Abstract
Background
It is important to accurately diagnose the depth of colorectal neoplasia invasion. We aimed to evaluate the usefulness of a new forward-viewing radial-array echoendoscope (FRE), relative to the pit pattern method.
Methods
In this prospective study, the invasion depth of suspected early-stage carcinoma was diagnosed using the pit pattern and FRE methods. The diagnoses were classified as T1a (submucosal invasion distance < 1,000 μm) or shallower and T1b (≥ 1,000 μm) or deeper. Pathological diagnoses were used to compare the diagnostic capabilities of the two methods.
Results
The final analyses included 110 lesions. The FRE was successfully inserted to the lesion in all cases. There were no significant differences between the two methods regarding the correct prediction rate (79.1% vs. 75.5%, P = 0.57), accuracy (81.3% vs. 79.0%, P = 0.68), specificity (81.3% vs. 70.8%, P = 0.135), positive predictive value (65.0% vs. 60.4%, P = 0.649), negative predictive value (91.0% vs. 98.1%, P = 0.108), or frequency of unevaluable cases (2.7% vs. 4.5%, P = 0.471). The correct prediction rate was calculated by adding the number of unevaluable cases to the denominator of accuracy. Relative to the pit pattern method, the FRE method offered significantly higher sensitivity for predicting T1b or deeper invasion (81.3% vs. 97.0%, P = 0.048). The pit pattern method had significantly poorer accuracy for large lesions (> 36 mm) than for smaller lesions (≤ 36 mm). In contrast, the accuracy of the FRE method did not differ significantly with lesion size. When using the FRE method, no cases were unevaluable because of attenuation. The FRE method provided correct diagnoses in 2 of 3 cases that were unevaluable using the pit pattern method.
Conclusions
The pit pattern and FRE methods offered similar diagnostic performance for invasion depth. Furthermore, the FRE method may be used to correctly diagnose cases that are unevaluable using the pit pattern method.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Endoscopic treatments for early colorectal cancer have recently improved after the application of endoscopic submucosal dissection (ESD) in the colorectum [1,2,3,4,5,6]. These improvements have allowed more lesions to be treated endoscopically, although more precise pre-treatment diagnosis of invasion depth is needed to select the treatment strategy for colorectal neoplasia. For example, endoscopic treatment is used for adenoma and intramucosal cancers, which have no possibility of metastasis, while the treatment strategies for T1 cancer are determined based on the submucosal (SM) invasion distance. In T1a cases (SM invasion distance of < 1000 μm), endoscopic treatment is performed because of the very low probability of lymph node metastasis, while T1b cases (SM invasion distance of ≥ 1000 μm) are typically treated surgically, given the occurrence of lymph node metastasis in approximately 10–15% of cases [7, 8]. Surgical treatment is also selected for cases with a T2 or deeper classification. Therefore, it is very important to preoperatively distinguish between T1a or shallower cases and T1b or deeper cases.
There are several methods for diagnosing the depth of invasion for colorectal neoplasia. Endoscopic ultrasonography (EUS) is an established method with good accuracy. For example, Mukae et al. reported that the diagnostic accuracy of EUS was 89% (excluding difficult to evaluate cases) [9]. During EUS, the depth of invasion is typically evaluated using a high-frequency ultrasound probe (HFUP) or an oblique-viewing echoendoscope. However, because an HFUP has high frequency, attenuation can lead to cases being considered unevaluable [9, 10], which has led to some studies only targeting non-polypoid lesions [11,12,13]. Moreover, it can be difficult to deeply insert an oblique-viewing echoendoscope [14], and some studies have only targeted left colonic and rectal lesions [15]. Another approach to diagnose the depth of invasion is the pit pattern method, which is widely used, especially in Japan. Shimura et al. have reported that the pit pattern method has 71.2% accuracy [12].
Few reports have described the evaluation of invasion depth using a forward-viewing radial-array echoendoscope (FRE), although Kongkam et al. reported that the FRE is a feasible tool for determining T and N classifications for colon cancers beyond the rectum [14]. However, no reports have described using FRE to differentiate between T1a or shallower cases and T1b or deeper cases. In this context, we hypothesized that FRE might help to address the issues regarding ultrasound attenuation and deep insertion of the endoscope, which might make it a useful tool for determining the depth of invasion for colorectal neoplasia and differentiating between T1a or shallower cases and T1b or deeper cases. Therefore, this study aimed to prospectively evaluate the diagnostic performance of the pit pattern and FRE methods, as well as the insertability and related adverse events of the FRE.
Patients and methods
Study design and patients
This prospective single-center study was conducted at Nagoya University Hospital in Japan between August 2017 and June 2019 and was carried out in accordance with the principles of the Declaration of Helsinki. Patient data, including their general characteristics, were obtained from the medical records of our hospital. All patients provided written informed consent before their enrollment. The study’s protocol was approved by our institutional review board (2015–0381) and was registered with the University Hospital Medical Information Network Clinical Trials Registry (UMIN000028059).
The inclusion criteria were (1) age of > 20 years, (2) suspected early-stage carcinoma (intramucosal cancer and T1) based on conventional endoscopic observation using white-light imaging (WLI), (3) planned treatment using endoscopy or surgery, and (4) written informed consent. Patients were excluded when they had (1) a history of chemotherapy or radiation therapy; (2) an inappropriate lesion for study entry as judged by the investigators, such as a pedunculated lesion, a scaring lesion, or a lesion in ulcerative colitis; or (3) no final histology results for the lesion because lung metastases were detected using computed tomography after the endoscopy.
Study protocol
The study included patients with suspected early-stage carcinoma based on WLI findings, and chromoendoscopy with a 0.2% indigo-carmine solution was added in some cases to clarify the morphology (Fig. 1A). The WLI observation was performed by an independent physician who did not participate in the pit pattern or FRE evaluations. Before the pit pattern method was applied, enrolled patients were sedated using 5-mg midazolam intravenously (the dose was adjusted as needed), and an antispasmodic agent (such as intravenous 20-mg scopolamine butylbromide or 1-mg glucagon) was administered to all patients without contraindications or comorbidities. Invasion depth was first evaluated using the pit pattern method, and the results were recorded by one physician. The FRE evaluation was subsequently performed by another physician who was blinded to the pit pattern evaluation, in order to avoid bias related to the order of the evaluations. The insertion time of FRE and the procedure time for each method was measured. The participating physicians were four expert endoscopists who had each performed > 3000 pit pattern evaluations and > 100 conventional EUS evaluations. The pathological diagnosis of invasion depth was based on the surgical or endoscopic specimen to evaluate the accuracies of the pit pattern and FRE methods. Because the FRE evidence was insufficient for definitively diagnosing the depth of colorectal neoplasia invasion, the attending physician (no a study investigator) selected the treatment plan (endoscopic or surgical treatment) by combining all evaluation results from the WLI, pit pattern, and FRE evaluations, with the pit pattern set as the gold standard. We also evaluated the insertability and related adverse events of the FRE.
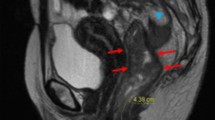
Representative images. A Conventional colonoscopy revealed a laterally spreading tumor in the rectum with a central depression (size: 25 mm). Chromoendoscopy with a 0.2% indigo-carmine solution helped clearly visualize the morphology. B Magnifying colonoscopy of the boxed area in (A) using a 0.05% crystal violet solution revealed the VN pit pattern. C The forward-viewing radial-array echoendoscope revealed a hypoechoic mass extending into the middle of the submucosal layer. The position of the muscularis mucosa could not be identified; thus, the submucosal invasion distance was measured from the lesion’s surface layer (4850 μm). D The histological assessment revealed that the cancer had invaded to the submucosal layer. The position of the muscularis mucosa could not be identified; thus, the submucosal invasion distance was measured from the lesion’s surface layer (4000 μm). The histological diagnosis was pT1b
Pit pattern diagnosis
All lesions were sprayed with a solution containing 0.05% crystal violet and then evaluated under × 80 magnification using a magnifying colonoscope (EC-L600ZP7; FUJIFILM CO., Tokyo, Japan) (Fig. 1B). The results were classified according to Kudo et al.’s pit patterns [16]. Types IIIL, IIIs, IV, VI, and VN were considered neoplastic patterns, including adenoma and cancers. Type VI was subdivided into type VI-h (highly irregular) and type VI-s (slightly irregular). Type VI-h was defined as a pit pattern with a narrowing pit, irregular edges, unclear outline, decline or loss of stromal area, or scratch signs. Type VI-s did not have any of these characteristics. For the present study, we assumed that types IIIL, IIIs, IV, and VI-s corresponded to an invasion depth of T1a or shallower and that types VI-h and VN corresponded to an invasion depth of T1b or deeper.
FRE diagnosis
All lesions were observed using an FRE (EG-580UR; FUJIFILM CO., Tokyo, Japan) (Fig. 1C). The FRE was inserted to the lesion, and the lumen of the colon was filled with distilled water. The balloon was not used to capture the endosonographic images. The available frequencies were 5, 7.5, 10, and 12 MHz, which were optimized for each case. In cases with a FRE diagnosis of a T1 lesion, the SM invasion distance was measured from the lower end of the muscularis mucosae (where identifiable) to the deepest part of the lesion. If the muscularis mucosae could not be identified or approximated, the invasion distance was measured from the surface of the lesion. The depth of invasion based on FRE was also classified as T1a (SM invasion distance of < 1000 μm) or shallower and T1b (SM invasion distance of ≥ 1000 μm) or deeper.
Pathological assessment
To determine the invasion depth, the surgical or endoscopic specimen was evaluated by a pathologist who was blinded to the pre-treatment diagnosis (Fig. 1D). Similar to the FRE evaluation, in pathological (p) T1 cases, SM invasion distance was measured from the lower end of the muscularis mucosae (where identifiable) to the deepest part of the lesion. If the muscularis mucosae could not be identified or approximated, the invasion distance was measured from the surface of the lesion. The pathological diagnosis of pT1 was classified as pT1a (SM invasion distance of < 1000 μm) or pT1b (≥ 1000 μm) [8].
Objectives and outcome measures
The primary study objective was to compare the pit pattern and FRE methods’ abilities to predict T1b or deeper invasion. The following measures of diagnostic performance were evaluated: correct prediction rate, accuracy, sensitivity, specificity, positive predictive value, and negative predictive value. The correct prediction rate was defined as (true positive cases + true negative cases)/(positive cases + negative cases + unevaluable cases). The correct prediction rate was calculated by adding the number of unevaluable cases to the denominator of accuracy. On the other hand, accuracy, sensitivity, specificity, positive predictive value, and negative predictive value were calculated according to the standard definitions after excluding all unevaluable cases. In addition to these, the procedure time was also evaluated. The procedure time in the pit pattern was the time from spraying the crystal violet to diagnosing with magnification. That in the FRE was the time from the beginning of the filling of the distilled water to evaluating the tumor depth. The secondary study objective was to perform risk analyses for incorrect diagnoses of invasion depth using the pit pattern and FRE methods. The risk analyses were only performed for evaluable cases. We also performed analyses for the following: (1) insertability and related adverse events of FRE, (2) detailed pathological assessments of FRE diagnoses in evaluable cases, and (3) cases that could not be evaluated using the pit pattern or FRE method.
Statistical analysis
In some papers, the accuracy using EUS was about 90% [17,18,19]. We estimated that the FRE diagnosis would increase the correct prediction rate for diagnosing invasion depth to 90% (vs. 75% for the pit pattern diagnosis). Based on a power of 80% and a two-sided test with a significance level of 5%, 100 patients would be needed. Thus, we targeted 120 patients to account for potential dropouts.
Univariate analyses were performed using the McNemar’s test, the χ2 test, Fisher’s exact probability test, or Wilcoxon signed-rank test. Multivariate analyses were performed using logistic regression. All analyses were performed using IBM SPSS software (version 24; IBM Corp., Armonk, NY, USA), and a P value < 0.05 was considered statistically significant.
Results
We enrolled 120 patients with 120 lesions, although 10 patients and 10 lesions were subsequently excluded (Fig. 2). Thus, data for 110 lesions were included in the final analysis. Table 1 shows the characteristics of the 110 lesions in the 110 patients. The mean lesion size was 36.0 mm, and all lesions had sizes of > 10 mm. Twenty-eight lesions were polypoid (25.5%) and 45 lesions (40.9%) were located at the proximal colon. The FRE was successfully inserted to evaluate all lesions and there were no adverse events related to the use of the FRE. The median time taken for FRE insertion to the lesions located in the cecum was 10.0 min.
After endoscopic or surgical treatment with final histology evaluations, 77 lesions (70.0%) were classified as pT1a or shallower (adenoma, intramucosal cancer, and pT1a) and 33 lesions (30.0%) were classified as pT1b or deeper (pT1b, pT2, and pT3).
Comparison of evaluability
When we compared the pit pattern and FRE methods, there was no significant difference in the frequencies of unevaluable cases (2.7% [3 cases] vs. 4.5% [5 cases], P = 0.471). All 3 cases (2.7%) that were unevaluable using the pit pattern method were related to insufficient staining on the lesion surface due to mucus. Among the cases that were unevaluable using the FRE method, 2 cases (1.8%) were related to peristalsis, 2 cases (1.8%) were related to location on the fold, and 1 case (0.9%) was related to insufficient water retention. Polypoid lesions accounted for approximately 25% of all cases, although attenuation did not interfere with the ability to evaluate these lesions using the FRE.
Comparisons of diagnostic performance
Table 2 shows the correct prediction rate (which includes cases that were judged unevaluable), accuracy, sensitivity, specificity, positive predictive value, and negative predictive value for diagnostic predictions of T1b or deeper invasion that were obtained using the pit pattern and FRE methods. The pit pattern and FRE methods provided similar correct prediction rates (79.1% vs. 75.5%, P = 0.57). In addition, no significant differences were observed between the two methods in terms of accuracy (81.3% vs. 79.0%, P = 0.68), specificity (81.3% vs. 70.8%, P = 0.135), positive predictive value (65.0% vs. 60.4%, P = 0.649), or negative predictive value (91.0% vs. 98.1%, P = 0.108). The FRE method had significantly higher sensitivity than the pit pattern method (81.3% vs. 97.0%, P = 0.048).
No significant difference was observed between the two methods in terms of procedure time (5.4 min [3.2–8.9] vs. 5.6 min [2.7–11.2], P = 0.218).
Risk factors for incorrect diagnosis
Tables 3 and 4 show the risk analyses for incorrect diagnoses of invasion depth that were obtained using the pit pattern and FRE methods. All of the risk analyses were limited to the evaluable cases. The univariate analyses of the pit pattern and FRE methods did not reveal any significant risk factors for incorrect diagnosis. All of the characteristics that were evaluated in the univariate analyses were included in the multivariate analyses of the two methods. For the pit pattern method, the multivariate analysis revealed that a lesion size of > 36 mm (mean tumor size) was an independent risk factor (P = 0.031, odds ratio: 3.233, 95% confidence interval: 1.115–9.373). In contrast, analyses of the FRE method showed that diagnostic accuracy did not differ significantly with lesion size. The FRE method provided similar accuracies for polypoid lesions and flat lesions.
Detailed pathological assessment of FRE diagnoses in evaluable cases
Table 5 summarizes the detailed pathological assessments of FRE diagnoses in evaluable cases. The pathological assessments revealed that the FRE method of predicting T1b or deeper invasion was more likely to overestimate depth than to underestimate depth (21 cases vs. 1 case).
Using FRE in cases unevaluable using the pit pattern method
Table 6 shows the FRE diagnoses of the cases that were unevaluable using the pit pattern method. In the first case, an FRE diagnosis was also impossible because of peristalsis. In the second case, the FRE diagnosis was T1a or shallower, and the pathological diagnosis was intramucosal cancer. In the third case, the FRE diagnosis was T1b or deeper, and the pathological diagnosis was pT1b. Thus, in the two cases for which FRE was possible, the FRE diagnosis matched the pathological diagnosis.
Using the pit pattern method in cases unevaluable using FRE
Table 7 shows the pit pattern diagnoses of the cases that were unevaluable using the FRE method. In one of them, the pit pattern diagnosis was also impossible due to the presence of mucus. Three of them could not be diagnosed correctly by the pit pattern diagnosis, while one of them could be diagnosed correctly.
Discussion
The present study evaluated whether FRE could be used to accurately diagnose the depth of colorectal neoplasia invasion and differentiate between cases with invasion depths corresponding to T1a or shallower and T1b or deeper. An HFUP or oblique-viewing echoendoscope is typically used during EUS to diagnose invasion depth, although these tools are associated with several issues. For example, the high frequency of HFUPs (mainly 12–20 MHz) leads to issues with echo attenuation, which can make a case unevaluable, particularly when an HFUP is used for polypoid lesions. In contrast, the FRE we evaluated uses a frequency of 5–12 MHz, which should be associated with less attenuation, even for polypoid lesions. The images of HFUP and FRE in the evaluation of polypoid lesions are shown in Fig. 3. Since we did not include HFUP observations in the protocol of this study, we prepared the HFUP image of another polyp with size and morphology similar to the polyp presented in FRE. As shown in Fig. 3A, when HFUP with a frequency of 20 MHz was used to observe a polyp with a height of about 15 mm, it was difficult to evaluate the deep portion, due to attenuation. Conversely, in Fig. 3B, when FRE with a frequency of 7.5 MHz was used to observe a similar polyp with a height of about 15 mm, it was possible to evaluate the invasion depth of the polyp without attenuation. In this FRE image, the lesion did not invade the submucosa and was diagnosed as intramucosal cancer. It is highly likely that FRE could make it possible to estimate the tumor depth that could not be evaluated by HFUP.
Conventional echoendoscopes in the colon are oblique-viewing, which sometimes makes them difficult to insert into the deep colon. In contrast, the FRE’s forward view addresses this issue and improves insertability because we could successfully insert the FRE to all lesions, including the lesions in the proximal colon, which accounted for approximately 40% of the overall study cohort. The median time taken for insertion to the lesions in the cecum by FRE was 10.0 min. In a previous paper [20], the median insertion time to the cecum using the normal colonoscope (model CF260H or CF260HZ; Olympus Optical, Tokyo, Japan) by the attending physician (with > 2000 total career colonoscopies) was 11.8 min. Thus, the insertion time in this study and that in the previous study are similar. The working length of the FRE was 1250 cm, which is shorter than that of the intermediate-length colonoscope. However, the insertability of FRE is good, and it was possible to insert it into the proximal colon without forming a loop in most cases. Hence, there was little difficulty in insertion due to the shorter working length of FRE.
Several studies have compared the accuracies for diagnosing colorectal neoplasia invasion depth between EUS and magnifying chromoendoscopy methods, which include the pit pattern method. However, the results of these studies are conflicting [12, 13, 17,18,19, 21]. In addition, some of the studies did not include cases that were judged unevaluable using EUS, or did not describe the related results. Furthermore, other studies were biased by the order of the diagnostic methods.
In the present study, the pit pattern and FRE methods had similar correct prediction rates, accuracies, and frequencies of unevaluable cases. The FRE method also offered similar accuracies for polypoid and flat lesions. The FRE method had significantly higher sensitivity for predicting T1b or deeper invasion than the pit pattern method. Moreover, our assessments were blinded to avoid bias related to the order of the evaluation. These findings show that the FRE method has similar diagnostic performance and better sensitivity than the pit pattern method for diagnosing the depth of colorectal neoplasia invasion. The reason why the accuracy of FRE in this study was lower than that in previous EUS studies might be because the pit pattern and EUS were performed in an unblinded manner in some of these studies. However, in this study, FRE was performed by another endoscopist who did not know the result of the pit pattern.
With respect to procedure time, there was no significant difference between pit pattern and FRE evaluations. A previous report has indicated that the procedure time was longer for EUS than for magnifying chromoendoscopy [12]. Interestingly, there was no significant difference in the procedure times for the pit pattern and FRE evaluations in our study, despite the fact that the lesion size in our study was larger than that in the previous report [12]. In this context, magnifying chromoendoscopy requires a longer time to evaluate large lesions, while FRE has a broader evaluation range and does not require a prolonged time to evaluate even large lesions. This suggests that the burden on the patient’s body while performing FRE is not much different than that while performing pit pattern diagnosis.
A lesion size of > 36 mm was an independent risk factor for incorrect diagnoses of invasion depth using the pit pattern method. Conversely, the lesion size in the FRE assessment was not associated with any significant difference in diagnostic accuracy. Our results show that the FRE method can be used to correctly diagnose the invasion depth, regardless of lesion size. When using the FRE method to diagnose the invasion depth of large lesions, we attempted to move the scope in all directions relative to the lesion, scan all parts of the lesion, and capture the deepest part of the lesion.
We also examined the detailed pathological assessments of FRE diagnoses in evaluable cases. The FRE method has the advantage of a high sensitivity for predicting T1b or deeper invasion. However, its specificity seemed to be lower than that of pit pattern diagnosis although the difference was not statistically significant. While using the FRE method, overestimation of invasion depth is more likely than underestimation of invasion depth. Overestimation of invasion depth is a concern because it may lead to unnecessary surgical management of the lesion. When the FRE indicate T1b or deeper images, the endoscopist must adopt the FRE result with caution. If necessary, it is better to perform another procedure to determine the treatment necessary to improve diagnostic reliability.
Most previous studies have distinguished between clinical T1a and T1b disease using EUS to evaluate the form of the SM layer, rather than making this distinction based on the invasion distance [10]. The form of the SM layer becomes slightly narrow in T1a cases, but distinctly thin or obscure in T1b cases. However, one study also reported a significant correlation between the histological and HFUP diagnoses of the SM invasion distance [22]. Thus, we evaluated the SM invasion distance using FRE in T1 cases and classified the results as T1a (< 1000 μm) or T1b (≥ 1000 μm) based on the distance from the lower end of the muscularis mucosa (or the lesion’s surface layer) to the deepest part of the tumor. This method is similar to and complements the existing guidelines for pathological evaluations [8]. Although few reports have described using this technique, we believe it is useful based on the similar accuracies of the pit pattern and FRE methods.
Although the FRE did not significantly improve the correct prediction rate of invasion depth, it was similar to that for the pit pattern method. Furthermore, the FRE correctly diagnosed 2 of 3 cases that were unevaluable using the pit pattern method. Thus, FRE may be effective even in cases that are unevaluable using the pit pattern method (e.g., because of mucus). Because of the high sensitivity of FRE for predicting T1b or deeper invasion, we suggest that endoscopic treatment should be indicated for cases diagnosed as VI-h using the pit pattern method, but as T1a or shallower using the FRE method.
The present study has two important limitations. The first limitation is that the patients received intravenous injections of scopolamine butylbromide or glucagon, which were followed by the pit pattern diagnosis and then the FRE diagnosis. Thus, peristalsis was more likely to occur during the FRE diagnosis and might have worsened the observation conditions. It might also be prudent to consider two groups of patients in future studies, with one group undergoing the pit pattern diagnosis first and the other group undergoing the FRE diagnosis first. The second limitation is the study’s single-center design and small sample size. A larger multi-center study will be needed to validate our findings. It would also be useful to evaluate FRE performance in other countries. The third limitation was that the insertion time of FRE was compared with that reported in previous studies, not directly compared with the insertion time in this study of the magnifying colonoscope.
In conclusion, the present study revealed that the FRE method has similar ability to predict the depth of colorectal neoplasia invasion, relative to the pit pattern method. Furthermore, the FRE method remained useful in cases with polypoid lesions, lesions at the proximal colon, and larger lesions. Moreover, the FRE method may correctly diagnose cases that are unevaluable using the pit pattern method.
References
Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 72:1217–1225
Nakajima T, Saito Y, Tanaka S, Iishi H, Kudo SE, Ikematsu H, Igarashi M, Saitoh Y, Inoue Y, Kobayashi K, Hisasbe T, Matsuda T, Ishikawa H, Sugihara K (2013) Current status of endoscopic resection strategy for large, early colorectal neoplasia in Japan. Surg Endosc 27:3262–3270
Fujiya M, Tanaka K, Dokoshi T, Tominaga M, Ueno N, Inaba Y, Ito T, Moriichi K, Kohgo Y (2015) Efficacy and adverse events of EMR and endoscopic submucosal dissection for the treatment of colon neoplasms: a meta-analysis of studies comparing EMR and endoscopic submucosal dissection. Gastrointest Endosc 81:583–595
Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Kudo SE, Tsuruta O, Sugihara K, Watanabe T, Saitoh Y, Igarashi M, Toyonaga T, Ajioka Y, Ichinose M, Matsui T, Sugita A, Sugano K, Fujimoto K, Tajiri H (2015) JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 27:417–434
Ikematsu H, Yoda Y, Matsuda T, Yamaguchi Y, Hotta K, Kobayashi N, Fujii T, Oono Y, Sakamoto T, Nakajima T, Takao M, Shinohara T, Murakami Y, Fujimori T, Kaneko K, Saito Y (2013) Long-term outcomes after resection for submucosal invasive colorectal cancers. Gastroenterology 144:551–559
Fujishiro M, Yahagi N, Kakushima N, Kodashima S, Muraki Y, Ono S, Yamamichi N, Tateishi A, Oka M, Ogura K, Kawabe T, Ichinose M, Omata M (2007) Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol 5:678–683
Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, Kumamoto T, Ishiguro S, Kato Y, Shimoda T, Iwashita A, Ajioka Y, Watanabe H, Watanabe T, Muto T, Nagasako K (2004) Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol 39:534–543
Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kawano H, Kinugasa Y, Kokudo N, Murofushi K, Nakajima T, Oka S, Sakai Y, Tsuji A, Uehara K, Ueno H, Yamazaki K, Yoshida M, Yoshino T, Boku N, Fujimori T, Itabashi M, Koinuma N, Morita T, Nishimura G, Sakata Y, Shimada Y, Takahashi K, Tanaka S, Tsuruta O, Yamaguchi T, Yamaguchi N, Tanaka T, Kotake K, Sugihara K, Japanese Society for Cancer of the Colon, and Rectum (2018) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol 23:1–34
Mukae M, Kobayashi K, Sada M, Yokoyama K, Koizumi W, Saegusa M (2015) Diagnostic performance of EUS for evaluating the invasion depth of early colorectal cancers. Gastrointest Endosc 81:682–690
Kobayashi K, Kida M, Katsumata T, Yoshiwaza S, Yokoyama K, Sada M, Igarashi M, Saigenji K (2003) Clinical role of endoscopic ultrasonography for the diagnosis of early colorectal cancer and selecting the treatment procedure. Dig Dis Sci 15:298–305
Hurlstone DP, Cross SS, Adam I, Shorthouse AJ, Brown S, Sanders DS, Lobo A (2004) Efficacy of high magnification chromoscopic colonoscopy for the diagnosis of neoplasia in flat and depressed lesions of the colorectum: a prospective analysis. Gut 53:284–290
Shimura T, Ebi M, Yamada T, Hirata Y, Nishiwaki H, Mizushima T, Asukai K, Togawa S, Takahashi S, Joh T (2014) Magnifying chromoendoscopy and endoscopic ultrasonography measure invasion depth of early stage colorectal cancer with equal accuracy on the basis of a prospective trial. Clin Gastroenterol Hepatol 12:662–668
Yamada T, Shimura T, Ebi M, Hirata Y, Nishiwaki H, Mizushima T, Asukai K, Togawa S, Takahashi S, Joh T (2015) Subset analysis of a multicenter, randomized controlled trial to compare magnifying chromoendoscopy with endoscopic ultrasonography for stage diagnosis of early stage colorectal cancer. PLoS ONE 10:1–12
Kongkam P, Linlawan S, Aniwan S, Lakananurak N, Khemnark S, Sahakitrungruang C, Pattanaarun J, Khomvilai S, Wisedopas N, Ridtitid W, Bhutani MS, Kullavanijaya P, Rerknimitr R (2014) Forward-viewing radial-array echoendoscope for staging of colon cancer beyond the rectum. World J Gastroenterol 20:2681–2687
Bhutani MS, Nadella P (2001) Utility of an upper echoendoscope for endoscopic ultrasonography of malignant and benign conditions of the sigmoid/left colon and the rectum. Am J Gastroenterol 96:3318–3322
Kudo S, Rubino C, Teixeira C, Kashida H, Kogure E (2004) Pit pattern in colorectal neoplasia: endoscopic magnifying view. Endoscopy 33:367–373
Haruki S, Kobayashi K, Yokoyama K, Sada M, Koizumi W (2012) Comparison of diagnostic accuracies of various endoscopic examination techniques for evaluating the invasion depth of colorectal tumors. Gastroenterol Res Pract 2012:1–7
Hurlstone DP, Brown S, Cross SS, Shorthouse AJ, Sanders DS (2005) High magnification chromoscopic colonoscopy or high frequency 20 MHz mini probe endoscopic ultrasound staging for early colorectal neoplasia: a comparative prospective analysis. Gut 54:1585–1589
Matsumoto T, Hizawa K, Esaki M, Kurahara K, Mizuno M, Hirakawa K, Yao T, Iida M (2002) Comparison of EUS and magnifying colonoscopy for assessment of small colorectal cancers. Gastrointest Endosc 56:354–360
Nagata N, Sakamoto K, Arai T, Niikura R, Shimbo T, Shinozaki M, Noda M, Uemura N (2014) Predictors for cecal insertion time: The impact of abdominal visceral fat measured by computed tomography. Dis Colon Rectum 57:1213–1219
Fu KI, Kato S, Sano Y, Onuma EK, Saito Y, Matsuda T, Koba I, Yoshida S, Fujii T (2008) Staging of early colorectal cancers: magnifying colonoscopy versus endoscopic ultrasonography for estimation of depth of invasion. Dig Dis Sci 53:1886–1892
Tanaka S, Yoshida S, Chayama K (2004) Clinical usefulness of high-frequency ultrasound probes for new invasion depth diagnosis in submucosal colorectal carcinoma. Dig Endosc 16:161–164
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Takeshi Kuno, Takeshi Yamamura, Masanao Nakamura, Keiko Maeda, Tsunaki Sawada, Yasuyuki Mizutani, Masaya Esaki, Takuya Ishikawa, Kazuhiro Furukawa, Eizaburo Ohno, Hiroki Kawashima and Mitsuhiro Fujishiro have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuno, T., Yamamura, T., Nakamura, M. et al. A forward-viewing radial-array echoendoscope is useful for diagnosing the depth of colorectal neoplasia invasion. Surg Endosc 35, 4389–4398 (2021). https://doi.org/10.1007/s00464-020-07936-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07936-3