Abstract
Purpose
In this retrospective, non-randomized study, we compared the quality of life (QOL) of patients who underwent laparoscopic ventral and incisional hernia repair (LVIHR) with fascial defect closure or non-defect closure and examined the factors associated with the QOL after LVIHR.
Methods
Between February 2013 and 2016, we conducted a single-center, follow-up study of 33 consecutive midline hernia patients who underwent LVIHR. Overall, 14 cases underwent intraperitoneal onlay mesh repair (IPOM), and 19 underwent IPOM with fascial defect closure (IPOM-plus). Patients were interviewed using the 36-item Short Form Health Survey (SF-36) to assess their pre- and postoperative QOL (at 1, 3, 6, and 12 months after surgery). The QOL, as assessed by the SF-36, was compared before and at 1 year after surgery, and the risk factors associated with the QOL were examined.
Results
Overall, scores for 5 of the 8 domains and 1 of the 3 components of SF-36 had improved by 1 year after surgery compared with before surgery. The scores for the SF-36 domains and components at 1 year post-surgery were comparable in patients undergoing IPOM or IPOM-plus. Obesity, operative time, hernia size, and mesh size were factors correlated with the QOL.
Conclusions
LVIHR improved the QOL, regardless of defect closure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic surgery for ventral and incisional hernia repair (LVIHR) has been extensively used since it was first reported by Leblanc in 1993 [1]. The two most popular approaches to LVIHR are intraperitoneal onlay mesh repair (IPOM) and IPOM with fascial defect closure (IPOM-plus).
Improving the quality of life (QOL) of patients after LVIHR is crucial because ventral and incisional hernias can be primary or secondary benign disease. IPOM-plus appears to produce a more favorable surgical outcome than IPOM in terms of complications [2]. However, the QOL after IPOM and IPOM-plus remains unclear.
In this study, we assessed the QOL of patients who underwent LVIHR with IPOM or IPOM-plus using a universal questionnaire: the 36-item Short Form Health Survey (SF-36). We also examined factors associated with the QOL after surgery.
Methods
Patients
In this retrospective, non-randomized, single-center follow-up study, 33 consecutive patients with midline incisional hernia (maximum width, 10 cm) who underwent LVIHR with IPOM or IPOM-plus between February 2013 and 2016 were included.
For all patients in this study, indications for surgery included symptoms that reduced the QOL in daily life, such as pain, abdominal discomfort, and constipation. There were no cases of emergency surgery, such as for intestinal obstruction or peritonitis.
Overall, 14 patients underwent IPOM between February 2013 and July 2015, whereas 19 underwent IPOM-plus between August 2015 and February 2016. All surgeries were performed by the same surgeon at a single institution.
Questionnaire
Using SF-36, patients were interviewed to assess their health-related QOL pre- and post-operation (at 1, 3, 6, and 12 months). SF-36 includes the following eight domains: Physical Functioning (PF), Role-Physical (RP), Bodily Pain (BP), General Health Perception (GH), Vitality (VT), Social Functioning (SF), Role-Emotional (RE), and Mental Health (MH). The mean score of each SF-36 domain is defined as 50.0 in healthy Japanese individuals [3, 4]. Higher scores represent a better function/outcome. One summary score of SF-36 (role-social component score [RCS]) is used in Japan, in addition to two original summary scores (physical component score [PCS] and mental component score [MCS]) [4]. The QOL, as assessed by the SF-36 pre- and post-operation (at 1, 3, 6, and 12 months), was compared between patients who underwent LVIHR with IPOM and IPOM-plus.
Follow-up
All patients were scheduled for an outpatient follow-up visit at our institution at 1, 3, 6, and 12 months after surgery to assess morbidity and predefined surgical and medical complications. The patients underwent ultrasonography or computed tomography to examine abdominal wall complications, particularly seroma formation and mesh bulging.
Risk factors
Risk factors, including obesity (body mass index [BMI] > 25 kg/m2), chronic occlusive pulmonary disease (COPD), immunosuppressed state in patients receiving steroid medications or those suffering from collagen disease, diabetes mellitus (DM), walking difficulty (because of knee pain, backache, or cardiopulmonary dysfunction), operative time, hernia size, mesh size, seroma formation, and SF-36 scores before and at 1 year after surgery, were analyzed. Seroma formation assessed at 1, 3, 6, and 12 months after surgery was compared between patients who underwent LVIHR with IPOM and IPOM-plus.
Complications
Complications after LVIHR, such as recurrence, mesh bulging, chronic pain, and seroma formation, were recorded. The Clavien–Dindo classification of each surgical complication was evaluated. Patients were classified as having chronic pain when they experienced continuous pain for 3 months or longer, and seroma formation was defined as seroma requiring aspiration.
Surgery
LVIHR was performed as stated in this section. Under general epidural anesthesia, the entry point of the first 5-mm trocar was defined as Palmer’s point. Twelve- and 5-mm trocars were then inserted at the left lateral side of the abdomen. Of note, 1 or 2 additional 5-mm trocars were allowed to be inserted as necessary. After trocar insertion, adhesiolysis was performed to reveal the hernial defect. The intracorporeal measurement of the defect size was performed using low-pneumo pressure, and the defect location was carefully marked on the outside of the skin using a 23-gauge needle. Notably, these marks are extremely important, as when these are not precise, the location of mesh fixation is not precise, leading to the misalignment of the defect and mesh. After measuring the defect size, a mesh was prepared using a 5-cm overlap of the defect. IPOM-plus was used to close the defect using a reverse U-shaped 2-cm seam on each side of the defect [5, 6]. Before inserting the mesh into the abdomen, the mesh was stitched with 2–4 threads at the center line to hitch and then rolled and inserted through the 12-mm trocar. After enrolling the mesh in the abdomen, an intraperitoneal hitch stitch was made using sutures but not tightened. Note that when the mesh is at the exact location, the edge of the mesh can be circularly tacked at 1.5–2.0 cm around the defect using absorbable tacks (AbsorbaTack; Medtronic, MN USA, or SorbaFix; BARD, RI, USA). The 2–4 threads were then tightened to hitch the mesh. Finally, the muscle fascia and skin were tightened using a 12-mm trocar.
Statistical analyses
A retrospective chart review was performed to evaluate all data. The SPSS Statistics software program, version 23 (IBM SPSS, Tokyo, Japan), was used for all analyses. Fisher’s exact test was used to compare demographics of patients. The SF-36 scores and seroma formation of patients undergoing LVIHR with IPOM or IPOM-plus before and after surgery were assessed using a paired t test and t test, respectively. The association of the QOL with risk factors was assessed using Pearson’s correlation coefficients.
Ethics
The institutional review board approved the study, and written informed consent was obtained from each patient for the publication of this article.
Results
A total of 33 patients were included in this study (14 in IPOM and 19 in IPOM-plus). More patients underwent LVIHR with IPOM-plus than with IPOM. Furthermore, patients who underwent LVIHR with IPOM more frequently showed a BMI > 25 kg/m2, COPD, and DM than those who underwent LVIHR with IPOM-plus. The operative time was shorter using IPOM than using IPOM-plus. The sex, age, immunosuppressed state, walking difficulty, hernia size, and mesh size were not significantly different between the two groups (Table 1).
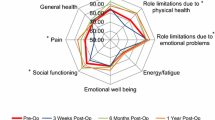
No recurrence of complications occurred after surgery. Seroma formation was observed following LVIHR with IPOM, while chronic pain was observed following LVIHR with IPOM-plus. In all patients, the scores for 5 (PF, RP, GH, SF, and RE) of the 8 domains and 1 (RS) of the 3 components of SF-36 significantly improved at 1 year after LVIHR, while scores for the remaining domains and components declined (Table 2). At 1 year after LVIHR, no significant differences were observed in the SF-36 scores between IPOM and IPOM-plus (Fig. 1). Seromas disappeared faster in IPOM-plus than in IPOM (mean duration 2.9 ± 2.1 vs. 4.3 ± 2.2 months; P = 0.04). The hernia size was correlated with scores for the PF, RP, GH, SF, and RE domains of SF-36 before and 1 year after surgery; operative time correlated with scores for the PF; and mesh size correlated with scores for the SF, RE, RCS; obesity was correlated with MCS and RCS (Table 3). Defect closure and seroma formation did not affect the SF-36 scores.
No significant differences were noted in the SF-36 domain and component scores before and at 1 year after LVIHR with IPOM and IPOM-plus. SF-36 36-item Short Form Health Survey, LVIHR laparoscopic ventral and incisional hernia repair, IPOM intraperitoneal onlay mesh repair, IPOM-plus IPOM with fascial defect closure, PF physical functioning, RP role-physical, BP bodily pain, GH general health perception, VT vitality, SF social functioning, RE role-emotional, MH mental health, PCS Physical Component Summary, MCS Mental Component Summary, RCS Role-Social Component Summary, PreOpe pre-operation, M months
No serious complications were detected in any cases. One patient in the IPOM group developed chronic pain of Clavien–Dindo Grade II, and one patient in the IPOM-plus group exhibited seroma formation of Clavien–Dindo Grade I.
Discussion
Laparoscopic surgery for ventral and incisional hernia is a widely used technique [1]. LVIHR is associated with reduced complication and recurrence rates and an improved QOL compared with open ventral and incisional hernia repair [7]. In addition, IPOM-plus is frequently used in ventral and incisional hernia repair [5, 6, 8]. Most surgeons prefer IPOM-plus to achieve better outcomes and avoid complications, such as recurrence and mesh bulging; however, concerns remain regarding postoperative pain. The guidelines in the International Endohernia Society (IEHS) recommend that IPOM-plus be performed as Grade C for hernias of limited size and as Grade D to prevent seroma formation. The IEHS also stated that the IPOM-plus technique reduces the recurrence rate compared with classical IPOM (Level 3); closing hernia defects using IPOM-plus repair minimizes seroma incidence and prevents bulging, thereby reducing the patient’s discomfort (Level 4), and defect closure may lead to chronic pain (Level 4) [9]. The Society of American Gastrointestinal Endoscopic Surgeons (SAGE) guidelines states that the closure of hernia defects should be undertaken at the surgeon’s discretion, as theoretical advantages exist; however, this has not been conclusively proven by high-quality comparative studies, and further evidence is needed (weak recommendation) [10]. The IEHS and SAGE guidelines therefore do not strongly recommend closing defects.
Furthermore, these guidelines do not mention whether the QOL of IPOM-plus is better than that of IPOM. The QOL after LVIHR might be correlated with not only seroma, bulging, discomfort, and pain but also with the patient’s condition (obesity, COPD, immunosuppression, DM, and walking difficulty) and surgical factors (defect closure, operation time, hernia size, and mesh size). Therefore, it is crucial to identify any correlations between the QOL and SF-36 (as included pain score), patient and surgical factors, and seroma formation that might affect the QOL after surgery.
All patients who underwent LVIHR (IPOM or IPOM-plus) in our hospital showed significantly better outcomes in five domains and one component of the SF-36 at 1 year after surgery than before the surgery, and poor outcomes were not observed in any domain or component (Table 2).
In the present study, scores for the pain domain of SF-36 were not significantly different between IPOM and IPOM-plus. One patient in the IPOM-plus group appeared to experience increased pain due to tension and the use of a high number of sutures. However, no significant difference was found between the IPOM and IPOM-plus groups in terms of acute and chronic pain after surgery [7, 11]. Furthermore, the scores for the RP, BP, and VT domains at 1 month after surgery were lower in the IPOM-plus group than in the IPOM group (Fig. 1), suggesting that IPOM-plus might have a weaker effect on the QOL than IPOM at 1 month after surgery, although the underlying reasons for this remain unclear. No significant difference was noted in the SF-36 scores before and at 1, 3, 6, and 12 months after surgery when the baseline data were aligned and changes were compared. Serious complications did not occur in any cases, although one patient in the IPOM group experienced chronic pain, and one in the IPOM-plus group showed seroma formation.
Defect closure did not affect the SF-36 scores. The QOL and complications at 1 year after surgery appeared to be similar between the IPOM and IPOM-plus groups. Defect closure affected the disappearance of seroma. Obesity, operative time, hernia size, and mesh size were correlated with the SF-36 scores.
Regardless of the resulting QOL, surgeons tend to prefer surgeries likely to reduce the occurrence of complications, such as recurrence. In the present study, the QOL was not significantly different between the two groups. Therefore, surgeons may think in the following two ways: first, closure of the hernia defect is not necessary if the QOL or the complication rate is not affected by closure of the hernia defect. Second, there is a concept of closing the hernia defect with emphasis on the reduction of complications caused by closure of the hernia defect because the result of this study that does not change the QOL especially for pain. However, this aspect was not adequately explored in this study.
Limitations associated with this study include its retrospective nature, small sample size, different considerations for IPOM and IPOM-plus, and different backgrounds between the two groups (Table 1). A randomized controlled study using a large number of patients is warranted to further validate our findings.
In conclusion, no marked differences in the QOL or complications at 1 year post-surgery were observed in patients who underwent LVIHR with and without facial defect closure. In fact, the pain improved with fascial defect closure. Seroma disappeared faster with defect closure than without defect closure, but seroma formation was not correlated with the QOL. Finally, LVIHR improved the QOL, regardless of defect closure.
References
LeBlanc KA, Booth WV. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: preliminary findings. Surg Laparosc Endosc. 1993;3:39–41.
Suwa K, Okamoto T, Yanaga K. Closure versus non-closure of fascial defects in laparoscopic ventral and incisional hernia repairs: a review of the literature. Surg Today. 2016;46:764–73.
Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51:1037–44.
Fukuhara S, Ware JE Jr, Kosinski M, Wada S, Gandek B. Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol. 1998;51:1045–53.
Franklin ME Jr, Gonzalez JJ Jr, Glass JL, Manjarrez A. Laparoscopic ventral and incisional hernia repair: an 11-year experience. Hernia. 2004;8:23–7.
Banerjee A, Beck C, Narula VK, Linn J, Noria S, Zagol B, et al. Laparoscopic ventral hernia repair: does primary repair in addition to placement of mesh decrease recurrence? Surg Endosc. 2012;26:1264–8.
Rogmark P, Petersson U, Bringman S, Eklund A, Ezra E, Sevonius D, et al. Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg. 2013;258:37–45.
Chelala E, Thoma M, Tatete B, Lemye AC, Dessily M, Alle JL. The suturing concept for laparoscopic mesh fixation in ventral and incisional hernia repair: mid-term analysis of 400 cases. Surg Endosc. 2007;21:391–5.
Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society [IEHS])—part 2. Surg Endosc. 2014;28:353–79.
Earle D, Roth JS, Saber A, Haggerty S, Bradley JF, Fanelli R, et al. SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc. 2016;30:3163–83.
Clapp ML, Hicks SC, Awad SS, Liang MK. Trans-cutaneous closure of central defects (TCCD) in laparoscopic ventral hernia repairs (LVHR). World J Surg. 2013;37:42–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saijo, F., Tokumura, H., Narushima, Y. et al. The quality of life after laparoscopic ventral and incisional hernia repair with closure and non-closure of fascial defect. Surg Today 49, 942–947 (2019). https://doi.org/10.1007/s00595-019-01834-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-019-01834-5