Abstract
Background
Outcomes of incisional hernia repair (IHR) include recurrence and quality of life (QOL). Operative approaches include laparoscopic, open, and robotic approaches. Data regarding comparative QOL outcomes among these repair types are unknown. Our study evaluates quality of life after three approaches to IHR.
Study design
Patients undergoing open (OHR), laparoscopic (LIHR), and robotic extra-peritoneal (RIHR) at a single institution from 2009 to 2019 were reviewed from a prospectively managed quality database. Short-term QOL was compared among the three procedures using the Surgical Outcomes Measurement System (SOMS) and Carolinas Comfort Scale (CCS), objective pain scores and postoperative narcotic use. Data regarding length of stay (LOS), emergency department (ED) visits, readmission, reoperations and surgical site infection (SSI) were also collected.
Results
A total of 795 patients undergoing IHR were analyzed (418 open, 300 laparoscopic and 77 robotic). Patient were similar in age, gender and co-morbidities. LIHR patients had higher BMI and RIHR patients had larger hernia and mesh size. LOS was longer and rate of SSI was higher for OIHR compared to laparoscopic and RIHR. Patients undergoing LIHR reported increased narcotic use, Visual Analogue Scale (VAS) and CCS pain scores compared to open and robotic repair. Return to daily activity was 4 days shorter for robotic than open and laparoscopic repair; ED visits, readmissions, reoperations, and other QOL domains were similar.
Conclusion
Our data suggests that short-term quality of life after robotic extra-peritoneal IHR is improved compared to open and laparoscopic repair. Additional follow up is required to determine differences in long-term QOL after IHR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
An incisional hernia is a type of ventral hernia which occurs when a protrusion of tissue forms at the site of a previous surgical scar [1]. Incisional hernias (IH) develop at an approximate rate of 15–20%, and it has been estimated that about 400,000–600,000 IH are repaired in the US each year [2]. The only definitive treatment for IH is surgical repair. There are multiple surgical approaches, as incisional hernia repair (IHR) procedures can by performed by open-incisional hernia repair (OIHR), laparoscopic incisional hernia repair (LIHR), and robotic extra-peritoneal incisional hernia repair (RIHR).
It has been previously established that a decreased length of stay, faster return to work, and a lower rate of surgical site infection are all associated with LIHR when compared to OIHR [2]. Robotic IHR has been proposed as an alternative to these. Studies suggest that the benefit of robotic approach may be related to improved dexterity and ergonomics with minimally invasive approach [3, 4]. The platform for RIHR that the surgeon uses also provides an operative field with ten-times magnification as well as three-dimensional imaging, and robotic instruments also provide a degree of freedom greater than the human wrist [4]. One study comparing LIHR to RIHR demonstrated no significant difference in perioperative outcomes [3]. Others have shown that RIHR is associated with a higher risk of postoperative morbidity including infection, though without a difference in mortality, 30-day readmission, length of stay (LOS), and postoperative pain medication use [5]. However, little data exists regarding short term quality of life outcomes after RIHR when compared to LIHR and OIHR.
We aim here to report our short-term quality of life outcomes among the various surgical approaches in treating IH, with a specific focus on RIHR. We hypothesize that patients who undergo RIHR will have better short-term quality of life compared to patients who undergo LIHR or OIHR.
Methods
Patient population
Patients undergoing OIHR, LIHR, and RIHR (n = 795) from 2009 to 2019 at a single institution were identified from a prospectively managed quality database at NorthShore University HealthSystem. This database consists of all incisional hernia repairs performed HealthSystem by four board-certified general surgeons. Of note, RIHR was started in 2017 and is currently performed by only two of the surgeons. Data extraction was conducted in accordance with the IRB-approved protocol.
Data collected
The preoperative factors that were collected included age at surgery, gender, body mass index (BMI), smoking status, steroid use, incarceration, strangulation, obstruction, hernia reduciblity, medical comorbidities, prior hernia repair of any type, whether the hernia was recurrent, and prior abdominal surgeries. Intra-operative variables collected included hernia size, American Society of Anesthesiologist (ASA) class, operative time, mesh size, mesh type, whether primary closure was performed, and estimated blood loss. Post-operative outcomes collected include: LOS, pain score at discharge, duration of narcotic use, return to activities of daily living (ADL), emergency department visits within 30 days of the surgery, readmission within 30 days of the surgery, reoperation within 30 days of the surgery, surgical site infection, recurrence, seroma, and hematoma. Surgical site infections were classified using the ACS National Surgical Quality Improvement Program (NSQIP) operation manual.
Health-related quality of life surveys
The Surgical Outcomes Measurement Systems (SOMS) is sent to patients preoperatively, and postoperative at 3 weeks and 6 months. The Carolinas Comfort Scale (CCS) is only sent to patients postoperatively as it is focused specifically on the repair itself. Both of these tools have been validated for use in patients undergoing hernia repair [6,7,8]. Preoperative SOMS survey data generates Pain Impact (scored 6–30), Pain Quality (4–21), Pain VAS (0–10), Fatigue (7–35), and Physical Functioning (7–36) scores. Furthermore the postoperative 3 week and 6th month SOMS questionnaires generate the same five scores as the preoperative questionnaire as well as additional question for Body Image (4–20) and Satisfaction (0–11). Higher scores are better for SOMS Physical Functioning and Satisfaction. Lower scores are better for all other QOL domains. On the other hand, CCS questionnaires generate Mesh Sensation (0–40), Pain (0–40), Movement (0–35) and Total scores (0–115). Each question from the CCS is scored on a 5-point scale, 5 representing “disabling symptoms,” 4 representing “severe symptoms,” 3 representing “moderate/daily symptoms,” 2 representing “mild/bothersome symptoms,” 1 representing “mild/not bothersome symptoms” and 0 representing “no symptoms.”
Operative technique
Open incisional hernia repair was performed in an extraperitoneal or retrorectus fashion with permanent or absorbable, non-composite mesh placement as a sublay technique, using transfacial suture fixation of the mesh. Transversus abdominis release was used selectively.
Laparoscopic incisional hernia repair performed as an intraperitoneal underlay using a composite mesh, with and without primary fascial closure, as noted. Mesh fixation was performed using a combination of sutures and tacks.
Robotic extra-peritoneal incisional hernia repair is performed as a transabdominal, extraperitoneal repair with fascial closure and sublay non-composite mesh in all cases. Transversus abdominis release was utilized selectively.
Statistical analysis
Pre- and intra-operative factors, post-operative outcomes, and patient-reported QOL for each surgical approach are displayed as mean with standard deviation, median with interquartile range, or frequency with percentage. Differences between groups were evaluated, and post hoc adjustments for multiple comparisons were made. Normally distributed numeric data was assessed using analysis of variance (ANOVA) and the Tukey–Kramer test, while ordinal and non-normal numeric data were assessed using the Kruskall–Wallis test and the Dwass, Steel, Critchlow-Flinger method for multiple comparisons. Categorical data were assessed with chi-square or Fisher’s exact tests and the Bonferroni correction for multiple comparisons. Multivariable linear and logistic regression was used to analyze differences in outcomes while controlling for age, BMI, sex and hernia size. All statistical analysis was performed with SAS 9.3 with two-tailed tests and a significance level of p = 0.05.
Results
Patient preoperative characteristics
During the study period, a total of 795 patients who underwent IHR were analyzed (418 open, 300 laparoscopic, 77 robotic). Preoperative and intra-operative patient characteristics are summarized in Table 1. Age (64 ± 14 vs. 60 ± 14 vs. 63 ± 11; p = 0.001), male sex (44.5% vs. 36.7% vs. 49.4%; p = 0.043), and BMI (30.7 ± 7.0 vs. 32.9 ± 7.1 vs. 32.4 ± 6.6; p < 0.001) were different between OIHR, LIHR, and RIHR patients. Those who underwent OIHR used steroids (5.0% vs. 2.0% vs. 0.0%; p = 0.020) and had prior hernia repairs (35.4% vs. 27.3% vs. 20.8%; p = 0.009) more frequently than LIHR or RIHR. More RIHR patients had reducible hernias than OIHR or LIHR (98.7% vs. 91.4% vs. 85.0%; p = 0.001). In terms of comorbidities, a higher proportion of patients diagnosed with congestive heart failure (CHF) (3.3% vs. 1.0% vs. 0%; p = 0.039) and coronary artery disease (CAD) (8.4% vs. 3.7% vs. 3.9%; p = 0.0241) underwent open repair more frequently than LIHR or RIHR. Twenty-eight (6.7%) patients undergoing OIHR, zero patients undergoing LIHR, and twenty-two (28.6%) patients undergoing RIHR required transversus abdominis muscle release (TAR) (p < 0.0001), each of these groups are significantly different from the others. Rates of current smokers, diabetes, COPD and recurrent hernia were not different between groups.
Postoperative period
Intraoperative details are summarized in Table 2. Notably, median LOS was significantly longer in patients who underwent OIHR than patients who underwent LIHR or RIHR (72 vs. 28 vs. 26 h; p < 0.001). Multivariable analysis showed that LOS is about 42 (p < 0.001) and 60 (p < 0.001) hours longer in patients who underwent OIHR than those who underwent LIHR or RIHR, respectively. Pain at discharge, as measured by a visual analogue scale, was significantly higher in patients who underwent LIHR than patients who underwent OIHR (3.4 ± 2.3 vs. 2.4 ± 2.2; p < 0.001). Patients who underwent RIHR self-reported stopping their medication (2.4 ± 4.0 vs. 4.6 ± 4.3 vs. 5.4 ± 4.6 days; p < 0.001) and returning to daily activities (9.1 ± 7.1 vs. 9.1 ± 7.1 vs. 9.0 ± 6.4 days; p < 0.001) significantly earlier than patients who underwent OIHR or LIHR. Patients reported stopping their medication about 2 (p = 0.001) and 3 (p < 0.001) days earlier for RIHR than open or LIHR, respectively. Return to daily activities was reported to be 5 (p = 0.001) and 4 (p < 0.001) days earlier for RIHR than open or LIHR, respectively. Rate of SSI (4.5% vs. 1.0% vs. 0.0%; p < 0.001) was significantly higher and rate of seroma (12.9% vs. 20.7% vs. 29.9%; p < 0.001) was significantly lower in patients who underwent OIHR than patients who underwent LIHR or RIHR. Rate of urinary retention (2.0% vs. 0.0%; p = 0.046) and rate of suture fixation tenderness (3.8% vs. 0.0%; p = 0.011) were higher in those who underwent LIHR than those who underwent RIHR. Results are summarized in Table 3.
Quality of life
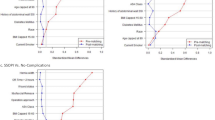
171 SOMS preoperative surveys were analyzed (78 open, 75 laparoscopic, and 18 robotic). Results are summarized in Table 4. Physical functioning was higher for LIHR than OIHR or RIHR (31.7 ± 5.2 vs. 30.8 ± 5.6 vs. 28.0 ± 7.4; p = 0.049). 212 SOMS 3 week postoperative surveys were analyzed (95 open, 74 laparoscopic, and 43 robotic). There were no statistically significant differences among the three groups. At 3 weeks postop, 152 CCS surveys were analyzed (66 open, 62 laparoscopic, and 24 robotic). Those who underwent LIHR had higher pain than those who underwent OIHR (11.5 ± 8.8 vs. 8.2 ± 9.8; p < 0.05). 76 SOMS 6 month postoperative surveys were analyzed (38 open, 26 laparoscopic, and 12 robotic). Those who underwent OIHR reported feeling worse about their body image than those who underwent LIHR or RIHR (8.2 ± 4.2 vs. 5.1 ± 2.1 vs. 4.5 ± 0.7; p < 0.001). 68 CCS 6 month postoperative surveys were analyzed (31 open, 28 laparoscopic, and 9 robotic). Pain was significantly higher in those who underwent OIHR than those who underwent LIHR (7.7 ± 10.1 vs. 1.9 ± 3.9; p < 0.05).
Multivariable analysis controlling for age, BMI, sex, hernia size, and recurrence status showed that there were no significant differences among surgery types for any SOMS or CCS at 3 weeks post operation. SOMS pain quality at 6 months was about 2.5 points higher (p = 0.011) for OIHR than LIHR. SOMS pain VAS at 6 months was about 1.5 higher (p = 0.020) for OIHR than LIHR. SOMS body image at 6 months was 3.5 (p < 0.001) and 4 (p = 0.001) points higher for OIHR than for LIHR or RIHR, respectively. CCS mesh sensation was 4 points higher (p = 0.008), CCS pain was 6.5 points higher (p = 0.001), and CCS total score was about 13 points higher (p = 0.010) for OIHR than LIHR, all indicating worse outcomes.
Discussion
This study is the first to report short and intermediate term quality of life outcomes among OIHR, LIHR, and RIHR. Since the recurrence risk among all three repair types is relatively low, the majority of patients undergoing these repairs will not suffer a recurrence. Therefore, quality of life outcomes and perioperative morbidity may be equally important in defining success in IHR.
Our data suggest that patients undergoing RIHR use less pain medication and resume normal activities sooner than those undergoing either LIHR and OIHR. Like others, our data indicates that median LOS was significantly longer in patients who underwent OIHR as compared to those who underwent LIHR or RIHR. Other outcomes such as SOMS body image, CCS mesh sensation, CCS pain were inferior for patients undergoing OIHR compared to either LIHR or RIHR. It is interesting that we see a difference in pain scores on CCS but not SOMS, and this may be due to the fact that SOMS reflects generalized postoperative quality of life and CCS is a more hernia-specific tool evaluating hernia and mesh QOL outcomes. As such, CCS may better reflect pain at the surgical site. However, total CCS scores were not significantly different between groups. When comparing LIHR to OIHR, OIHR was associated with a longer LOS. LIHR had higher VAS pain at discharge.
Similar to other studies, OIHR was associated with a higher risk of SSI. However, the opposite was true in regards to seroma development, as it was highest in the robotic group, followed by the laparoscopic group, and lowest in the open repair group. This is consistent with prior studies [9]. The exact mechanism by which seroma formation is higher after minimally invasive repair is not fully elucidated, but may be related to leaving hernia sac intact with robotic repair compared to open. Of note, surgeons at our center do not perform routine drainage of seromas, and no seromas required percutaneous drainage in this cohort of patients. Unfortunately, time to resolution for seromas is not a variable that collected in our database. Comparing resolution time among lap, robotic, and open groups in the future may be helpful in counseling patients preoperatively.
Donkor, et al. [2] showed that LIHR had a decreased length of stay and a lower rate of infection as compared to OIHR. Our study demonstrates similar findings. Priscila et al. [5] found that RIHR had a higher rate of complication and postoperative infections when compared to LIHR this conflicts what we found, as we found that the rate of SSI within 30 days of the procedure was significantly different between RIHR vs. OIHR and LIHR vs. OIHR, but that there was no statistical difference between RIHR vs. LIHR. Our results also differ from theirs as they found that there was no difference in postoperative pain medication use between LIHR vs. RIHR, however we found that patients undergoing RIHR stopped their medication significantly earlier than those who underwent LIHR. However our results do agree with Priscila et al. [5] in that we also did not find a statistical difference between 30-day readmission and length of stay between RIHR vs. LIHR.
Our study does have limitations. Because of later adoption of RIHR compared to LIHR and OIHR in our institution, the number of patients in the robotic hernia group was lower than in the other two cohorts. However, the significant quality of life benefits with RIHR will likely persist with increased numbers of patients. Other differences may reach statistical significance with more patients in the RIHR group over time.
An additional limitation relates to potential selection bias. Not all surgeons offered all three approaches, particularly as surgeon C performed the majority of robotic repairs. The introduction of robotic approach to our group’s practice likely includes considerations of learning curve, and the indication for each approach evolved over the course of surgeons’ learning curves. In general, robotic approaches are currently utilized in Ventral Hernia Working Group 2 patients with increased risk of surgical site outcomes. The use of transversus abdominis release is also worth noting, as listed in Table 2, with greater utilization in the robotic group than open or laparoscopic. This likely reflects an additional evolving practice with more appropriate utilization later in the study period.
Patient characteristic data would suggest that significant selection bias does not exist. More globally, and consistent with national trends in complex hernia surgery, selection bias may exist in that more open incisional hernia repairs were performed earlier in the study period, and the development of enhanced recovery after surgery (ERAS) protocols may have affected the differences in surgical outcomes, as length of stay and narcotic use would be expected to be lower in those enrolled in an ERAS pathway. This is an active area of study at our institution and in general, more homogenous data with sample sizes that allow for patient matching is necessary. There is also likely aselection bias in terms of medical comorbities, as patients diagnosed with CHF or CAD are more likely to undergo OIHR. This may be due to their inability to tolerate pneumoperitoneum and to limit operative time. An additional limitation may include the method of assessment of return to normal activities after surgery. Patients report the postoperative date on which they resumed normal activities, but this is not a detailed, objective assessment of several activities of daily living. Further detailed assessment may provide additional insight in short term QOL.
The final limitation of our study, and of others examining objective outcomes after robotic surgery, deals with cost. This study does not compare cost among these operative approaches, and many have highlighted the increased cost of robotic surgery as a potential detractor for this approach [10,11,12]. This may be the case in our cohort, though we do not have that data available. Ideally, a cost comparison among the three approaches would include a measure of patients’ LOS, ability to return to work, return to normal activities, and regular physical functioning, as these may prove worth some additional cost. Further cost analyses could be designed to assess whether the benefits of LIHR and RIHR outweigh the cost of the procedure.
Conclusion
Our study reports short-term quality of life outcomes for patients undergoing incisional hernia repair. Minimally invasive approach of either laparoscopic or robotic confers some quality of life benefit over OIHR. Robotic approach may offer some early QOL benefit compared to other approaches. Patients discontinue pain medication and resume normal activities sooner with robotic approach. Additional study is required to determine differences in quality of life among the three approaches in the long term.
Abbreviations
- IH:
-
Incisional hernia
- IHR:
-
Incisional hernia repair
- OIHR:
-
Open incisional hernia repair
- LIHR:
-
Laparoscopic incisional hernia repair
- RIHR:
-
Robotic extra-peritoneal incisional hernia repair
- LOS:
-
Length of stay
- BMI:
-
Body mass index
- ASA:
-
American Society of Anesthesiologist
- ADL:
-
Return to activities of daily living
- NSQIP:
-
National Surgical Quality Improvement Program
- SOMS:
-
Surgical Outcomes Measurement System
- CCS:
-
Carolinas Comfort Scale
References
Al Chalabi H, Larkin J, Mehigan B, McCormick P (2015) A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis of randomized controlled trials. Int J Surg 20:65–74. https://doi.org/10.1016/j.ijsu.2015.05.050
Donkor C, Gonzalez A, Gallas M, Helbig M, Weinstein C, Rodriguez J (2017) Current perspectives in robotic hernia repair. Robot Surg 4:57–67. https://doi.org/10.2147/RSRR.S101809
Coakley KM, Sims SM, Prasad T, Lincourt AE, Augenstein VA, Sing RF, Heniford BT, Colavita PD (2017) A nationwide evaluation of robotic ventral hernia surgery. Am J Surg 214:1158–1163. https://doi.org/10.1016/j.amjsurg.2017.08.022
Warren JA, Love M (2018) Incisional hernia repair: minimally invasive approaches. Surg Clin North Am 98:537–559. https://doi.org/10.1016/j.suc.2018.01.008
Armijo P, Pratap A, Wang Y, Shostrom V, Oleynikov D (2018) Robotic ventral hernia repair is not superior to laparoscopic: a national database review. Surg Endosc 32:1834–1839. https://doi.org/10.1007/s00464-017-5872-7
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206:638–644. https://doi.org/10.1016/j.jamcollsurg.2007.11.025
Heniford B, Lincourt A, Walters A, Colavita P, Belyansky I, Kercher K, Sing R, Augenstein V (2018) Carolinas Comfort Scale as a measure of hernia repair quality of life: a reappraisal utilizing 3788 international patients. Ann Surg 267:171–176. https://doi.org/10.1097/SLA.0000000000002027
Vigneswaran Y, Gitelis ME, Lapin B, Wang E, Butt Z, Carbray J, Payne S (2015) The surgical outcomes measurement system is a superior measure of patient-centered outcomes after hernia repair. J Am Coll Surg 221:79
Warren JA, Cobb WS, Ewing JA, Carbonell AM (2017) Standard laparoscopic versus robotic retromuscular ventral hernia repair. Surg Endosc 31:324–332. https://doi.org/10.1007/s00464-016-4975-x
Zayan NE, Meara MP, Schwartz JS, Narula VK (2019) A direct comparison of robotic and laparoscopic hernia repair: patient-reported outcomes and cost analysis. Hernia. https://doi.org/10.1007/s10029-019-01943-7
Abdelmoaty W, Dunst C, Neighorn C, Sanstrom L, Hammill C (2019) Robotic-assisted versus laparoscopic unilateral inguinal hernia repair: a comprehensive cost analysis. Surg Endosc 33:3436–3443. https://doi.org/10.1007/s00464-018-06606-9
Khoraki J, Gomez P, Mazzini G, Pessoa B, Browning M, Aquilina G, Salluzzo J, Wolfe L, Campos G (2019) Perioperative outcomes and cost of robotic-assisted versus laparoscopic inguinal hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-019-07128-8
Acknowledgements
Dr. Ray Joehl critically reviewed the study proposal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Linn reports personal fees from WL Gore and Associates, outside the submitted work; Dr. Ujiki reports personal fees from Boston, Olympus and Cook, personal fees from Gore and Scientific, outside the submitted work. Beau Forester, Dr. Attaar, Kara Donovan, Kristine Kuchta, Dr. Denham, Dr. Haggerty, JoAnn Carbray have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Forester, B., Attaar, M., Donovan, K. et al. Short-term quality of life comparison of laparoscopic, open, and robotic incisional hernia repairs. Surg Endosc 35, 2781–2788 (2021). https://doi.org/10.1007/s00464-020-07711-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07711-4