Abstract
Background
Incisional hernia (IH) is a frequent occurrence following open surgery for Crohn’s disease (CD). This study compares the IH rates of patients with CD undergoing open versus laparoscopic bowel resection.
Methods
Seven hundred and fifty patients with CD operated by the authors at the Mount Sinai Medical Center, New York, USA, were reviewed from a prospectively maintained surgical database. Five hundred patients with Crohn’s disease undergoing open surgery were compared to 250 patients undergoing laparoscopic bowel resection.
Results
The mean duration of follow-up in the study population was 6.8 years. Patients undergoing open surgery had a significantly higher age at onset of disease, age at surgery, longer duration of disease, lower serum albumin, history of multiple previous resections, were more likely to be on steroids, needed more blood transfusions, and had an increased necessity for an ileostomy during resection. Nevertheless, the incidence of IH at 36 months was nearly identical in both groups (10.8 vs. 8.4% for open vs laparoscopic). 16% of the patients in the laparoscopic group (range: 7–20%) required conversion to open surgery. Patients undergoing laparoscopic resection that required conversion to open surgery had the highest IH rate at 18%. There was a significant correlation between IH and the length of the midline vertical extraction incision. Patients undergoing laparoscopic resection with intracorporeal anastomosis and small transverse or trocar site extraction incisions had no IH.
Conclusions
A marked decrease or complete elimination of IH in patients with CD undergoing bowel resection may be possible using advanced laparoscopic techniques that require intra-abdominal anastomosis and use of the smallest transverse extraction incisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The surgical treatment of patients with inflammatory bowel disease (IBD) has undergone a dramatic revolution since the advent of minimally invasive laparoscopic surgery. Patients with Crohn’s disease (CD) with previous abdominal surgery and complicated disease often still require open surgery. Incisional hernia (IH) is a common occurrence following open surgery in CD and has been reported in the literature to be as high as 20% on long-term postoperative follow-up [1]. Laparoscopic bowel resection in CD may be performed with intracorporeal or extracorporeal anastomoses. Both methods in most instances will require an extraction incision. The smaller length of the extraction incision combined with a lower rate of postoperative wound infection when compared to a laparotomy incision would create the expectation of a potential lower incidence of IH [2]. Incisional hernia following laparoscopic bowel resection for CD has not been well studied and comparison with a large group undergoing open surgery was not previously available [3, 4]. This study reviews a large series of patients with CD undergoing bowel resection using open and laparoscopic technique and compares the incidence and factors correlating with the development of IH.
Materials and methods
Seven hundred and fifty patients with CD operated by the authors at the Mount Sinai Medical Center were reviewed from a prospectively maintained surgical database. Five hundred patients who underwent open bowel resection operated between January 1976 and December 2014 were compared to 250 patients undergoing laparoscopic bowel resection operated between February 2006 and December 2015. The duration of follow-up of the patients was calculated from date of surgery to the date of last postoperative visit. IH was defined as presence of a hernia in the midline incision, ileostomy closure, or laparoscopic extraction site developing within 36 months of the index surgery. IH was diagnosed by clinical examination, radiologic findings, and/or operative report. There were no trocar site hernias in this study. Parastomal hernias were excluded from the analysis. Preoperative clinical variables including age at diagnosis of CD, age at surgery, duration of disease, gender, smoking status, body mass index (BMI), number of previous bowel resections, hemoglobin, albumin, preoperative steroids and/or immunosuppressive medications including biologicals given within 6 weeks of surgery were included in the statistical analysis. Indications for surgery, need for ileostomy, postoperative length of hospital stay, complications, blood transfusion and wound infection were studied. Indication for surgery was classified as perforating and non-perforating disease as described by Greenstein et al. [5]. Postoperative complications were classified into septic and non-septic. Septic complications were defined as those related to infectious causes. Non-septic complications comprised intestinal obstruction, prolonged ileus, cardiac dysfunction, and other non-infectious causes. Wound infection was defined as presence of purulent drainage from the wound.
Patients undergoing open surgery had a vertical midline incision and closure of the wound was performed using absorbable running polydioxanone (PDS) or non-absorbable polypropylene sutures. Ileostomy sites were usually closed with absorbable sutures using transverse incisions in the right lower quadrant. In the laparoscopic group, the extraction site was most often through a midline vertical incision. In some instances, a transverse Pfannenstiel or peri-umbilical incision was used. A wound protector was used in all laparoscopic cases and closure of these incisions was similar to that of open cases. The length of the extraction site was recorded in centimeters. Laparoscopic surgery was analyzed as intention to treat. Patients undergoing laparoscopic surgery that required conversion to open surgery were defined as indicated in the operative report that the incision was extended beyond that required for laparoscopic surgery and the procedure was completed using standard open techniques. Patients requiring conversion to open surgery were analyzed under the laparoscopic group.
Descriptive statistics were performed using the IBM SPSS software [6]. Categorical variables were analysed using χ 2 and Fischer’s exact test. Unpaired Student t test was employed to compare continuous variables, and variables with a p value of less than 0.1 were used as independent variables in a Cox proportional hazard regression model. Independent factors were reported with hazard ratio (HR) and 95% confidence intervals (CI). Statistical significance was assumed when the obtained p-value was <0.05. Kaplan–Meier curves were used to study the time to development of IH and were stratified by the surgical approach. The data analysis was performed collectively for the entire population and separately for the two groups.
Results
Seven hundred and fifty patients with Crohn’s disease undergoing bowel resection were studied. Five hundred of these underwent open bowel resection and 250 had laparoscopic bowel resection. The mean duration of follow-up in the study population was 6.8 years. Patients undergoing open surgery had a significantly higher age at onset of disease, age at surgery, and longer duration of disease (See Table 1). The mean preoperative serum albumin was significantly higher in patients undergoing laparoscopic versus open surgery (3.8 vs. 3.6, p < 0.01). Patients undergoing open surgery were more likely to be on steroids, while those undergoing laparoscopic surgery were more likely to be on biologic and other immunosuppressive agents. These differences were significant (See Table 2). There was no significant difference in gender, indication for surgery, BMI, smoking status, and preoperative anemia.
Patients undergoing open resection were significantly more likely to have had multiple previous resections than laparoscopic patients (p < 0.01). The intraoperative need for an ileostomy was also higher in the open group (23 vs. 4%, p < 0.01). The necessity for perioperative blood transfusion was significantly higher in the patients undergoing open surgery (12 vs. 3%, p < 0.01). Mean length of stay was significantly shorter in the laparoscopic group (9 vs. 5 days, p < 0.01). The overall postoperative complication rates, including septic and non-septic complications, were similar in both groups (21 vs. 20%). The rate of wound infection was twice as high in the open group, but this difference did not reach statistical significance (8 vs. 4%, p = 0.068).
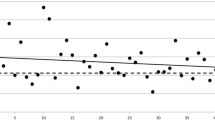
The overall incidence of IH in the study population is 6% at 12 months, 8% at 24 months, and 10% at the end of 36 months (See Fig. 1). There was no significant difference in the incidence of IH between patients undergoing open versus laparoscopic surgery at the end of 12, 24, and 36 months (See Fig. 2). Univariate analysis of the entire study population showed that the following factors correlate significantly with the development of IH: age at onset of CD, duration of disease, age at surgery, male gender, BMI, smoking, number of previous bowel resections, postoperative stay, complications (septic and non-septic) and wound infection (See Tables 3 and 4). Multivariate analysis shows that smoking and BMI are independent variables correlating with the development of IH in this study population (See Table 5).
Subset analysis of patients undergoing laparoscopic surgery reveals that 41 patients (16%) required conversion to open surgery. Patients requiring conversion were significantly older at the time of surgery (39 vs. 34 years, p < 0.05), were more likely to have multiple previous resections (p < 0.01), had a higher rate of postoperative complications (37 vs. 17%, p < 0.05) and a longer postoperative length of stay (5.6 vs. 4.7 days, p < 0.05, See Table 6). When indications for surgery were reviewed, patients requiring conversion were more likely to be operated for perforating disease (fistula and abscess) than patients that were completed laparoscopically (54 vs. 37%, p = 0.055). The incidence of IH at 36 months for patients requiring conversion was 17% compared to 7% in patients having laparoscopic surgery without conversion (p = 0.057). The conversion rate ranged from 7 to 20% when stratified by the surgeon (p < 0.05).
The mean length of the extraction incision in laparoscopic patients is 3.3 cm. Analysis of the type of extraction incision showed that 37 patients had a transverse or Pfannenstiel incisions while 213 had vertical midline incisions. There were no IH in patients that had a Pfannenstiel or other transverse extraction incisions, while those with vertical extraction incisions had an IH rate of 10% at 36 months (p = 0.051). Patients with a midline vertical extraction incision of 4 cm or longer had a significantly higher IH rate (18 vs. 5%, p < 0.05). Thirty-eight patients (15%) in this series had an intracorporeal anastomosis, and the specimen was brought out through a slightly enlarged trocar site or Pfannenstiel incision. None of these patients developed an IH during the duration of the study (See Table 7). Multivariate analysis of the laparoscopic patients shows that the age at surgery, BMI, length of the midline vertical extraction incision, and conversion to open correlate significantly with development of IH (See Table 8).
Discussion
In the present study, follow-up of patients with CD undergoing open and laparoscopic bowel resection shows a nearly identical incidence of IH at 36 months (10.8 vs. 8.4%). Patients undergoing open surgery are more likely to be older at onset of disease and at surgery. The duration of disease is also significantly longer. They have a lower serum albumin, are more likely to be on steroids, and require more blood transfusions. They are also more likely to have had previous surgery, have a higher need for ileostomy and a significantly higher rate of wound infection, yet the incidence of IH remain similar between the two groups. Several studies comparing open to laparoscopic bowel resection have also reported no significant difference in rates of IH between the two groups [7, 8]. The resections in these studies were predominantly done for treatment of colon cancer. Randomized controlled trials of laparoscopic versus open surgery in patients with CD undergoing bowel resection and in patients with Ulcerative colitis (UC) undergoing ileoanal pouch procedures showed no significant difference in the rate of IH [3, 9]. In a study by Eshuis et al. [4], the incidence of IH for open bowel resection in CD was significantly higher than the previously listed studies; however, the results for laparoscopic IH remain essentially similar as in the present study at 7%. We have previously reported that the incidence of IH after open resection continues to increase with time after surgery and at 15 years of follow-up reaches 20% [1]. The present study is limited to a follow-up of 36 months which accounts for the overall IH rate of 10%.
Multivariate analysis of our patients reveals that smoking and BMI are independent factors that correlate with the development of IH. In addition, postoperative wound infection, male gender, and age at surgery approach statistical significance. Multivariate analysis of the laparoscopic subset shows that the age at surgery, BMI, length of the extraction incision, and conversion to open surgery are independent factors that correlate with the development of IH. Postoperative wound infection is not statistically significant in this subset. These findings are similar to those reported by Llaguna et al., Sadava et al., and Julliard et al. [10,11,12].
Laparoscopic bowel resection in most instances requires an extraction incision of variable length, and location. The smallest extraction site can be a 10 mm periumbilical trocar site which is enlarged to allow removal of the specimen. Erdas et al. [13] reported that the incidence of IH in 10 mm umbilical trocar extraction sites for laparoscopic cholecystectomy can be as high as 4%. In most cases in this series, the extraction incision was a vertical incision located in the midline, often in a periumbilical location and the incidence of IH was 10%. This number is identical to the IH rate of the larger incisions in the open cases. Surgical bowel resection for Crohn’s disease can be complicated especially in patients who have had multiple previous surgeries. Forty-one patients of our laparoscopic group (16%) required conversion to open surgery. This rate is similar to that reported by Mino et al. [14] of 14.4% in a large series of patients with CD undergoing laparoscopic resection. We found in the present series that the conversion rate also varied significantly when stratified by surgeon. Univariate analysis comparing patients requiring conversion to those who did not revealed that conversion was associated with a higher postoperative complication rate than both laparoscopic and open surgery. The incidence of IH at 36 months in the converted group rose to 17% which is higher than the rate of IH following open surgery (10.8%).
Patients with midline vertical extraction incisions of 4 cm or greater in this series were found to have a significantly higher incidence of IH (18 vs. 5%, p < 0.05). In a study by Benlice et al. [15], the length of incision was found to correlate with IH and the risk increased for each centimeter increment of the extraction incision. Further analysis of the extraction site in our study reveals that none of the 37 patients with a small transverse extraction incision (Pfannenstiel or periumbilical trocar site) developed IH. This finding was corroborated by DeSouza, Benlice, Lee and Singh [2, 15,16,17]. Very small extraction incisions located in a remote location from the site of the anastomosis will often require performance of an intracoporeal anastomosis. We found that none of the 38 patients in this series who had an intracorporeal anastomosis developed IH. All these patients had either a very small Pfannenstiel incision or periumbilical trocar extraction site. Shapiro et al. [18] in a study of 191 patients with colon cancer undergoing laparoscopic right hemicolectomy comparing intracorporeal versus extracorporeal anastomosis showed that intracorporeal anastomosis with a Pfannenstiel extraction incision had an IH rate of 2.2% while patients having laparoscopic resection with extracorporeal anastomosis via a periumbilical incision had a significantly higher IH rate of 17%. In a large meta-analysis of 14 studies involving 1717 patients, Ricci et al. [19] also compared intracorporeal vs extracorporeal anastomosis in laparoscopic right hemicolectomy. The rate of IH was significantly lower in patients undergoing an intracorporeal anastomosis (2.3 vs. 13.7%, p < 0.05) [19]. In our series, laparoscopic bowel resection for Crohn’s disease was most often performed using extracorporeal anastomosis which usually requires a larger extraction incision closer to the resection site. Also, intracoporeal anastomosis is performed under direct vision and is less likely to result in a twisted anastomosis [20,21,22]. However, the degree of difficulty in performing an intracorporeal anastomosis is significantly increased over extracorporeal anastomosis [23].
In conclusion, in order to minimize IH rates, laparoscopic bowel resection in patients with CD requires elimination or reduction in length of the extraction incision and use of small, transverse, possibly Pfannenstiel incisions. In some cases such as total proctocolectomy and abdominoperineal resection, the bowel may be extracted perineally without an abdominal incision. In a few instances, surgeons have also used natural orifice extraction sites such as trans-rectal or trans-vaginal, but these cases are few and require further study [24, 25]. Robotic surgery has also been used to facilitate intracorporeal anastomosis, and in a study by Morpugo et al. [26] comparing robotic intracorporeal to laparoscopic extracorporeal anastomosis, none of the patients in the robotic group developed IH while in the laparoscopic group the incidence was 8%. A marked decrease or complete elimination of IH in patients with CD undergoing bowel resection may be possible using advanced laparoscopic techniques requiring intra-abdominal anastomosis and the smallest transverse extraction incisions performed by experienced colorectal surgeons.
References
Heimann TM, Swaminathan S, Greenstein AJ, Steinhagen RM (2017) Incidence and factors correlating with incisional hernia following open bowel resection in patients with inflammatory bowel disease: a review of 1000 patients. Ann Surg. doi:10.1097/SLA0000000000002120
DeSouza A, Domajnko B, Park J, Marecik S, Prasad L, Abcarian H (2011) Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc 25:1031–1036
Stocchi L, Milsom JW, Fazio VW (2008) Long-term outcomes of laparoscopic versus open ileocolic resection for Crohn’s disease: follow-up of a prospective randomized trial. Surgery 144:622–627
Eshuis EJ, Slors JF, Stokkers PC, Sprangers MA, Ubbink DT, Cuesta MA, Pierik EG, Bemelman WA (2010) Long-term outcomes following laparoscopically assisted versus open ileocolic resection for Crohn’s disease. Br J Surg 97:563–568
Greenstein AJ, Lachman P, Sachar DB, Springhorn J, Heimann T, Janowitz HD, Aufses AH Jr (1988) Perforating and non-perforating indications for repeated operations in Crohn’s disease: evidence for two clinical forms. Gut 29:588–592
IBM SPSS statistical package. Version 20. www. ibm.com/analytics/us/en/technology/spss/. Accessed on 31th January 2017
Ihedioha U, Mackay G, Leung E, Molloy RG, O’ Dwyer PJ (2008) Laparoscopic colorectal resection does not reduce incisional hernia rates when compared with open colorectal resection. Surg Endosc 22:689–692
Pecorelli N, Amodeo S, Frasson M, Vignali A, Zuliani W, Braga M (2016) Ten year outcomes following laparoscopic colorectal resection: results of a randomized controlled trial. Int J Colorectal Dis 31:1283–1290
Benlice C, Stocchi L, Costedio M, Gorgun E, Hull T, Kessler H, Remzi FH (2015) Laparoscopic IPAA is not associated with decreased rates of incisional hernia and small-bowel obstruction when compared with open technique: long-term follow-up of a case-matched study. Dis Colon Rectum 58:314–320
Llaguna OH, Avgerinos DV, Lugo JZ, Matatov T, Abbadessa B, Martz JE, Leitman IM (2010) Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus open colon resections. Am J Surg 200:265–269
Sadava EE, Kerman Cabo J, Carballo FH, Bun ME, Rotholtz NA (2014) Incisional hernia after laparoscopic colorectal surgery. Is there any factor associated? Surg Endosc 28:3421–3424
Julliard O, Hauters P, Possoz J, Malvaux P, Landenne J, Gherardi D (2016) Incisional hernia after single incision laparoscopic cholecystectomy: incidence and predictive factors. Surg Endosc 30:4539–4543
Erdas E, Dazzi C, Secchi F, Aresu S, Pitzalis A, Barbarossa M, Garau A, Murgia A, Contu P, Licheri S, Pomata M, Farina G (2012) Incidence and risk factors for trocar site hernia following laparoscopic cholecystectomy: a long-term follow-up study. Hernia 16:431–437
Mino JS, Gandhi NS, Stocchi LL, Baker ME, Liu X, Remzi FH, Monteiro R, Vogel JD (2015) Preoperative risk factors and radiographic findings predictive of laparoscopic conversion to open procedures in Crohn’s disease. J Gastrointestinal Surg 19:1007–1014
Benlice C, Stocchi L, Costedio MM, Gorgun E, Kessler H (2016) Impact of specific extraction-site location on the risk of incisional hernia after laparoscopic colorectal resection. Dis Colon Rectum 59:743–750
Lee L, Mappin-Kasirer B, Sender Liberman A, Stein B, Charlebois P, Vassiliou M, Fried GM, Feldman LS (2012) High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 26:3180–3185
Singh R, Omiccioli A, Hegge S, Mckinley C (2008) Does the extraction site location in laparoscopic colorectal surgery have an impact on incisional hernia rates? Surg Endosc 22:2596–2600
Shapiro R, Keler U, Segev L, Sarna S, Hatib K, Hazzan D (2016) Laparoscopic right hemicolectomy with intracorporeal anastomosis: short and long-term benefits in comparison with extracorporeal anastomosis. Surg Endosc 30:3823–3829
Ricci C, Casadei R, Alagna V, Zani E, Taffurelli G, Pacilio CA, Minni F (2016) A critical and comprehensive systematic review and meta-analysis of studies comparing intracorporeal and extracorporeal anastomosis in laparoscopic right hemicolectomy. Langenbecks Arch Surg. doi:10.1007/s00423-016-1509-x
Nguyen SQ, Teitelbaum E, Sabnis AA, Bonaccorso A, Tabrizian P, Salky B (2009) Laparoscopic resection for Crohn’s disease: an experience with 335 cases. Surg Endosc 23:2380–2384
Grams J, Tong W, Greenstein AJ, Salky B (2010) Comparison of intracorporeal versus extracorporeal anastomosis in laparoscopic assisted hemicolectomy. Surg Endosc 24:1886–1891
Hellan M, Anderson C, Pigazzi A (2009) Extracorporeal versus intracorporeal anastomosis for laparoscopic right hemicolectomy. JSLS 13:312–317
Jamali FR, Soweid AM, Dimassi H, Bailey C, Leroy J, Marescau J (2008) Evaluating the degree of difficulty of laparoscopic colorectal surgery. Arch Surg 143:262–267
Gardenbroek TJ, Eshuis EJ, van Acker GJ, Tanis PJ, Bemelman WA (2012) Alternative specimen extraction techniques after laparoscopic emergency colectomy in inflammatory bowel disease. Surg Endosc 26:408–412
Kayaalp C, Yagci MA (2015) Laparoscopic right colon resection with transvaginal extraction: a systematic review of 90 cases. Surg Laparosc Endosc Percutan Tech 25:384–391
Morpugo E, Contardo T, Molaro R, Zerbinati A, Orsini C, D’Annibale A (2013) Robotic assisted intracorporeal anastomosis versus extracorporeal anastomosis in laparoscopic right hemicolectomy for cancer: a case control study. J Laparoendosc Adv Surg Tech 23:414–417
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Tomas M. Heimann, Santosh Swaminathan, Adrian J. Greenstein, Alexander J. Greenstein, Sergey Khaitov, Randolph M. Steinhagen, Barry A. Salky have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Heimann, T.M., Swaminathan, S., Greenstein, A.J. et al. Can laparoscopic surgery prevent incisional hernia in patients with Crohn’s disease: a comparison study of 750 patients undergoing open and laparoscopic bowel resection. Surg Endosc 31, 5201–5208 (2017). https://doi.org/10.1007/s00464-017-5588-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5588-8