Abstract
Introduction
Laparoscopy is accepted as a standard surgical approach for Crohn’s disease. However, the rate of conversion is high, ranging from 15 to 70 % depending on the population. There are also concerns that conversion results in worsened outcomes versus an initial open procedure.
Methods
This study evaluated preoperative radiographic findings to determine who is at increased risk of conversion and may therefore benefit from an initial open approach. A case-matched study included patients from 2004 to 2013 with preoperative CTE/MRE who underwent laparoscopic surgery converted to an open approach, and compared them to laparoscopically completed controls with similar age, same surgeon, and number of previous abdominal operations. Studies were reviewed by two blinded radiologists. Variables included abdominal AP diameter, amount of subcutaneous fat, peritoneal versus pelvic location of disease (greater or lesser hemipelvis or abdomen), intestinal location of disease (colon, TI, ileum, jejunum), and presence, length, and location of strictures, simple or complex fistula, phlegmon, or abscess. Conditional logistic regression evaluated relationships between radiographic variables and conversion. Twenty-seven patients meeting study criteria were compared with 81 controls.
Results
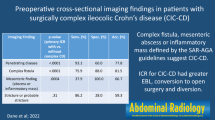
A negative association between conversion and disease in the left lesser pelvis was found (p = 0.019) and neared significance for left abdomen (p = 0.08). Positive correlations were found with pelvic fistulas (p = 0.003), complex fistulas (p = 0.017), and pelvic abscesses (p = 0.009) and neared significance for Society of Abdominal Radiology classification (p = 0.058).
Conclusion
Preoperative imaging in patients with Crohn’s disease can help in selecting the most suitable cases to approach laparoscopically and reduce conversion rates and should be evaluated in conjunction with other preoperative factors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease is an inflammatory bowel disorder affecting 400,000–600,000 individuals in the USA.1 In a chronic relapsing and remitting disease, 70–90 % of individuals will require surgery during their lifetime and 50 % of those will continue on multiple surgical procedures.2 Complications of the disease include bleeding, obstruction, fistulization, infection, and intractability.3 For most of these complications, surgical intervention with bowel resection is necessary. Previously, an open approach via a midline laparotomy incision was the most widely accepted method of performing the necessary bowel resections. While the advent of laparoscopic techniques eventually led to wide acceptance for oncologic resections, it was slow to find a foothold for Crohn’s due to the increased difficulty from the inflammatory nature of the disorder. Nonetheless, over time, several studies conclusively demonstrated the safety profile and decreased complications of laparoscopy in IBD and it is now considered as the approach of choice in patients requiring primary surgery.4–6 However, the rate of conversion to open surgery remains high, ranging from 5 % to as high as 70 %, but more typically in the 20–25 % range.4,7–9 The significant variation in these rates is due to several factors. These include a lack of consistency in the definition of conversion, with some authors defining it as an incision greater than 10 cm versus others defining it as an incision greater than 5 cm, and also due to the significant differences in patient populations. Some studies selected uncomplicated cases, while others included those with fistulas, abscesses, previous operations, etc. Additionally, there are concerns from the general colorectal literature that conversion from laparoscopic to open results in worsened outcomes compared even to those with an open operation as the initial approach.10–12 In addition, conversion results in increased resource utilization, operative costs, and operative times compared to either successful laparoscopic or open procedures, regardless of the indication for operation.13
Previous studies have evaluated preoperative and intraoperative findings predictive of conversion to an open procedure. These include male gender, a history of more than three acute episodes of Crohn’s disease, preoperative steroid use longer than 3 months, smoking, preoperative malnutrition, unexpected intraperitoneal abscess or fistula, previous abdominal surgical procedures, increased length of time between flares, and extracecal colonic disease.7,13 Regarding intraoperative findings, Alves et al. and Casillas et al. demonstrated that the most common reasons for conversion were the presence of a large inflammatory mass, adhesions, ileosigmoid fistula, pelvic abscess, unfavorable anatomy, inability to assess anatomy, failure to identify the ureter, and bleeding.7,14
These studies all involved relatively low sample sizes, and none sought to evaluate radiographic findings in predicting conversion. It is common practice to obtain preoperative imaging studies in the form of CT enterography (CTe) or MR enterography (MRe) to define the extent of disease and to plan surgery in patients with Crohn’s disease. To date, no studies have evaluated the findings of these imaging modalities as possible preoperative predictors of the need for conversion to an open procedure.
Therefore, the proposed study sought to determine if preoperative radiographic CT enterography or MR enterography could be used to predict which patients are at increased risk of conversion from laparoscopic to open surgery for Crohn’s disease and may thus benefit from an open approach from the onset.
Methods
A single-institution, retrospective case–control study was performed. The study period was 2003 to 2013 which coincides with the period in which CTe gained widespread use for the radiologic evaluation of Crohn’s disease in our institution. Data were extracted from a prospectively maintained departmental database and from the medical record. The study population was limited to patients with Crohn’s disease (ICD-9, 550.0-9) who underwent CTe or MRe within 3 months prior to a planned laparoscopic bowel resection for small or large bowel Crohn’s disease. Exclusion criteria were patients with Crohn’s disease who did not undergo preoperative CT enterography or MR enterography, incomplete imaging, incomplete documentation, or those who were treated non-operatively or with an initial open procedure.
Study patients whose procedures were converted from laparoscopic to open surgery were designated as the case group, while those patients who had their procedures completed laparoscopically were designated as the control group. Conversion was defined as the lengthening of any abdominal incision beyond what was planned to complete the operation laparoscopically. Exteriorization to remove the specimen, takedown of enterocutaneous fistulas as necessary, and completion of an anastomosis under direct vision were not considered as conversions. Cases were then frequency matched with controls in an approximately 1:3 ratio and matched by characteristics in descending order of importance by operating surgeon, number of previous abdominal surgeries, age within 5 years, and body mass index category (Fig. 1). Operative reports were subsequently reviewed to determine indication for surgery, duration of time between imaging and surgery, stage of operation at conversion, reason for conversion, preoperative and postoperative diagnoses, and final pathology results.
The preoperative CTe and MRe studies were reviewed by two dedicated, high-volume, gastrointestinal radiologists with 9 years (NSG) and 25 years (MEB) of experience, who were blinded to the operative findings. Multiple imaging variables were recorded. Location of the disease was defined as in the abdomen, greater pelvis, or lesser pelvis as well as laterality. Simple fistula denoted a single tract, while complex fistula was used if there were multiple enteroenteric fistulous tracts and/or associated abscesses. The greater pelvis was defined as the space enclosed by the pelvic girdle superiorly and the pelvic brim inferiorly, and the lesser pelvis was considered to be the space beneath the pelvic brim. Length of diseased bowel segment was recorded. Segment of bowel involved was recorded as the jejunum, ileum, terminal ileum, or colon. Intraperitoneal anterior–posterior dimension, extent of intraperitoneal fat as measured from the posterior aspect of the anterior abdominal wall to the closest site of the disease, and extent of subcutaneous fat as measured from the skin surface to the anterior abdominal wall at the site of maximal disease were all recorded. Penetration of the disease was assessed and classified as none, a sinus tract, simple fistula, complex fistula, or abscess/phlegmon. Based on the Society of Abdominal Radiology Classification for Crohn’s disease (work in progress), the radiologists gave an imaging classification: active inflammatory Crohn’s disease with or without luminal narrowing, mixed active inflammatory and fibrostenotic Crohn’s disease, and fibrostenotic Crohn’s disease. Penetrating disease was recorded as a modifier which could be added to any of the above categories.
Differences in baseline characteristics between converted and non-converted patients were examined with chi-square tests or t tests. Stepwise conditional regression analysis was then performed on the radiographic variables via univariate and multivariate analysis with entry level at p < 0.05 in order to determine odds ratios for their association with conversion to an open procedure, which can be interpreted as risk ratios in the face of adequate sampling of controls from the study base. No variables were entered into the multivariate model based on clinical considerations alone.
Results
In the study period, a total of 341 patients with Crohn’s disease underwent planned laparoscopic surgery. Of these, 187 had timely preoperative imaging. A total of 27 of these were converted to an open procedure (14.4 %). The remaining 160 were completed laparoscopically (85.6 %). Of these, 81 were selected as controls, were frequency matched by an operating surgeon, had a number of previous abdominal surgeries, aged within 5 years, and were body mass index categorized (Fig. 1).
Demographic variables were not significantly different between groups (Table 1). Patients in the case group had undergone surgeries by 13 different attending surgeons. The gender distribution of cases was not statistically significant, with 44 % females versus 56 % males. The average age of cases was 35.5 years. The average body mass index was 24.85. Fourteen of the 27 cases had never had a previous abdominal operation. Of the 13 patients with previous operations, ten were open procedures. Ten had undergone previous intestinal resections. Only four cases had undergone more than one abdominal operation or bowel resection.
The most common indications for operation were failure of medical management in 32 %10 and fistulas in 32 %.10 Stricture resulting in bowel obstruction was the indication for operation in 22 %.6 Inflammatory mass resulting in SIRS/sepsis was the indication in 11 %3 and perforation in 3 %1 (Fig. 2). In some cases, multiple indications for operation were present. Surgeries performed included ileocolic resection in 59 %,16 fistula repair in 15 %,4 sigmoidectomy in 11 %,3 total colectomy in 11 %,3 and small bowel resection in 3 %1 (Fig. 3). Conversion occurred due to large inflammatory mass in 26 %,7 dense adhesions in 26 %,7 uncertain anatomy in 19 %,5 abnormal anatomy in 15 %,4 fistula in 11 %,3 and pelvic abscess not amenable to percutaneous drainage in 3 %1 (Fig. 4). In some cases, multiple reasons for conversion were present. While the mean length of stay was higher in cases (9.15 days) versus controls (7.79 days), this was not statistically significantly different (p = 0.34). When evaluating radiographic findings, univariate analysis revealed multiple variables predictive of conversion (Table 2). These remained significant with multivariate logistic regression. These included sparing of disease in the left lesser pelvis (odds ratio (OR) = 4.276, confidence interval (CI) 1.182–15.471), the presence of an enterocutaneous fistula in the pelvis (OR = 3.808, CI 1.529–9.482) or complex enteroenteric fistula anywhere within the abdomen (OR = 3.012, CI 1.190–7.622), or the presence of a pelvic abscess (OR = 6.273, CI 2.175–18.094). Sparing of disease involving the left abdomen neared significance (OR = 0.280, CI 0.061–1.163) (Table 3). Segment of bowel involved (p = 0.30), the length of disease (p = 0.43), the intraperitoneal AP dimension (p = 0.57), and the extent of intraperitoneal fat and subcutaneous fat (p = 0.45) were not associated with conversion.
Discussion
Patients with complicated Crohn’s disease often require enteric resection. While this has traditionally been performed via open laparotomy, the laparoscopic approach has now become standard due to significant improvements in blood loss, length of stay, time to return of bowel function, fewer subsequent bowel obstructions, decreased pain, decreased overall morbidity, and functional recovery indices.6,15–21 Several studies have shown that colorectal patients with a laparoscopic procedure converted to open have longer operative courses, length of stay, increased resource utilization, and increased morbidity compared to both successfully completed laparoscopic procedures and those which were approached in an open fashion initially. For example, Slim et al. noted increased morbidity in 50 % of converted patients compared to 21 % in those who underwent initial laparotomy. While this likely represents an increased severity of the underlying disease, it is also likely that this is in part explained by the longer operating times.10,11,22–24
As such, numerous studies have looked at the risk factors associated with conversion, in an attempt to predict which cases will fail a laparoscopic approach. Preoperative patient-related factors found to be significant include smoking, ASA grade, BMI, and previous intestinal resections. Disease-related factors include fistula as an indication for operation, steroid administration within 3 months of surgery, extracecal colonic disease, and malnutrition. Operative factors include surgeon seniority, presence of fistula (especially ileosigmoid), pelvic abscess, phlegmon, dense adhesions, and bowel injury during adhesiolysis.3,25,9
To date, no studies have evaluated preoperative imaging findings and their correlation with conversion. As mentioned previously, Alves et al. and Brouquet et al. noted that the most common intraoperative findings causing conversion from laparoscopic to open included large inflammatory mass, adhesions, ileosigmoid fistula, and pelvic abscess.7,9 Our study mirrored these findings, indicating that preoperative imaging findings predict intraoperative findings well.
The patients in this study underwent multiple surgical procedures, with some encompassing multiple tasks including bowel resection with extracorporeal anastomosis, pelvic and abdominal washouts, ostomy formations, and hernia closures. While the heterogeneity of disease location and procedure may limit the generalizability of these findings, Crohn’s disease is itself a very heterogeneous process with unpredictable intraoperative findings. The findings in our study indicate that preoperative imaging can predict intraoperative findings which would lead to conversion. Knowing these ahead of time can improve preoperative planning as well as patient expectation and counseling.
The presence of an enteroenteric fistula as a risk factor for conversion to an open procedure is unsurprising. Fistulas tend to result in obliteration of surgical planes and significant inflammation, thus are much more often to be technically difficult. Oftentimes, fistulization to another abdominopelvic organ or to an area of bowel that is not planned for resection can be difficult to repair safely in a laparoscopic manner. The presence of a fistulous phlegmon was in fact the most common reason for conversion among the 27 patients in the case group of this study.
Adhesions that were dense enough such that the surgeon could not safely separate the bowel requiring resection from its surrounding structures was the second most common reason for conversion. This again illustrates the transmural inflammatory nature of the disease and the difficulty of managing this in a laparoscopic fashion.
Disease in the left pelvis demonstrating a decreased risk of conversion is an initially puzzling finding. The confidence interval is large, indicating that this may simply be a spurious finding due to the low sample size. However, it is more likely that this again represents the inflammatory nature of the disease. Disease confined to the rectum is less likely to result in enteroenteric fistulas with bowel or other organs outside of the planned area of resection. In other words, classic ileocolic Crohn’s disease may be at higher risk for conversion to an open procedure simply due to the higher risk of inflammatory spread.
There are some limitations to this study. Ultimately, the sample size remained small due to the fact that until recently, obtaining preoperative CTe or MRe was not standard practice. This limited our power to detect significant variables predictive of conversion from a laparoscopic to open operation. Additionally, 13 surgeons were included in this study with significant differences in a level of experience. While this is a strength in regards to generalizability, it adds a level of heterogeneity and potential confounding to the data. This was mitigated as much as possible by matching cases and controls by surgeon whenever possible. The retrospective, non-randomized nature of this study inevitably introduces the risk of bias or unobserved or anticipated confounding to the study. The study’s retrospective nature also introduces other limitations. In regards to reasons for conversion, adhesions were a common factor. Unfortunately, we were not able to obtain detailed intraoperative data on whether these were due to previous surgeries or the inflammation from the disease itself. That being said, of the seven patients who were converted due to adhesions, three had no previous surgeries and four had previous abdominal operations; thus, there was no statistically significant difference regarding previous surgery as a risk factor for conversion due to dense adhesions. Lastly, while several studies have mentioned concerns that conversion leads to poorer outcomes, there is the possibility that patients may benefit from starting a case laparoscopically, with the initial laparoscopic phase reducing the magnitude of subsequent open surgery. This has not been described extensively for Crohn’s operations, and a hybrid approach is not deliberately practiced at our institution. As such, it is difficult to ascertain after the fact from most operative reports whether or not the initial laparoscopic phase was of benefit, and thus, we are unable to comment on the significance of this.
Conclusion
Patients with Crohn’s disease are often faced with a future involving multiple abdominal operations. When possible, the benefits of laparoscopic intervention are clear, including improved cosmesis, less postoperative pain and length of hospitalization, quicker return to function, fewer intra-abdominal adhesions, and overall less morbidity. For uncomplicated ileocolic Crohn’s disease, several studies have shown that this is undoubtedly the approach of choice. With complicated or recurrent Crohn’s disease, the approach is less obvious, as conversion rates are high. Several studies have looked at preoperative and intraoperative risk factors which may influence the risk of conversion from a laparoscopic operation to an open operation. This is the first study which involves radiographic findings. While any of these imaging findings alone may not warrant perfunctory abandonment of a laparoscopic consideration, in combination with other preoperative risk factors, they may aid both in the decision-making of how a patient should be initially approached surgically and how they should be counseled preoperatively. Ultimately, the goal of research such as this will be to join these findings with other preoperative patient and disease-specific variables in order to form a predictive algorithm for conversion risk which may help direct a surgeon’s approach to individual patients.
References
Loftus EV, Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004 May;126(6):1504–17. PubMed
H. Hasegawa MW, H. Nishibori, K. Okabayashi, T. Hibi, and M. Kitajima. Laparoscopic surgery for recurrent Crohn’s disease. British Journal of Surgery. 2005 2005;90(8):4.
Schmidt CM, Talamini MA, Kaufman HS, Lilliemoe KD, Learn P, Bayless T. Laparoscopic surgery for Crohn’s disease: reasons for conversion. Annals of Surgery. 2001 Jun;233(6):733–9. PubMed Central PMCID: 1421315.
Spinelli A, Sacchi M, Bazzi P, Leone N, Danese S, Montorsi M. Laparoscopic surgery for recurrent Crohn’s disease. Gastroenterology Research and Practice. 2012;2012:381017. PubMed Central PMCID: 3255167.
Ludwig KA, Milsom JW, Church JM, Fazio VW. Preliminary experience with laparoscopic intestinal surgery for Crohn’s disease. American Journal of Surgery. 1996 Jan;171(1):52–5; discussion 5–6. PubMed
Milsom JW, Hammerhofer KA, Bohm B, Marcello P, Elson P, Fazio VW. Prospective, randomized trial comparing laparoscopic vs. conventional surgery for refractory ileocolic Crohn’s disease. Diseases of the Colon and Rectum. 2001 Jan;44(1):1–8; discussion 8−9. PubMed
Alves A, Panis Y, Bouhnik Y, Marceau C, Rouach Y, Lavergne-Slove A, et al. Factors that predict conversion in 69 consecutive patients undergoing laparoscopic ileocecal resection for Crohn’s disease: a prospective study. Diseases of the Colon and Rectum. 2005 Dec;48(12):2302–8. PubMed
Rottoli M, Bona S, Rosati R, Elmore U, Bianchi PP, Spinelli A, et al. Laparoscopic rectal resection for cancer: effects of conversion on short-term outcome and survival. Annals of Surgical Oncology. 2009 May;16(5):1279–86. PubMed
Brouquet A, Bretagnol F, Soprani A, Valleur P, Bouhnik Y, Panis Y. A laparoscopic approach to iterative ileocolonic resection for the recurrence of Crohn’s disease. Surgical Endoscopy. 2010 Apr;24(4):879–87. PubMed
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ. Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. The British Journal of Surgery. 2010 Nov;97(11):1638–45. PubMed
Slim K, Pezet D, Riff Y, Clark E, Chipponi J. High morbidity rate after converted laparoscopic colorectal surgery. The British Journal of Surgery. 1995 Oct;82(10):1406–8. PubMed
Heneghan HM, Martin ST, Kiran RP, Khoury W, Stocchi L, Remzi FH, et al. Laparoscopic colorectal surgery for obese patients: decreased conversions with the hand-assisted technique. Journal of Gastrointestinal Surgery: Official Journal of the Society for Surgery of the Alimentary Tract. 2013 Mar;17(3):548–54. PubMed
Young-Fadok TM, HallLong K, McConnell EJ, Gomez Rey G, Cabanela RL. Advantages of laparoscopic resection for ileocolic Crohn’s disease. Improved outcomes and reduced costs. Surgical Endoscopy. 2001 May;15(5):450–4. PubMed
Casillas S, Delaney CP, Senagore AJ, Brady K, Fazio VW. Does conversion of a laparoscopic colectomy adversely affect patient outcome? Diseases of the Colon and Rectum. 2004 Oct;47(10):1680–5. PubMed
Tan JJ, Tjandra JJ. Laparoscopic surgery for Crohn’s disease: a meta-analysis. Diseases of the Colon and Rectum. 2007 May;50(5):576–85. PubMed
Rosman AS, Melis M, Fichera A. Metaanalysis of trials comparing laparoscopic and open surgery for Crohn’s disease. Surgical Endoscopy. 2005 Dec;19(12):1549–55. PubMed
Tilney HS, Constantinides VA, Heriot AG, Nicolaou M, Athanasiou T, Ziprin P, et al. Comparison of laparoscopic and open ileocecal resection for Crohn’s disease: a metaanalysis. Surgical Endoscopy. 2006 Jul;20(7):1036–44. PubMed
Sardinha TC, Wexner SD. Laparoscopy for inflammatory bowel disease: pros and cons. World Journal of Surgery. 1998 Apr;22(4):370–4. PubMed
Benoist S, Panis Y, Beaufour A, Bouhnik Y, Matuchansky C, Valleur P. Laparoscopic ileocecal resection in Crohn’s disease: a case-matched comparison with open resection. Surgical Endoscopy. 2003 May;17(5):814–8. PubMed
Fichera A, Peng SL, Elisseou NM, Rubin MA, Hurst RD. Laparoscopy or conventional open surgery for patients with ileocolonic Crohn’s disease? A prospective study. Surgery. 2007 Oct;142(4):566–71; discussion 71 e1. PubMed
Maartense S, Dunker MS, Slors JF, Cuesta MA, Pierik EG, Gouma DJ, et al. Laparoscopic-assisted versus open ileocolic resection for Crohn’s disease: a randomized trial. Annals of Surgery. 2006 Feb;243(2):143–9; discussion 50–3. PubMed Central PMCID: 1448907.
Marusch F, Gastinger I, Schneider C, Scheidbach H, Konradt J, Bruch HP, et al. Importance of conversion for results obtained with laparoscopic colorectal surgery. Diseases of the Colon and Rectum. 2001 Feb;44(2):207–14; discussion 14–6. PubMed
Gervaz P, Pikarsky A, Utech M, Secic M, Efron J, Belin B, et al. Converted laparoscopic colorectal surgery. Surgical Endoscopy. 2001 Aug;15(8):827–32. PubMed
Schwandner O, Schiedeck TH, Bruch H. The role of conversion in laparoscopic colorectal surgery: Do predictive factors exist? Surgical Endoscopy. 1999 Feb;13(2):151–6. PubMed
Moorthy K, Shaul T, Foley RJ. Factors that predict conversion in patients undergoing laparoscopic surgery for Crohn’s disease. American Journal of Surgery. 2004 Jan;187(1):47–51. PubMed
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mino, J.S., Gandhi, N.S., Stocchi, L.L. et al. Preoperative Risk Factors and Radiographic Findings Predictive of Laparoscopic Conversion to Open Procedures in Crohn’s Disease. J Gastrointest Surg 19, 1007–1014 (2015). https://doi.org/10.1007/s11605-015-2802-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2802-7