310–318
Lottrup C, Gregersen H, Liao D, Fynne L, Frokjaer JB, Krogh K, Regan J, Kunwald P, McMahon BP (2015) Functional lumen imaging of the gastrointestinal tract. J Gastroenterol 50:1005–1016
Ilczyszyn A, Botha AJ (2014) Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus 27:637–644
Su B, Attaar M, Wong H, Callahan ZM, Kuchta K, Stearns S, Linn JG, Denham W, Haggerty SP, Ujiki MB (2020) Using a standardized intra-operative endoflip protocol during fundoplication to identify factors that affect distensibility. Surg Endosc 35(10):5717–5723
DeHaan RK, Davila D, Frelich MJ, Gould JC (2017) Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc 31:193–198
Turner B, Helm M, Hetzel E, Gould JC (2019) Is that “floppy” fundoplication tight enough? Surg Endosc 34(4):1823–1828
Nathanson LK, Brunott N, Cavallucci D (2012) Adult esophagogastric junction distensibility during general anesthesia assessed with an endoscopic functional luminal imaging probe (EndoFLIP(R)). Surg Endosc 26:1051–1055
Valiati W, Fuchs KH, Valiati L, Freys SM, Fein M, Maroske J, Tigges H, Thiede A (2000) Laparoscopic fundoplication–short- and long-term outcome. Langenbecks Arch Surg 385:324–328
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Min P Kim is a consultant for Veran, Intuitive Surgical, and Medtronic. Edward Chan is a consultant for Veran. Anuj Shah, Duc T. Nguyen, Leonora M. Meisenbach, Ray Chihara, and Edward A. Graviss do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shah, A., Nguyen, D.T., Meisenbach, L.M. et al. A novel EndoFLIP marker during hiatal hernia repair is associated with short-term postoperative dysphagia. Surg Endosc 36, 4764–4770 (2022). https://doi.org/10.1007/s00464-021-08817-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08817-z